Intra-aortic balloon pump
| Cardiology Network |
 Discuss Intra-aortic balloon pump further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
The Intra-aortic balloon pump (IABP) is a mechanical device that is used to decrease myocardial oxygen demand while at the same time increasing cardiac output. By increasing cardiac output it also increases coronary blood flow and therefore myocardial oxygen delivery. It consists of a cylindrical balloon that sits in the aorta and counterpulsates. That is, it actively deflates in systole increasing forward blood flow by reducing afterload, and actively inflates in diastole increasing blood flow to the coronary arteries. [1] [2] [3] [4] [5] [6]
The balloon is inflated during diastole by a computer controlled, ECG linked mechanism. This controls the flow of helium from a cylinder into and out of the balloon. Helium is used because its low viscosity allows it to travel quickly through the long connecting tubes. The IABP is a polyethylene balloon mounted on a catheter, which is generally inserted into the aorta through the femoral artery in the leg. The pump is available in a wide range of sizes (2.5 cc to 50 cc) that will fit patients of any age and size. The balloon is guided into the descending aorta, approximately 2 cm from the left subclavian artery. At the start of diastole, the balloon inflates, augmenting coronary perfusion. At the beginning of systole, the balloon deflates; blood is ejected from the left ventricle, increasing the cardiac output by as much as 40 percent and decreasing the left ventricular stroke work and myocardial oxygen requirements. In this manner, the balloon supports the heart indirectly.
The balloon is inflated with helium, an inert gas that is easily absorbed into the bloodstream in case of rupture. Inflation of the balloon can be triggered according to the patient's electrocardiogram, their blood pressure, a pacemaker (if they have one), or by a pre-set internal rate. Optimal management of balloon timing and volume is guided by direct pressure reading. If no pressure wave is available, the ECG may be used for timing the balloon. The system is operated by an external console.
The IABP has two main benefits:
- The inflation of the balloon displaces an amount of blood to the ascending aorta which increases the pressure there and consequently increases the flow in the coronary arteries.
- The deflation of the balloon generates an expansion wave which decreases end diastolic aortic pressure and consequently reduces left ventricular myocardial oxygen requirements in the following beat.
History
In 1958 Harken described for the first time a method to treat left ventricular failure by using counterpulsation or diastolic augmentation. He suggested removing a certain blood volume from the femoral artery during systole and replacing this volume rapidly during diastole. By increasing coronary perfusion pressure this concept would therefore augment cardiac output and unload the functioning heart simultaneously. This method of treatment was limited because of problems with access (need for arteriotomies of both femoral arteries), turbulence and development of massive hemolysis by the pumping apparatus. Even experimental data showed that no augmentation of coronary blood flow was obtained.
In 1961 Clauss et al. introduced their study on arterial counterpulsation concept.
In 1962 Moulopoulus et al. adapted counterpulsation to intra-aortic balloon pumping and developed an experimental prototype of the intra-aortic balloon (IAB) whose inflation and deflation were timed to the cardiac cycle.
In 1968 the initial use in clinical practice of the IABP and it`s further improvement was realized respectfully continued by Kantrowiz`s group.
In its first years, the IABP required surgical insertion and surgical removal with a balloons size of 15 French.
In 1979, the IAB was adapted for percutaneous insertion by Bregman and Casarella, and this was followed in the early 1980s by a dual lumen, wire guided,smaller catheter device which could be placed in couple of minutes with significantly improved insertion success and reduced vascular complications.
In 1985 the first prefolded IAB was developed. These improvements permit safer use and earlier intervention to provide hemodynamic support. These advances made it for even nonsurgical personnel possible to perform an IAB insertion at the patient’s bedside. Refinements have reduced the catheter size to 8F and 9F for 30 to 50 cc balloons, and technically advanced consoles can rapidly shuttle the helium gas with automatic timing.
Use of counterpulsation
Intraaortic balloon counterpulsation is used in situations when the heart's own cardiac output is insufficient to meet the oxygenation demands of the body. These situations could include cardiogenic shock, severe septic shock, post cardiac surgery and numerous other situations.
