Colitis
|
WikiDoc Resources for Colitis |
|
Articles |
|---|
|
Most recent articles on Colitis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Colitis at Clinical Trials.gov Clinical Trials on Colitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Colitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Colitis Risk calculators and risk factors for Colitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Colitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: M.Umer Tariq [2]; Maham Khan [3]; Ogheneochuko Ajari, MB.BS, MS [4]; Rim Halaby, M.D. [5]; Qasim Salau, M.B.B.S., FMCPaed [6]
Synonyms and keywords: Proctocolitis, Proctitis, Enterocolitis.
Overview
Colitis is the inflammation of the colon, that can be either acute or chronic. Causes of colitis include infectious causes such as Chlamydia trachomatis, Neisseria gonorrhoeae, Shigella dysenteriae, HSV, allergic cause( food potein-induced proctocolitis) and radiation. Colitis may co-exist with enteritis (inflammation of the small bowel), proctitis (inflammation of the rectum) or both. The mainstay of therapy for infectious proctocolitis is antimicrobial therapy. The preferred regimen is a combination of Ceftriaxone and Doxycycline.
Classification
There is no established classification system for colitis. However, it may be classified based on etiology, age and duration of symptom.
Classification by etiology
| Classes of Colitis | Disorders |
| Autoimmune | |
| Allergic | |
| Infectious colitis |
|
| Idiopathic | |
| Iatrogenic | |
| Vascular | |
| Drug induced | |
| Unclassifiable |
|
Classification by Anatomy
Colitis may co-exist with inflammation involving other parts of the gastrointestinal tract. It can be classified based on anatomy into;
- Proctitis: When it involves the rectum
- Colitis: When it involves the inflammation is limited to the colon
- Proctocolitis: When it involves the rectum and colon (usually the distal part of the colon 12cm to 15cm above the anus (sigmoid colon)[1][2]
- Enterocolitis: When it involves the small intestine in addition to the colon
Schematic of Anatomical Classification of Colitis
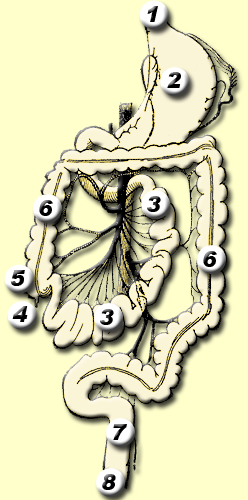
*Regions 4 to 6: Enterocolitis
*Region 6: Colitis
*Regions 6 to 8: Proctocolitis
*Regions 7 to 8:Proctitis
Classification by Age
Classification by duration of symptoms
Notes:
- Fulminant colitis is any colitis with a rapid downhill clinical course; in addition to the diarrhea, fever, and anemia seen in colitis, the patient has severe abdominal pain and presents a clinical picture similar to that of septicemia, where shock is present.
- Irritable bowel syndrome, a separate disease, has been called spastic colitis or spastic colon. This name causes confusion, since colitis is not a feature of irritable bowel syndrome.
- Immune mediated colitis is the experimental name in animal studies of ulcerative colitis. It is a synonym of ulcerative colitis, but it should not be used as a synonym when referring to ulcerative colitis.
Pathophysiology
The pathophysiology of colitis depends on the cause. Some pathogenetic mechanisms are not clearly understood.
Pathogenesis
Hypothesis regarding pathogenesis of Allergic colitis
- It is a non IgE immunological reaction against food protein antigens which is thought to be T cell mediated.[5][8][9][10][11]
- T cell (CD8 and TH-2) results in release of proinflammatory cytokines, such as TNF, attracting Eosinophils mainly and other polymorphonuclear cells (PMN) to the intestinal tract and subsequent inflammation.
- Genetic influence may have a role to play, may be seen in families.
- Could also be an autoimmune disease. Atypical p antineutrophil cytoplasmic antibodies (a-pANCA) have been seen in some infants with intestinal infiltration by Neutrophils.[12]
Pathogenesis of Infectious colitis
- Enteric organisms that cause colitis are usually acquired through feco-oral contamination especially in children. As few as 100 bacterial cells can be enough to cause an infection.[13]
- Can also be acquired as a sexually transmitted infection (STI) among individuals who practice unsafe anal sex.
- The pathogens are transmitted directly through overt abrasions or microabrasions in the rectal mucosa or indirectly during oral-anal contact.[14]
- May also occur following antibiotic use, especially broad spectrum antibiotics.
