PCI in the patient with refractory ventricular arrhythmia: Difference between revisions
m (Robot: Automated text replacement (-{{SIB}} +, -{{EH}} +, -{{EJ}} +, -{{Editor Help}} +, -{{Editor Join}} +)) |
m (Robot: Automated text replacement (-{{WikiDoc Cardiology Network Infobox}} +, -<references /> +{{reflist|2}}, -{{reflist}} +{{reflist|2}})) |
||
| Line 1: | Line 1: | ||
{{SI}} | {{SI}} | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | {{CMG}} | ||
Revision as of 20:34, 4 September 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Vijayalakshmi Kunadian MBBS MD MRCP [2];
Introduction
The majority of sudden cardiac deaths, which are predominantly due to acute coronary events, occur out of hospital. Rarely, resistant ventricular fibrillation, pulseless electrical activity (PEA) or asystole occur during cardiac catheterization. In such cases, the underlying coronary event should be immediately defined by coronary angiography and percutaneous coronary intervention performed as appropriate (PCI). Lethal ventricular arrhythmias have been reported to occur in 1.5-4% of patients undergoing PCI. In the Primary Angioplasty in Myocardial Infarction (PAMI) trial, ventricular arrhythmias occurred in 4.3% of patients 1.
Pathophysiology and clinical causes of arrhythmia
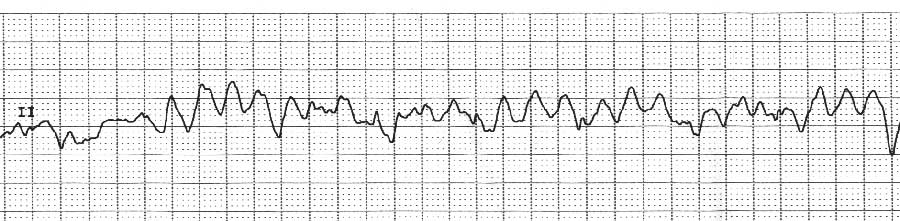
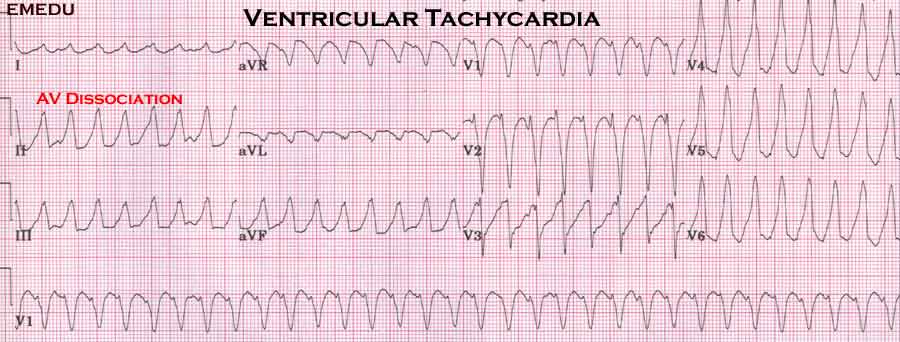
Left ventricular dysfunction and ongoing ischemia causes arrhythmia. There are several factors during angiography and intervention that result in sustained arrhythmias. These include the use of high osmolar contrast media, reperfusion injury, catheter manipulation, small caliber right coronary artery, presence of intracoronary thrombus and new ischemic events. Sudden obstruction of the coronary artery without preexisting coronary artery narrowing can be associated with a higher incidence of ventricular fibrillation (VF) compared with an obstruction occurring in association with preexisting stenosis. In the setting of an acute myocardial infarction, malignant arrhythmias can occur as a result of direct ischemia and hemodynamic compromise during PCI. The initiation and maintenance of sustained ventricular tachycardia (VT) and VF in the setting of myocardial ischemia and myocardial infarction (MI) result from very complex interaction of multiple factors. These include damaged myocardium, arrhythmia triggers, and various modulating factors. Ventricular arrhythmias in some patients have been thought to be related to reperfusion injury, occurring within a period of minutes after reperfusion has been achieved. The calcium paradox, the oxygen paradox, the production of oxygen-free radicals, and angiotensin II play an important role in the genesis of reperfusion injury and reperfusion arrhythmias. Although restoration of blood flow to the jeopardized myocardial salvage was established, reperfusion itself may lead to additional tissue injury beyond that generated by ischemia alone.