Factors affecting diastolic augmentation
- Patient hemodynamics
- Heart rate
- Stroke volume
- Mean arterial pressure
- Systemic vascular resistance
- IABP related mechanical factors
- Intra aortic balloon position
- Intra aortic balloon in sheath
- Intra aortic balloon not unfolded
- Kink in intra aortic balloon catheter
- Intra aortic balloon leak
- Low helium concentration
- IABP console related factors
- Timing
- Position of intra aortic balloon augmentation dial
Indications & Contraindications
Indications
The following situations may benefit from this device: [1] [2] [3]
- Cardiogenic shock when used alone as treatment for myocardial infarction 9-22% survive the first year.
- Reversible intracardial mechanical defects complicating infarction, i.e. acute mitral regurgitation, papillary muscle rupture and septal perforation.
- Refractory unstable angina benefits from counterpulsation.
- Weaning from bypass surgery: Post cardiothoracic surgery most common and useful is the use of counterpulsation in weaning patients from cardiopulmonary bypass after continued perioperative injury to myocardial tissue.
- Preoperative use has been suggested for high-risk patients such as those with unstable angina with stenosis greater than 70% of main coronary artery, in ventricaular dysfunction with an ejection fraction less than 35%.
- Impending infarction
- Acute Myocardial Infarction [7]
- Refractory ventricular failure
- Support for diagnostic coronary angiographies and percutaneous coronary ınterventions
- Ischemia related intractable ventricular arrhythmias
- Septic shock
- Intraoperative pulsatile flow generation
- Cardiac support for non-cardiac surgery
- Prophylactic support in preparation for cardiac surgery
- Post surgical myocardial dysfunction / low cardiac output syndrome
- Myocardial contusion
- Mechanical bridge to other assist devices and heart transplant for those patients with left ventricular failure.
- Cardiac support following correction of anatomical defects
Contraindications
In general contraindications are as follow;
- Anatomic abnormality of femoral or iliac arteries
- Iliac or aortic atherosclerotic disease impairing blood flow run off
- Aorto femoral grafts
- Moderate or severe aortic regurgitation
- Artificial aortic valves
- Aortic dissection or aneurysm
- Patent ductus (counterpulsation may augment the abnormal pathway of aortic to pulmoner artery shunting)
- Bleeding diathesis
- Sepsis
- Sheathless insertion with severe obesity, scarring of the groin
Absolute contraindication
The following conditions will always exclude patients for treatment:[1] [2] [3]
- Aortic valve insufficiency
- Aortic dissection
- Severe aortoiliac occlusive disease
Relative contraindication
The following conditions could, under very pressing circumstances, be allowed to be included for therapy:[1]
Balloon Pump Inserting and Removal Techniques
Insertion
In the early years of IABP - therapy, insertion of the balloon was performed by surgical cut down to the femoral vessels. After a longitudinal incision in the groin, the femoral arteries were identified and controlled. A vascular graft was then sewn to the common femoral artery in an end-to-side fashion. The balloon was introduced into the artery via the graft and properly positioned in the thoracic aorta and the graft tightly secured to the distal portion of the balloon catheter. Finally the skin incision was closed. Removal of the balloon required a second operation.
Since 1979, a percutaneous placement of the IAB via the femoral artery using a modified Seldinger technique allows an easy and rapid insertion in the majority of situations. After puncture of the femoral artery a J-shaped guide wire is inserted to the level of the aortic arch and then the needle is removed. The arterial puncture side is enlarged with the successive placement of an 8 to 10,5 Fr dilator/sheath combination. Only the dilator needs to be removed. Continuing, the balloon is threaded over the guide wire into the descending aorta just below (app. 1.5 - 2 cm) the left subclavian artery. The sheath is gently pulled back to connect with the leak-proof cuff on the balloon hub, ideally so that the entire sheath is out of the arterial lumen to minimize risk of ischemic complications to the distal extremity. Recently sheathless insertion kits became available. Removal of a percutaneously placed IAB may either be via surgical removal or closed technique. There are alternative routes for balloon insertion include subclavian, axillary or iliac arteries.
Insertion of a counterpulsation balloon without a leading guidewire under any circumstances is not recommended.