- Chlamydia trachomatis
- Inoculation and replication of Chlamydia trachomatis serovars L1, L2, or L3 depends on alternation between two forms of the bacterium: the infectious elementary body (EB) and noninfectious, replicating reticulate body (RB).[15]
- The EB form is responsible for inoculation with C. trachomatis.
- The C. trachomatis EB enters the body during sexual intercourse or by crossing epithelial cells of mucous membranes.[16]
- Once inside the host cell, EBs immediately start differentiating into reticulate bodies (RBs) that undergo replication.
- The process of endocytosis and accumulation of RBs within host epithelial cells causes host cell destruction (necrosis) which leads to the formation of a papule at the site of inoculation which may ulcerate, depending on the extent of infection and number or EBs transmitted.[17]
- Shigella specie
- Shigella first invades the epithelial cells of the large intestine (the rectosigmoid mucosa) by using M cells as entry ports for transcytosis. Shigella then invades macrophages and induces cellular apoptosis, which results in inflammation, generation of proinflammatory cytokines, and recruitment of polymorphonuclear neutrophils (PMNs).[18]
- Campylobacter
- Regarding Campylobacter jejuni colitis the exact pathogenesis by which it causes colitis after transmission is not fully understood.
- However, it is hypothesized that requirement for C. jejuni virulence include (1) motility, (2) drug resistance, (3) host cell adherence, (4) host cell invasion, (5) alteration of the host cell signaling pathways, (6) induction of host cell death, (7) evasion of the host immune system defenses, and (9) acquisition of iron which serves as a micronutrient for growth and works as a catalyst for hydroxyl radical formation.[19]
- C. jejuni is known to also secrete proteins that may contribute to the ability of the bacterium to invade the host epithelial cells.[19]
Entameoba histolytica
- Following transmission of Entameoba histolytica, the trophozoites undergo excystation in the small intestine, after which it migrates to the large intestine using pseudopods.
- In the large intestine, the trophozoites invades the intestinal mucosa into the bloodstream. Simultaneously, they form resistant cysts in the large intestines that are then excreted in human stools.[20]
- E. histolytica trophozoites secrete proteases, which induce the release of mucin from goblet cells, resulting in glandular hyperplasia.[20]
- E. histolytica is also said to contain glycosidases that cleave glycsolyated mucin molecules, resulting in mucin degradation.[21][22]
- Pseudomembranous colitis
- Under normal condition, there is usually a balance in the normal intestinal commensals.
- Following broad spectrum systemic antibiotics use, especially penicillin-based antibiotic such as amoxicillin, cephalosporins, fluoroquinolones and macrolides this balance is affected with killing susceptible bacteria and allowing for proliferation of the remaining non-susceptible bacteria.
- Clostridium difficile, an obligate anaerobic gram positive spore forming bacillus tends to proliferate under such conditions and is the usual cause (almost 99 percent of cases) of pseudomembranous colitis.[23]
- Clostridium difficile, produces toxin A (enterotoxin), toxin B (cytotoxin), and binary toxin. These toxins are required for it to colonize the gut, intestinal cell disruption, attract inflammatory cells and cause disease.[24][23]
- Other reported causes of pseudomembranous colitis include infections such as Staphylococcus aureus, Yersinia specie, Salmonella specie, Shigella specie, NSAIDs such as indomethacin, chemotherapeutic drugs like - cisplatin and inflammatory bowel disease.
Pathogenesis of radiation colitis
- Occur following radiation treatment for pelvic tumors.[25][26][27][28]
- More common with radiation doses higher than 45Gy.[28]
- The DNA is the main site of damage. May also affect RNA, proteins and cell membranes.
- Injury occurs few hours to days, up to three months after irradiation in acute radiation proctocolitis. It affects rapidly dividing cells of the epithelium and mucosa.
- This leads to cell death, recruitment and activation of polymorphonuclear (PMN) inflammatory cells, mucosal edema and damage to small blood vessels.
- Usually self limiting.
- In chronic radiation colitis, mesenchymal tissue is involved.
- The damage is progressive with atrophy of the mucosa, fibrosis of the intestinal wall, obliteration of small arteries, chronic ischemia, ulcers, and fistula formation.
- This occurs usually after three months to years.
Pathogenesis of ischemic colitis
- Rare cause of colitis
- Seen in the elderly with low cardiovascular status
- The exact pathogenesis remains unclear. It is characterized by polymorphonuclear (PMN) cells infiltration, extensive mucosal necrosis and bleeding, submucosa edema and absence of lymphocytes and plasma cells in the deeper aspect of the lamina propria.[29]
- Exact pathogenesis not fully clear.
- It is a chronic inflammatory disease affecting the innermost part of the lamina propria.
