Hashimoto's thyroiditis pathophysiology: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (21 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Hashimoto's thyroiditis}} | {{Hashimoto's thyroiditis}} | ||
{{CMG}} {{AE}} {{MMF}} | {{CMG}}; {{AE}} {{MMF}} | ||
==Overview== | ==Overview== | ||
| Line 7: | Line 7: | ||
== Pathophysiology== | == Pathophysiology== | ||
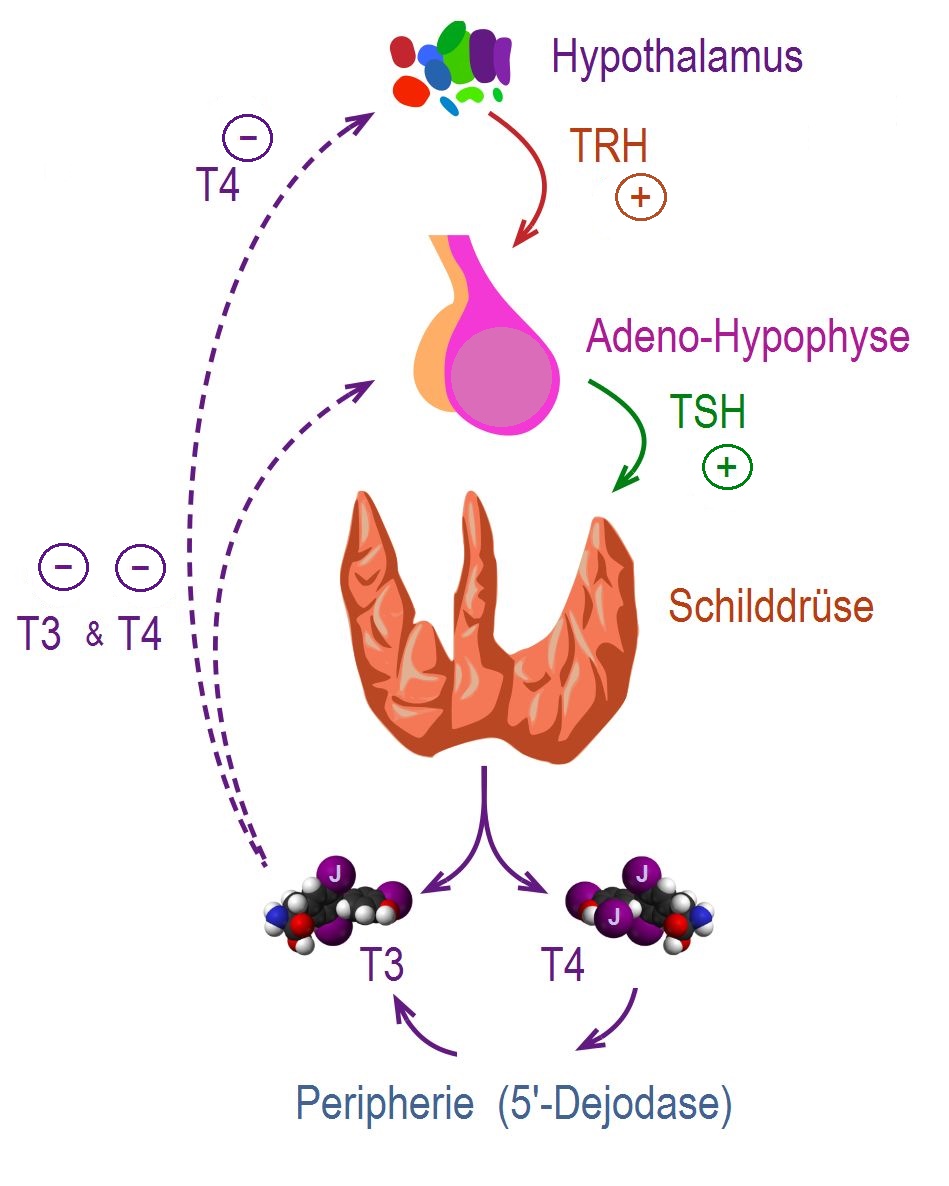
The control, synthesis, and release of the thyroid hormones is usually controlled by [[hypothalamus]] and [[pituitary gland]].<ref name="pmid25905405">{{cite journal |vauthors=De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J |title=Thyroid Hormone Synthesis And Secretion |journal= |volume= |issue= |pages= |year= |pmid=25905405 |doi= |url=}}</ref><ref name="pmid11949270">{{cite journal |vauthors=Kirsten D |title=The thyroid gland: physiology and pathophysiology |journal=Neonatal Netw |volume=19 |issue=8 |pages=11–26 |year=2000 |pmid=11949270 |doi=10.1891/0730-0832.19.8.11 |url=}}</ref> | {| | ||
|The control, synthesis, and release of the thyroid hormones is usually controlled by [[hypothalamus]] and [[pituitary gland]].<ref name="pmid25905405">{{cite journal |vauthors=De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J |title=Thyroid Hormone Synthesis And Secretion |journal= |volume= |issue= |pages= |year= |pmid=25905405 |doi= |url=}}</ref><ref name="pmid11949270">{{cite journal |vauthors=Kirsten D |title=The thyroid gland: physiology and pathophysiology |journal=Neonatal Netw |volume=19 |issue=8 |pages=11–26 |year=2000 |pmid=11949270 |doi=10.1891/0730-0832.19.8.11 |url=}}</ref> | |||
* [[Thyroid hormone|Thyroid hormones (T3 and T4)]] that regulate [[basal metabolic rate]], influence [[oxygen]] consumption by tissues. They are crucial for normal development of the [[brain]] and growth of the body. | * [[Thyroid hormone|Thyroid hormones (T3 and T4)]] that regulate [[basal metabolic rate]], influence [[oxygen]] consumption by tissues. They are crucial for normal development of the [[brain]] and growth of the body. | ||
* Secretion of [[thyroid hormones]] follows upper control from the [[hypothalamus]] and the [[pituitary]]. [[Thyrotropin-releasing hormone|Thyroid releasing hormone (TRH)]] acts on [[thyrotropes]] releasing cells in the [[pituitary]] causing them to release [[Thyroid-stimulating hormone|thyroid stimulating hormone (TSH)]]. | * Secretion of [[thyroid hormones]] follows upper control from the [[hypothalamus]] and the [[pituitary]]. [[Thyrotropin-releasing hormone|Thyroid releasing hormone (TRH)]] acts on [[thyrotropes]] releasing cells in the [[pituitary]] causing them to release [[Thyroid-stimulating hormone|thyroid stimulating hormone (TSH)]]. | ||