- If the balloon pump is too proximal in the aorta, occlusion of the brachiocephalic, left carotid, or left subclavian arteries may occur.
- If the catheter is too distal, the celiac, superior mesenteric, or renal arteries may be obstructed.
Checking the position of the intra aortic balloon on radiographs or fluoroscopy:
- At the tip of this catheter is an approximately 1-cm metallic marker that is visible on radiographs or fluoroscopy and is used to ensure proper placement (just distal to the left subclavian artery).
- Ideally, the tip is positioned approximately 2-4 cm below the level of the aortic arch.
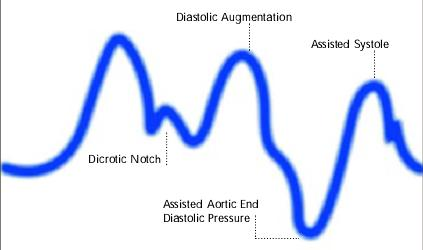
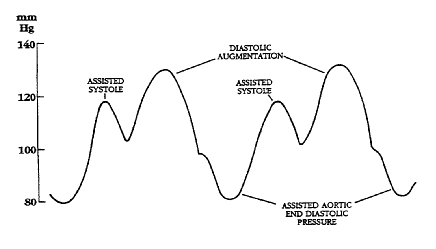
Related and helpful waveforms:
-
-
Diagram of correct intra aortic balloon timing; A= One complete cardiac cycle, B= Unassisted aortic end diastolic pressure, C= Unassisted systolic pressure, D= Diastolic augmentation, E= Reduced aortic end diastolic pressure, F= Reduced systolic pressure]]
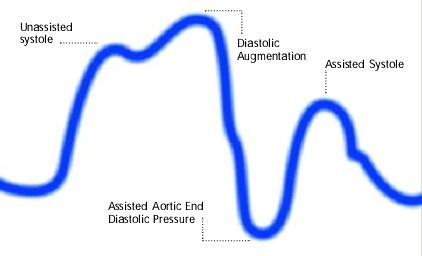
-
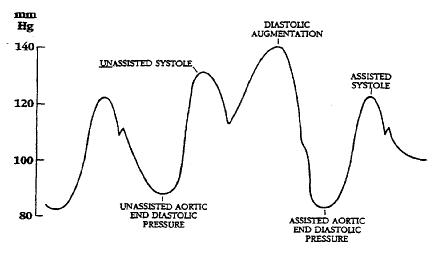
Inflation of the intra aortic balloon markedly after closure of the aortic valve (inflation of the balloon after dicrotic notch and absence of a sharp V shape)
-
Inflation of the intra aortic balloon prior to aortic valve closure (Inflation of balloon prior to dicrotic notch. Diastolic augmentation encroaches onto systole)
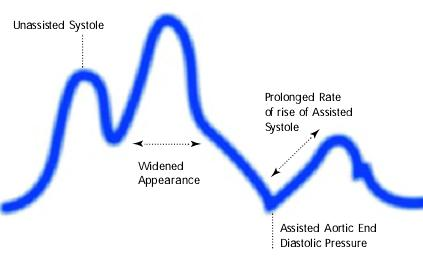
-
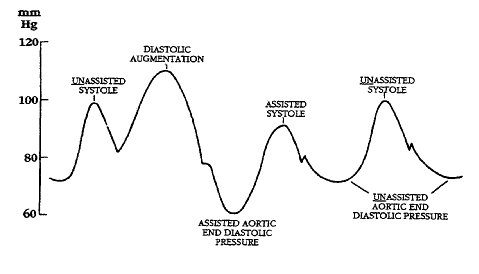
Assisted aortic end diastolic pressure may be equal to the unassisted aortic end diastolic pressure, rate of rise of assisted systole is prolonged and diastolic augmentation may appear of rise of widened
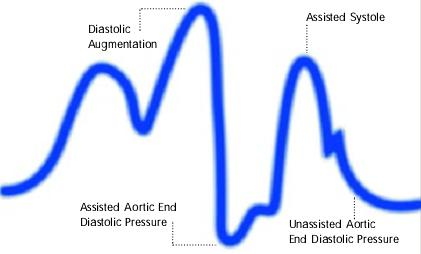
-
Premature deflation of the intra aortic balloon during the diastolic phase characterized as; deflation of balloon is seen as a sharp drop following diastolic augmentation, sub-optimal diastolic augmentation, assisted aortic end diastolic pressure may be equal to or less than the unassisted aortic end diastolic pressure and assisted systolic pressure may rise
Removal
When clinically indicated the balloon can be removed (before removal of IAB the patient is weaned progressively from support (decreasing the counterpulsation rate from 1:1 to 1:2 and then 1:3 but should not be reduced below 1:8 to reduce the change of clot formation until immediately before balloon removal) by aspirating negative pressure on the balloon lumen and withdrawing balloon and sheath together (once the balloon has been inflated, its deflated profile is larger than the sheath lumen, and therefore it cannot completely withdrawn into sheath before removal) while compressing the puncture site.