- An interplay between hyper-reactive immune system, gut microbiota, Impaired gut mucosa barrier, genetic factors, and environmental factors.[30][31][32]
- Cytotoxic T cells and autoantibodies (IgG and IgE) against the colon, cytoskeleton and bowel smooth muscles are seen.[30]
- The balance in gut microbes is shifted toward pathogenic microorganism, including colonic sulphate reducing bacteria.[31]
- About 160 genetic loci have been identified for inflammatory bowel disease (IBD) with newer potential loci being identified. Some of these loci are associated with impaired mucosal barrier function.[32]
Other pathogenetic mechanisms of proctocolitis=
- NSAIDS can also cause proctocolitis. The mechanism is not completely understood.[33][34]
- Inhibits cyclooxygenase and thus prostaglandin production. Prostaglandin helps maintain mucosal integrity.
- NSAIDS also impair oxidative phosphorylation, increasing risk of oxidative injury to the gut.
- Direct damage to the intestinal mucosa has been suggested in NSAID related injury since the rectum is often spared.
- It is also hypothesized that there is increased intestinal permeability with to antigenic materials following NSAID use, causing activation of the immune system and subsequent inflammation.
- Glutaraldehyde, a disinfectant used in cleaning endoscopes is an uncommon cause of proctocolitis.[35][36]
- Proctocolitis results from direct mucosa contact with the chemical.
- Improper cleaning of the endoscopes allows the glutaraldehyde disinfectant to remain, subsequently causing a chemical proctocolitis.
- The primary mucosa toxin in glutaraldehyde is not fully known. However, it may be related to the aldehyde.[35]
Genetics
There is no specific genetic cause for proctocolitis. However, genetic predisposition may play a role in some causes.[12][32]
Associated conditions
- Human Immunodeficiency Virus (HIV)/ AIDS
- Arterosclerosis
- Artificial infant feeding
Gross pathology
- Gross pathological findings are often limited to the rectosigmoid region and show evidence of acute or chronic inflammation with or without necrosis, ulcers and hemorrhage. In addition, specific changes based on the cause may be seen.
- Food protein-induced proctocolitis (FPIP) shows patchy or diffuse erythematous and friable mucosa. Characteristic circumscribed nodular hyperplasia with central pit-like erosions and ulcers may also be seen.[37][38]
- Pseudomembranous colitis. The gross pathologic finding is presence of diffuse, small, 2 to 10mm, raised yellowish (or whitish) lesions. Mucosa in between lesions may appear normal. Lesions may merge giving rise to a characteristic "pseudomembrane" layer over the mucosa.
- Ulcerative colitis. On gross pathology, the inflammation is seen in the innermost part of the lamina propria.
- Ischemic proctocolitis shows marked mucosal congestion with areas of necrosis and ulceration on gross patholgy.[29]
-
Allergic proctocolitis[39]
-
Radiation Proctitis[40]
-
Pseudomembranous colitis. (WC) [41]
-
Pseudomembranous colitis. [42]
-
Ulcerative colitis.[43]
Microscopic pathology
- Food protein-induced proctocolitis is characterized by marked eosinophil infiltrates in the mucosa of the rectosigmoid area.[37][44]
- The mucosa architecture is usually preserved on microscopy.[37]
- In pseudomembranous colitis microscopy shows[45]
- Heaped necrotic tissue
- Polymorphonuclear neutrophils in the lamina propria, breeching the epithelium like a "volcanic eruption".
- With or without capillary thrombi
- On microscopy, the characteristic finding in ulcerative colitis is presence of lymphocytes and plasma cells in the deeper aspect of the lamina propria (basal lymphoplasmacytosis).
- Crypt architecture is destroyed.
- Abscesses may also be seen in the crypts.
-
Ulcerative colitis. H&E staining showing crypt abscess, a characteristic finding in ulcerative colitis [46]
-
Ulcerative colitis. H&E stain showing marked lymphocytic infiltration (blue/purple) of the intestinal mucosa and distortion of the architecture of the crypts. [47]
-
Ischemic colitis. H&E staining showing changes seen in ischemic colitis [48]
-
Pseudomembranous colitis. H& E staining showing pseudomembranes in Clostridium colitis [49]
Causes
Common Causes
Common causes of Proctocolitis include infectious agents such as Chlamydia trachomatis (which causes LGV (Lymphogranuloma Venereum), Neisseria gonorrhoeae, HSV, Shigella dysenteriae and Campylobacter species. It can also be allergic (for example food protein-induced proctocolitis), idiopathic (for example microscopic colitis), vascular (for example ischemic colitis), or autoimmune (for example inflammatory bowel disease).