* [[TSH]] acts on [[thyroid gland]] by binding to specific membrane receptors and activating an [[intracellular]] pathway involving [[cAMP]] that ends in the formation and secretion of [[thyroid hormones]]. | * [[TSH]] acts on [[thyroid gland]] by binding to specific membrane receptors and activating an [[intracellular]] pathway involving [[cAMP]] that ends in the formation and secretion of [[thyroid hormones]]. | ||
* [[Iodine]] is essential for the synthesis of [[thyroid hormones]]. [[Iodide]] is | * [[Iodine]] is essential for the synthesis of [[thyroid hormones]]. [[Iodide]] is uptaken through a special Na/I transporter found in the membrane of [[thyroid]] follicular cell. After the [[iodide]] uptake, it goes through a series of organic reactions ending in the formation of the two forms of [[thyroid hormones]]: [[T3|T3 (Triiodothyronine)]] and [[T4|T4 (Thyroxine)]]. [[T3]] and [[T4]] remain stored in the [[thyroglobulin]] of the follicles and are released in response to further stimulation by [[TSH]] to the [[Thyroid follicle|thyroid follicles]]. | ||
* While [[T3]] is 3 to 5 times more potent than [[T4]], it represents only one-fourth of the total hormone secretion. [[T3]] is thought to be the biologically active form of the hormone. Most of the circulating [[T3]] is due to peripheral conversion of [[T4]] in the [[liver]] and peripheral tissues while only a small percentage is secreted directly from the [[thyroid gland]] itself. | * While [[T3]] is 3 to 5 times more potent than [[T4]], it represents only one-fourth of the total hormone secretion. [[T3]] is thought to be the biologically active form of the hormone. Most of the circulating [[T3]] is due to peripheral conversion of [[T4]] in the [[liver]] and peripheral tissues while only a small percentage is secreted directly from the [[thyroid gland]] itself. | ||
* [[T3]] and [[T4]] act on [[Nuclear receptor|nuclear receptors]] ([[DNA]] binding [[proteins]]) and cause the regulate the [[transcription]] of many [[proteins]] to regulate the [[metabolic rate]] of the body. | * [[T3]] and [[T4]] act on [[Nuclear receptor|nuclear receptors]] ([[DNA]] binding [[proteins]]) and cause the regulate the [[transcription]] of many [[proteins]] to regulate the [[metabolic rate]] of the body. | ||
* The higher regulation of [[thyroxine]] secretion follows the [[negative feedback]] role, meaning that high levels of [[T3]] and [[T4]] will suppress [[TRH]] and [[TSH]] secretion and vice versa (Low levels of [[Thyroxin|thyroxine]] will stimulate [[TRH]] and [[TSH]] secretion). This is useful in diagnosing the cause of [[hyperthyroidism]]. | * The higher regulation of [[thyroxine]] secretion follows the [[negative feedback]] role, meaning that high levels of [[T3]] and [[T4]] will suppress [[TRH]] and [[TSH]] secretion and vice versa (Low levels of [[Thyroxin|thyroxine]] will stimulate [[TRH]] and [[TSH]] secretion). This is useful in diagnosing the cause of [[hyperthyroidism]]. | ||