Predictors of malignant arrhythmias
Increased QTc dispersion may predict the risk for lethal ventricular arrhythmias during angioplasty. Henriques et al demonstrated that patients with VF during reperfusion therapy were older, more frequently female, less often had heart failure when compared to patients with VF before PCI. Patients with VF during PCI experienced more often angina prior to myocardial infarction and suffered more often from inferior MI compared to patients with VF before PCI 2. In the PAMI trial, step down logistic regression analysis identified current smoking, shorter time from symptom onset to emergency room presentation, lack of beta-blocker therapy in the emergency room, right coronary artery-related ST elevation myocardial infarction, and lower TIMI flow grades on admission as independent correlates of VT/VF 1.
Management
Sustained VT or VF with hemodynamic compromise should be terminated by synchronous DC shock. Use of medical therapy such as lidocaine and amiodarone can be beneficial. Intra-aortic balloon counterpulsation in selected patients can prevent serious ventricular arrhythmias in PCI. It can be used following primary PCI in high-risk patients in an attempt to improve outcomes by increasing coronary blood flow reserve, decreasing preload and afterload, and augmenting systemic pressure. In high-risk patients, prophylactic use of intra-aortic balloon counterpulsation may decrease the incidence VF, especially in patients with cardiogenic shock 3.
Long-term prognosis
Among patients who undergo primary PCI following a STEMI and had out-of-hospital cardiac arrest, both in-hospital and 2-year mortality was 27.5%. In the reference group of patients who had presented with STEMI and without cardiac arrest, in-hospital and 2-year mortality was 4.9 and 7.1%, respectively. After discharge from hospital there was no significant difference in mortality between the groups 4.
Outcomes of CPR and predictors of survival
A study by Sprung et al demonstrated that the incidence of periprocedural cardiac arrest decreased over the course of the study (the incidence of CPR decreased from 33.9 per 10,000 before 1995 to 13.1 per 10,000 after 1995). More than half the patients who experienced a cardiac arrest survived to be discharged from the hospital, and all were without neurologic damage. Survival after cardiac arrest did not depend on the extent of coronary artery disease. For patients who were discharged from the hospital, the fact that they experienced a cardiac arrest did not adversely affect long-term survival and the most significant predictors of mortality were prior coronary artery bypass surgery, hemodynamic instability or hypotension during catheterization, an emergency catheterization, or a procedure of prolonged duration 5.
Reference List
- Mehta RH, Harjai KJ, Grines L, Stone GW, Boura J, Cox D, O'Neill W, Grines CL. Sustained ventricular tachycardia or fibrillation in the cardiac catheterization laboratory among patients receiving primary percutaneous coronary intervention: incidence, predictors, and outcomes. J Am Coll Cardiol 2004 May 19;43(10):1765-1772.
- Henriques JP, Gheeraert PJ, Ottervanger JP, de Boer MJ, Dambrink JH, Gosselink AT, van 't Hof AW, Hoorntje JC, Suryapranata H, Zijlstra F. Ventricular fibrillation in acute myocardial infarction before and during primary PCI. Int J Cardiol 2005 December 7;105(3):262-266.
- Brodie BR, Stuckey TD, Hansen C, Muncy D. Intra-aortic balloon counterpulsation before primary percutaneous transluminal coronary angioplasty reduces catheterization laboratory events in high-risk patients with acute myocardial infarction. Am J Cardiol 1999 July 1;84(1):18-23.
- Bendz B, Eritsland J, Nakstad AR, Brekke M, Klow NE, Steen PA, Mangschau A. Long-term prognosis after out-of-hospital cardiac arrest and primary percutaneous coronary intervention. Resuscitation 2004 October;63(1):49-53.
- Sprung J, Ritter MJ, Rihal CS, Warner ME, Wilson GA, Williams BA, Stevens SR, Schroeder DR, Bourke DL, Warner DO. Outcomes of cardiopulmonary resuscitation and predictors of survival in patients undergoing coronary angiography including percutaneous coronary interventions. Anesth Analg 2006 January;102(1):217-224.