Causes by Organ System
Causes in Alphabetical Order
Life Threatening Causes
Example include toxic megacolon, ischemic colitis, infectious colitis such as escherichia coli O157:H7 and shigella.
Diagnosis
Symptoms
Physical Examination
Diagnostic Tests
Colitis is associated with the following findings:
- Swelling of the colon tissue
- Bleeding
- Erythema (redness) of the surface of the colon
- Ulcerations of the colon
Common tests which reveal these signs include:
- X-rays of the colon
- Testing the stool for blood and pus
- Sigmoidoscopy
- Colonoscopy
Additional tests include stool cultures and blood tests, including blood chemistry tests. A high erythrocyte sedimentation rate (ESR) is one typical finding in acute exacerbations of colitis.
Treatment
Medical Therapy
Treatment of colitis may include the administration of antibiotics and general anti-inflammatory medications such as Mesalamine or its derivatives, steroids, or one of a number of other drugs that ameliorate inflammation.
Changes in diet can be effective at treating the symptoms of colitis and easing the side effects. These can include reducing the intake of carbohydrates, lactose products, soft drinks, and caffeine. This approach has been championed by Elaine Gottschall.
Hygienic and naturopathic doctors have taken the diet approach further, attributing bowel inflammation to toxemia stemming from high-protein, fatty diets and other dietary irritants. Changing to a low-fat, minimally-processed, whole-foods diet per the Natural Hygiene self-healing system has been effective in eliminating symptoms and rebuilding health. Dr. Zarin Azar, MD,, is one advocate of this healing system.
Infliximab (or REMICADE) - a drug originally produced to treat Rheumatoid Arthritis - has recently been approved for the treatment of Colitis where traditional treatments have failed. REMICADE is a biologic therapy that recognizes, attaches to, and blocks the action of a protein in your body called tumor necrosis factor alpha (TNF-alpha). TNF-alpha is made by certain blood cells in your body. It is administered through a series of infusions.
Surgery
Approximately half of patients with fulminant colitis require surgery. Surgery usually entails removing the colon and bowel and creating a "pouch" with portions of the small intestine.
Differentiating Colitis from Other Diseases
Causes of proctocolitis are diverse and may overlap with other disease. The differential diagnosis of proctocolitis can be classified into two according to age group.
Differential diagnosis in Infants
- Swallowed maternal blood syndrome
- Anorectal fissure
- Necrotizing enterocolitis especially in preterm babies
- Vitamin K dependent hemorrhage
- Other Coagulopathies: (hereditary such as coagulation factor deficiency or acquired such as disseminated intravascular coagulopathy)
- Food protein-induced enterocolitis
- Intussusception
- Gastrointestinal Infections
- Meckel diverticulum
- Intestinal duplication cysts
- Vascular malformations
- Inflammatory bowel disease(early onset)
- Hirschsprung disease complicated by enterocolitis
- Volvolus
- Gastro-duodenal ulcers
- Gastrointestinal duplication cyst
- Liver disease with clotting factor deficiency
- Lymphonodular hyperplasia
Differential diagnosis in Infants
- Colorectal malignancy
- Crohn's disease
- Behcet's disease
- Arteriovenous malformation
- Diverticuclosis
- Infection
- Coagulopathy
- Systemic lupus erythematosus(SLE)
Epidemiology and Demographics
The causes of proctocolitis are diverse and overlap with other diseases.