* [[TSH]] will be low in [[Hyperthyroidism|primary hyperthyroidism]] where the gland is the source of the excess hormones. In [[Hyperthyroidism|secondary hyperthyroidism]], [[TSH]] will be high as the [[pituitary]] or the [[hypothalamus]] are the sources of the disease. | * [[TSH]] will be low in [[Hyperthyroidism|primary hyperthyroidism]] where the gland is the source of the excess hormones. In [[Hyperthyroidism|secondary hyperthyroidism]], [[TSH]] will be high as the [[pituitary]] or the [[hypothalamus]] are the sources of the disease. | ||
| | |||
[[Image: Regulation der Schilddrüsenfunktion .jpg|right|300px|thumb|'''Regulation of thyroid hormone secretion.''' <small>Source:By CFCF; slightly modified by Geo-Science-International - This file was derived from Thyroid vector.svg:, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=47043638</small>]] | |||
|} | |||
<br clear="left" /> | |||
===Pathogenesis=== | ===Pathogenesis=== | ||
Thyroid cells undergo [[atrophy]] or transform into a type of [[follicular cell]] rich in [[mitochondria]] called Hurthle cell. [[Cellular immunity|Cellular]] and [[humoral immunity]] is thought to be involved in the pathophysiology of Hashimoto's thyroiditis:<ref name="pmid26361257">{{cite journal |vauthors=Ajjan RA, Weetman AP |title=The Pathogenesis of Hashimoto's Thyroiditis: Further Developments in our Understanding |journal=Horm. Metab. Res. |volume=47 |issue=10 |pages=702–10 |year=2015 |pmid=26361257 |doi=10.1055/s-0035-1548832 |url=}}</ref><ref name="pmid24434360">{{cite journal |vauthors=Caturegli P, De Remigis A, Rose NR |title=Hashimoto thyroiditis: clinical and diagnostic criteria |journal=Autoimmun Rev |volume=13 |issue=4-5 |pages=391–7 |year=2014 |pmid=24434360 |doi=10.1016/j.autrev.2014.01.007 |url=}}</ref> | Thyroid cells undergo [[atrophy]] or transform into a type of [[follicular cell]] rich in [[mitochondria]] called Hurthle cell. [[Cellular immunity|Cellular]] and [[humoral immunity]] is thought to be involved in the pathophysiology of Hashimoto's thyroiditis:<ref name="pmid26361257">{{cite journal |vauthors=Ajjan RA, Weetman AP |title=The Pathogenesis of Hashimoto's Thyroiditis: Further Developments in our Understanding |journal=Horm. Metab. Res. |volume=47 |issue=10 |pages=702–10 |year=2015 |pmid=26361257 |doi=10.1055/s-0035-1548832 |url=}}</ref><ref name="pmid24434360">{{cite journal |vauthors=Caturegli P, De Remigis A, Rose NR |title=Hashimoto thyroiditis: clinical and diagnostic criteria |journal=Autoimmun Rev |volume=13 |issue=4-5 |pages=391–7 |year=2014 |pmid=24434360 |doi=10.1016/j.autrev.2014.01.007 |url=}}</ref> | ||
====Cellular immunity==== | ====Cellular immunity==== | ||
*Defects in [[regulatory T cell]] response to thyroid- | *Defects in [[regulatory T cell]] response to thyroid-specific antigens in autoimmune hypothyroidism resulting in failure of [[regulatory T cell]] function. | ||