The femoral artery compressed below the puncture site as the catheter and sheath are removed to avoid embolism to the leg.
Anticoagulation should be discontinued 4 hours before and a partial thromboplastin time (PTT) or activated clotting time (ACT) should be checked before the balloon is removal. Pressure over the groin must be maintained for 30 to 60 minutes.
Assessment of patients and maintenance of IABP
- Evaluation (daily): All patients with IABP should carefully evaluated for
- Infection
- Thrombocytopenia: After balloon removal, the platelet count rapidly returns to normal
- Hemorrhage
- Hemolysis
- Vascular obstruction with limb ischemia; regular examination of radial and dorsalis pedis arteries may be helpful for quick evaluation of peripheral arteries.
- Maintenance
- Heparin administration (5000 U bolus and 1000 U/hr) is almost a standard practice.
- When performing angiography or PCI from the contralateral femoral artery a J wire is used. The balloon is placed on standby while the wire and catheter pass the balloon so that damage is minimized.
- Control of IABP
- To achieve optimal effect of intra aortic balloon counterpulsation, inflation and deflation need to be correctly timed to the patient’s cardiac cycle. This is accomplished by either using the patient’s ECG signal, the patient’s arterial waveform or an intrinsic pump rate. The most common method of triggering the IAB is from the R wave of the patient’s ECG signal. Mainly balloon inflation is set automatically to start in the middle of the T wave and to deflate prior to the ending QRS complex.
- Tachyarrhythmias, cardiac pacemaker function and poor ECG signals may cause difficulties in obtaining synchronization when the ECG mode is used. In such cases the arterial waveform for triggering may be used.
- Duration of Intra Aortic Balloon Support
The balloon is usually removed once the patient has stabilized after the acute insult.
Complications
Since the device is placed in the femoral artery and aorta it could provoke ischemia, and compartment syndrome. At highest risk is the leg which is supplied by the femoral artery may become ischemic, but also placing the balloon too distal from the arcus aortae may induce occlusion of the renal artery and subsequent renal failure. [1] [2] [3]
Other possible complications are cerebral embolism during insertion, infection, dissection of the aorta or iliac artery, perforation of the artery and hemorrhage in the mediastinum. [1] [2] [3]
Mechanical failure of the balloon itself is also a risk which entails vascular surgery to remove under that circumstance. After balloon removal there is also a risk of 'embolic shower' from micro clots that have formed on the surface of the balloon, and can lead to peripherial thrombosis, myocardial ischemia, hemodynamic decompensation, and late pseudoaneurysm. [1] [2] [3]
The success rate for percutaneous inserton of IAB is more than 90%. If signs of ischemia appear the balloon should be removed. In general, vascular injuries should be dealt with directly by surgical interventions and repair. Balloon related problems and infection require removal and / or replacement of the intra aortic balloon.
As a summary the complete list of complications include:
- Vascular
- Femoral artery perforation & dissection
- Aortic perforation & dissection
- Femoral artery thrombosis
- Peripheral embolization
- Femoral vein cannulation
- A-V fistula
- False aneurysm
- Limb ischemia
- Visceral ischemia
- Balloon related
- Perforation
- Tear
- Rupture
- Incorrect positioning
- Gas embolization
- Others
- Hemorrhage (hematomas)
- Infection
- Broken and missing balloon & catheter parts
Role of IABP in high risk coronary interventions
Although, prophylactic use of Intra Aortic Balloon Pump may provide circulatory support during percutaneous coronary interventions in patients at high risk for procedure related morbidity and mortality, usefulness of elective IABP support in patients at high risk for complications during PCI is still controversial.