*[[Regulatory T cells]] can also | *[[Regulatory T cells]] can also dampen the [[immune response]]. [[Regulatory T cells]] are high in [[CD25]] expression and have altered activity in Hashimoto thyroiditis. | ||
* [[CD4+ cell|CD4+ cells]] are less sensitive to the inhibitory effect of [[TGFβ]] in Hashimoto thyroiditis. | * [[CD4+ cell|CD4+ cells]] are less sensitive to the inhibitory effect of [[TGFβ]] in Hashimoto thyroiditis. | ||
*There is an increased number of follicular [[helper T cells]] in patients Hashimoto's thyroiditis, which correlates with thyroid-specifc antibody levels. | *There is an increased number of follicular [[helper T cells]] in patients Hashimoto's thyroiditis, which correlates with thyroid-specifc antibody levels. | ||
| Line 54: | Line 58: | ||
*The capsule is intact, and the cut surface is light-tan and has a slight [[lobular]] pattern. | *The capsule is intact, and the cut surface is light-tan and has a slight [[lobular]] pattern. | ||
[[Image:Hashimoto's thyroiditis 1.jpg|left|thumb|400px|A gross photograph of thyroid gland taken at autopsy. The gland is only slightly enlarged and has a firm texture.<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small> | |||
]] | |||
[[Image:Hashimoto's thyroiditis 1.jpg|left|thumb|400px|A gross photograph of thyroid gland taken at autopsy. The gland is only slightly enlarged and has a firm texture.]] | |||
<br clear="left" /> | <br clear="left" /> | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
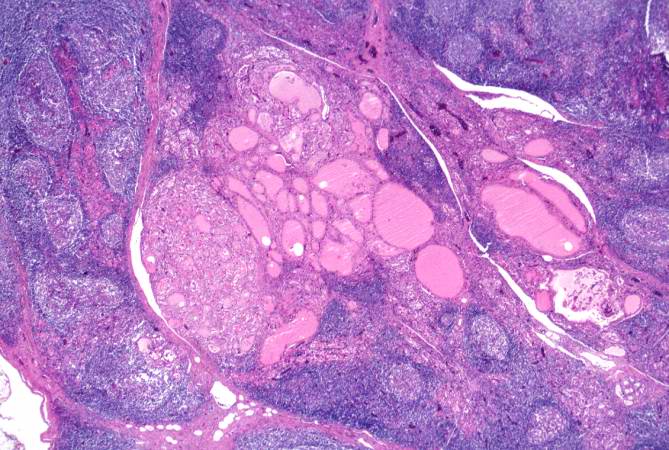
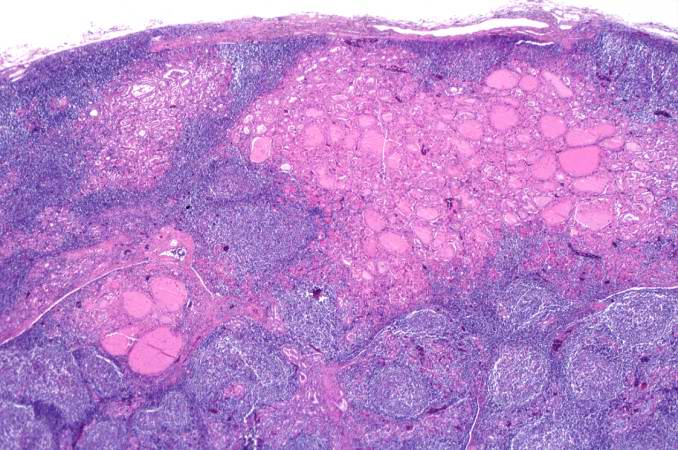
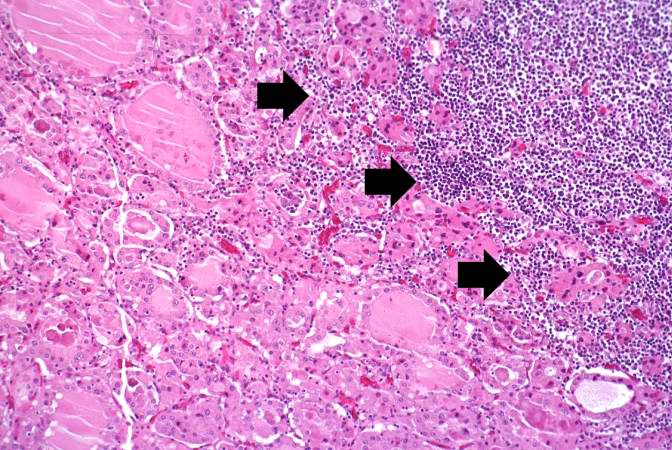
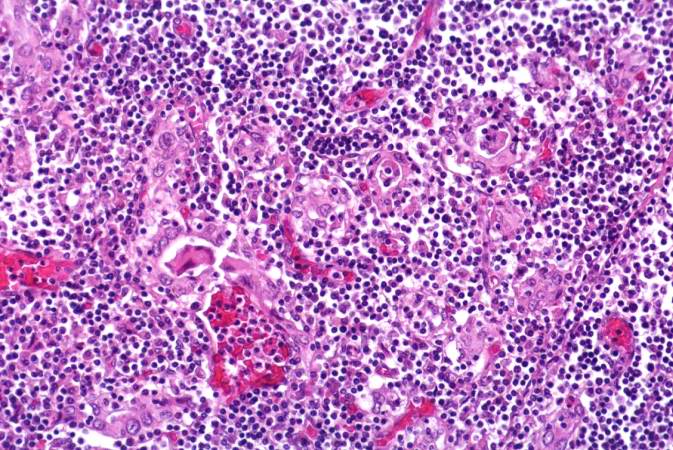
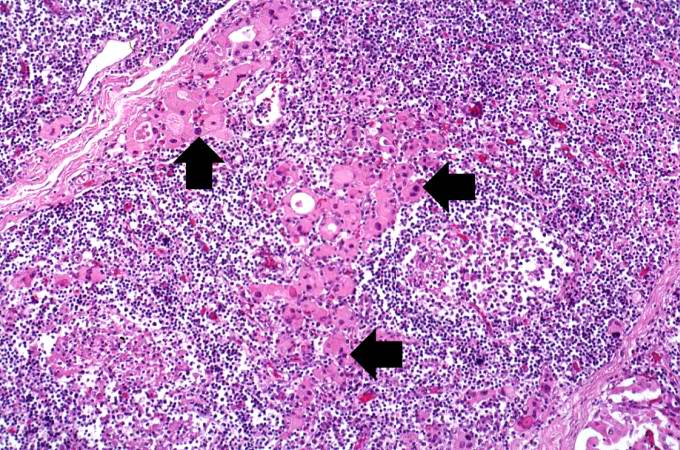
On microscopic histopathological analysis, characteristic findings of Hashimoto's thyroiditis include: | On microscopic histopathological analysis, characteristic findings of Hashimoto's thyroiditis include:<ref name="pmid24434360">{{cite journal |vauthors=Caturegli P, De Remigis A, Rose NR |title=Hashimoto thyroiditis: clinical and diagnostic criteria |journal=Autoimmun Rev |volume=13 |issue=4-5 |pages=391–7 |year=2014 |pmid=24434360 |doi=10.1016/j.autrev.2014.01.007 |url=}}</ref><ref name="urlThyroiditis — NEJM">{{cite web |url=http://www.nejm.org/doi/full/10.1056/NEJMra021194 |title=Thyroiditis — NEJM |format= |work= |accessdate=}}</ref> | ||
*Massive infiltration of the [[thyroid gland]] by [[lymphocytes]] and [[Plasma cell|plasma cells]] | *Massive infiltration of the [[thyroid gland]] by [[lymphocytes]] and [[Plasma cell|plasma cells]] | ||
*[[Germinal centers]] | *[[Germinal centers]] | ||
*[[Thyroid]] follicles are usually absent and the few remaining follicles are devoid of [[colloid]] | *[[Thyroid]] follicles are usually absent and the few remaining follicles are devoid of [[colloid]] | ||
*Hurthle cells | *[[Hurthle cells]] | ||
**Large polygonal cells with eosinophilic cytoplasm | |||
**Have an abundance of mitochondria | |||
[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
|background: "#FFFFFF;" |[[File:Hashimoto-thyroiditis-5 (1).jpg|400px|thumb|left|Photomicrograph shows '''germinal centers'''; Case courtesy of Dr Andrew Ryan, Radiopaedia.org, rID: 17084]] | |||
[[Image:Hashimoto's thyroiditis | <br clear="left" /> | ||
|background: "#FFFFFF;" |[[Image:HurthleBychkov5-08.jpg|400px|thumb|center|Micrograph of '''[[Hurthle cells]]''' <small> Courtesy of PathologyOutlines.com; Source:<ref name="urlwww.pathologyoutlines.com">{{cite web |url=http://www.pathologyoutlines.com/imgau/thyroid/ThyroidHurthleBychkov5-08.jpg |title=www.pathologyoutlines.com |format= |work= |accessdate=}}</ref>]] | |||
|- | |||
| background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 2.jpg|left|thumb|400px|This is a low-power photomicrograph of thyroid from this case. Note that the tissue is more cellular than one would expect and there does not appear to be normal colloid-filled blue spaces in this gland.<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | |||
<br clear="left" /> | |||
| background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 3.jpg|left|thumb|400px|This is a higher-power photomicrograph of thyroid from this case. Note a large number of blue-staining inflammatory cells in this tissue. These cells appear to be forming germinal centers. Some residual thyroid gland tissue can be seen in this section (arrows).<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | |||
<br clear="left" /> | <br clear="left" /> | ||
|- | |||
[[Image:Hashimoto's thyroiditis | |background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 4.jpg|left|thumb|400px|This is another view of thyroid gland filled with inflammatory cells forming germinal centers (arrows).<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | ||
<br clear="left" /> | <br clear="left" /> | ||
|background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 5.jpg|left|thumb|400px|This is a higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue.<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | |||
[[Image:Hashimoto's thyroiditis | |||
<br clear="left" /> | <br clear="left" /> | ||
|- | |||
[[Image:Hashimoto's thyroiditis | |background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 6.jpg|left|thumb|400px|This is another higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue.<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | ||
<br clear="left" /> | <br clear="left" /> | ||
|background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 7.jpg|thumb|400px|This is a high-power photomicrograph showing the inflammatory cells infiltrating into the residual thyroid tissue (arrows).<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small>]] | |||