Patients with pharmacologically uncontrollable chest pain, high-risk anatomic features, unprotected left main coronary artery stenosis, last remaining vessel supply, same session multivessel complex coronary interventions, coronary disease with ventricular dysfunction and severe left ventricular systolic dysfunction are likely get benefit from previous hemodynamic stabilization because even transient ischemia may produce a fatal complication.
IABP therapy provides an increase in coronary artery perfusion pressure, reducing the hemodynamic consequences of reduced coronary flow during balloon inflation and other PCI modalities. Placement and institution of IABP therapy before intervening, as opposed to provisional IABP therapy only if complications occur, may prevent intraprocedural cardiac and cerebral complications
Trivia
The IABP's developers thought that private insurance companies would not stand for such a radical new therapy, and approached the military, asking them to keep an eye out for IABP candidates in military hospitals. One day, the call came. A retired general was hospitalized in Walter Reed Army Medical Center. He had a history of multiple infarcts and was now end-stage. The IABP scientists were all ready to go, until they found out the general was former President Dwight D. Eisenhower. They declined the opportunity because they worried that if the IABP failed in him, it would permanently ruin the future prospects of the device.
Video: Intra Aortic Balloon Pump (IABP) Management
<youtube v=ZTgJQmwETUI/>
See also
- Cardiogenic shock
- Ventricular assist device
- Adjuncts for High Risk Percutaneous Coronary Interventions
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Intensive Care Medicine by Irwin and Rippe
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Intra Aortic Balloon Pump (IABP) Counterpulsation mirror with better quality by P. J Overwalder, M.D., Department of Surgery, Division of Cardiac Surgery, University Hospital Graz, The Internet Journal of Thoracic and Cardiovascular Surgery. 1999. Volume 2 Number 2.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Intra-aortic balloon pumping Department of Anaesthesia and Intensive Care of The Chinese University of Hong Kong
- ↑ Kreidieh I, Davies DW, Lim R, Nathan AW, Dymond DS, Banim SO. High-risk coronary angioplasty with elective intra-aortic balloon pump support. Int J Cardiol 1992, 35, 147–52
- ↑ Aguirre FV, Kern MJ, Bach R, Donohue T, Caracciolo E, Flynn MS, Wolford T. Intraaortic balloon pump support during high-risk coronary angioplasty. Cardiology 1994, 84, 175–86
- ↑ Szatmary L, Marco J, Fajadet J, Caster L, Carrie D. Intraaortic balloon counterpulsation and coronary angioplasty in high risk coronary heart patients. Acta Med Hung 1987, 44, 189–200
- ↑ Stone GW, Ohman EM, Miller MF, et. al. Contemporary utilization and outcomes of intra-aortic balloon counterpulsation in acute myocardial infarction: the Benchmark Registry. J Am Coll Cardiol 2003, 41, 1940-45.
External links
- Intra-aortic Balloon Pump (IABP) Texas Heart Institute
- Intra Aortic Balloon Pump (IABP) two videos demonstrating inflating and deflating the balloon
- Images in cardiovascular medicine The missing intra-aortic balloon pump catheter by Pasquale Totaro, Nello Degno, John Smith, Vincenzo Argano, Cardiac Surgery Department, Regional Cardiac Center, Morriston Hospital, Swansea, UK, Ital Heart J 2005; 6 (4): 361-362)
Template:SIB de:Intraaortale Ballonpumpe uk:Аортальна балонна контрапульсація



![Diagram of correct intra aortic balloon timing; A= One complete cardiac cycle, B= Unassisted aortic end diastolic pressure, C= Unassisted systolic pressure, D= Diastolic augmentation, E= Reduced aortic end diastolic pressure, F= Reduced systolic pressure]]](/images/e/ee/Correct_timing.png)