[[Image:Hashimoto's thyroiditis | |||
<br clear="left" /> | <br clear="left" /> | ||
|- | |||
[[Image:Hashimoto's thyroiditis | |background: "#FFFFFF;" |[[Image:Hashimoto's thyroiditis 8.jpg|left|thumb|400px|This is a high-power photomicrograph showing the lymphocytes and plasma cells surrounding the thyroid gland epithelium.<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small> ]] | ||
<br clear="left" /> | <br clear="left" /> | ||
|background: "#FFFFFF;" |[[Image: Hashimoto's thyroiditis 9.jpg|left|thumb|400px|This high-power photomicrograph shows more clearly the lymphocytes and plasma cells surrounding the thyroid gland epithelium. Large, eosinophilic, degenerating thyroid gland cells (Hurthle cells) can be seen in this section (arrows).<small><small>[http://www.peir.net Images courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]</small></small> ]] | |||
[[Image:Hashimoto's thyroiditis | |||
<br clear="left" /> | <br clear="left" /> | ||
|- | |||
|} | |||
==References== | ==References== | ||
| Line 98: | Line 105: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category: | | ||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | [[Category:Endocrinology]] | ||
[[Category:Up-To-Date]] | |||
Latest revision as of 21:58, 29 July 2020
|
Hashimoto's thyroiditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hashimoto's thyroiditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hashimoto's thyroiditis pathophysiology |
|
Risk calculators and risk factors for Hashimoto's thyroiditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
Hashimoto's thyroiditis (HT) is characterized by lymphocytic infiltration of the thyroid gland and production of antibodies that recognize thyroid-specific antigens. The pathogenesis is not yet completely understood. Thyroid cells undergo atrophy or transform into a type of follicular cell rich in mitochondria called Hurthle cell. It is currently thought that the disease is caused by abnormalities in cellular and humoral immunity which results in a localized cell-mediated immune response directed toward the thyroid parenchymal cells. This results in the decreased production of thyroid hormones.
Pathophysiology
The control, synthesis, and release of the thyroid hormones is usually controlled by hypothalamus and pituitary gland.[1][2]
|
 |
Pathogenesis
Thyroid cells undergo atrophy or transform into a type of follicular cell rich in mitochondria called Hurthle cell. Cellular and humoral immunity is thought to be involved in the pathophysiology of Hashimoto's thyroiditis:[3][4]
Cellular immunity
- Defects in regulatory T cell response to thyroid-specific antigens in autoimmune hypothyroidism resulting in failure of regulatory T cell function.
- Regulatory T cells can also dampen the immune response. Regulatory T cells are high in CD25 expression and have altered activity in Hashimoto thyroiditis.
- CD4+ cells are less sensitive to the inhibitory effect of TGFβ in Hashimoto thyroiditis.
- There is an increased number of follicular helper T cells in patients Hashimoto's thyroiditis, which correlates with thyroid-specifc antibody levels.
Humoral immunity
- Patients with Hashimoto thyroiditis have positive antibodies against thyroglobulin (TG) and thyroid peroxidase (TPO).
- Recently, a distinct variant of HT has been documented where the thyroid gland is infiltrated with IgG4-positive cells.
- Thyroid hormone receptor antibodies might be involved in the disease presentation as sometimes thyroiditis presents as hyperthyroidism. The balance between the thyroid stimulating antibodies (TSAb) and thyroid blocking antibodies (TBAb) explains the fluctuating hormone levels in patients with Hashimoto's thyroiditis. It should also be noted that thyroid stimulating antibodies (TSAb) might have a minor blocking action.
- The sodium-iodide symporter (NIS) mediates iodine uptake by the thyroid gland, while pendrin is responsible for the efflux of iodine through thyroid follicles. Antibodies against NIS and pendrin are also found in Hashimoto thyroiditis (HT).
Cytokines
- Increased plasma level and expressions of IL-17 and IL-22 are seen in HT.
Micro RNA
- MicroRNAs (miRNA), which are small noncoding RNA regions, have also been implicated in the pathogenesis of thyroid immunity. In HT tissue, a decreased level of miR-155_2 and an increase in miR-200a1 was found.
Genetics
- A family history of thyroid disorders is common, with HLA-B* 46:01 confers an increased risk of HT developing in Han Chinese children. HLA-A* 02:07 and HLA-DRB4 conferred susceptibility. The genes implicated vary in different groups and the incidence is increased in patients with chromosomal disorders, including Down's syndrome and Turner syndrome.[3][5]
Associated conditions
The following conditions are associated with Hashimoto's thyroiditis:[6]
- Type 1 diabetes
- Addison's disease
- Pernicious anemia
- Vitiligo
- Rheumatoid arthritis
- Premature ovarian failure
Gross Pathology
On gross pathology the characteristic findings of Hashimoto's thyroiditis are.[4][7]
- The gland is usually diffusely enlarged, firm, and slightly lobular.
- The capsule is intact, and the cut surface is light-tan and has a slight lobular pattern.

Microscopic Pathology
On microscopic histopathological analysis, characteristic findings of Hashimoto's thyroiditis include:[4][7]
- Massive infiltration of the thyroid gland by lymphocytes and plasma cells
- Germinal centers
- Thyroid follicles are usually absent and the few remaining follicles are devoid of colloid
- Hurthle cells
- Large polygonal cells with eosinophilic cytoplasm
- Have an abundance of mitochondria

|
 |

|

|

|
|
|
|
|
|
References
- ↑ De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Rousset B, Dupuy C, Miot F, Dumont J. "Thyroid Hormone Synthesis And Secretion". PMID 25905405.
- ↑ Kirsten D (2000). "The thyroid gland: physiology and pathophysiology". Neonatal Netw. 19 (8): 11–26. doi:10.1891/0730-0832.19.8.11. PMID 11949270.
- ↑ 3.0 3.1 Ajjan RA, Weetman AP (2015). "The Pathogenesis of Hashimoto's Thyroiditis: Further Developments in our Understanding". Horm. Metab. Res. 47 (10): 702–10. doi:10.1055/s-0035-1548832. PMID 26361257.
- ↑ 4.0 4.1 4.2 Caturegli P, De Remigis A, Rose NR (2014). "Hashimoto thyroiditis: clinical and diagnostic criteria". Autoimmun Rev. 13 (4–5): 391–7. doi:10.1016/j.autrev.2014.01.007. PMID 24434360.
- ↑ Barbesino G, Chiovato L (2000). "The genetics of Hashimoto's disease". Endocrinol. Metab. Clin. North Am. 29 (2): 357–74. PMID 10874534.
- ↑ "Thyroiditis - American Family Physician".
- ↑ 7.0 7.1 "Thyroiditis — NEJM".
- ↑ "www.pathologyoutlines.com".