Prevalence and Incidence
- The exact prevalence and incidence of proctocolitis is difficult to establish due to diverse causes and appropriate diagnostic criteria
- The prevalence and incidence of proctocolitis may be influenced by the patient’s age, genetic factors and race
- Food protein-induced proctocolitis (FPIP): Exact prevalence unknown
- Reported to be 1.6 in 1000 children under 1 year for cow-milk protein allergy in a population based study[52]
- Prevalence of FPIP is documented to range from a low of 16 percent to a high of 64 percent among infants with rectal bleeding[4][53][54]
- Sixty percent of infants with FPIP are babies who are on exclusive breastfeeding[55][4]
- FPIP is the most common cause of non-infectious colitis in infancy [12]
- The prevalence of proctocolitis from an adults study in a developed country between 1979 and 1983 was 58.4 cases per 100,000[56]
- The incidence of proctocolitis from the same study was 6.8 cases per 100,000 individuals per year[56]
- Regarding radiation proctitis the incidence is not fully known due in part to no standard definition and method of reporting[57]
- The incidence of radiation proctitis following external beam radiation studies range from 2% to 39%, brachytherapy 8% to 13%, while that of intensity-modulated radiation therapy (IMRT) range from 1% to 9%[57]
- Also, the incidence of acute radiation proctitis occurs in 20% of individuals undergoing radiation therapy, while chronic radiation proctitis occurs in 2% to 20% of individuals having radiation therapy[57]
- Ischemic proctocolitis makes up 3% to 5% of cases of ischemic injury to the colon[29]
- Food protein-induced proctocolitis (FPIP): Exact prevalence unknown
Age
- Food protein-induced proctocolitis is mainly a disease of infants, with onset usually in the first two to three months of life[4][53][54]. An adolescent form may develop later.[6]
- The incidence of infectious proctocolitis that is not acquired as a sexually transmitted infection (STI) is higher among pediatric age group
- Ischemic proctocolitis is more common among the elderly with average age range of 65 to 70 years[29][58]
- Other causes of proctocolitis are more common among the adult population than pediatric age group
Gender
- Infectious proctocolitis from STI is more common in men[59][60][61][62]
- The other causes of proctocolitis have no sex predilection
Race
- There is no racial predilection for proctocolitis
Risk Factors
Common risk factors for developing proctocolitis include:
Risk factors for food protein-induced proctocolitis (FPIP)
- Family history of atopy/ previous sibling with FPIP
- Use of formula feeds
Risk factors for ischemic proctocolitis
- Elderly or debilitated patients who have multiple comorbidities.
- Cardiovascular disease including atherosclerotis and peripheral vascular disease
- Diabetes mellitus
- Aortoiliac surgery
- Hemodialysis
- Pulmonary vascular disease
- Shock
- Sepsis
Risk factors for radiation proctocolitis
- Dose of radiation > 70 Gy
- Diabetes
- Peripheral vascular disease
- Co-existing inflammatory bowel disease
- HIV/AIDS
Risk factors for sexually transmitted infectious proctocolitis
- Men who have sex with men
- Unprotected anal sex
- HIV/AIDS
- Previously diagnosed sexually transmitted infection
- Casual sex acquaintance especially meeting on the internet/ multiple
- Recent foreign travel
- Co-existing ulcerative colitis
Risk factors for Clostridium difficile proctocolitis
- Elderly
- Use of antimicrobials especially broad spectrum antibiotics such as penicillins, cephalosporins, clindamycin and fluoroquinolones
- Chemotherapy
- Immune hypo-function
- Gastrointestinal surgery including proctocolectomy
- Mechanical bowel preparation
- Constipation
- Gut ischemia
- Hirschsprung disease
- Altered gut motility
- Malnutrition
- Elderly age group
- Prolonged medication use e.g NSAIDs
- Improper cleaning/ rinsing of glutaraldehyde disinfectant used in endoscopes
Screening
- According to the CDC routine screening, at least annually for common sexually transmitted diseases should be done in sexually active MSM
- A test for rectal infection with N. gonorrhoeae and C. trachomatis in men who have had receptive anal intercourse during the preceding year (using nucleic acid amplification testing (NAAT) of a rectal swab is the preferred approach)
- More frequent STD screening at 3-6 month intervals is indicated for MSM who have multiple or anonymous partners and in those who use illicit drug (particularly methamphetamine use) or whose sex partners participate in these activities
Other causes of proctocolitis
- Screening is not recommended for the other causes of proctocolitis
Natural History, Complications, and Prognosis
Natural History
The natural history of proctocolitis depends on the cause Food protein-induced proctocolitis (FPIP)
- The symptoms of FPIP typically develop in the first two or three months of life in an exclusively breastfed infant. Symptoms resolve within 48hrs to 96 hrs following avoidance of trigger protein. Spontaneous resolution of symptoms may occur in 20% of the children without elimination of the offending protein. Most infants will be able to tolerate the offending protein by 1 to 3 years of age.[4][63][8]
- The natural history of FPIP that develop in adolescence or early adulthood is not fully characterized[6]
Ischemic colitis
The presentation depends on the degree of bowel involvement. Mortality is high among those with full thickness bowel ischemia.[29]
Complications
Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
Physical Examination
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
- All patients with proctocolitis should be treated.
- Treatment of proctocolitis is similar to that of proctitis.
- Generally, the following regimen is recommended:
- Preferred regimen: Ceftriaxone 250 mg IM AND Doxycycline 100 mg PO bid for 7 days
To view additional treatment and special considerations for the management of proctitis/proctocolitis, click here.
Surgery
Prevention
See also
References
- ↑ 2015 Sexually Transmitted Diseases Treatment Guidelines. Centers for Disease Control and Prevention (2015).http://www.cdc.gov/std/tg2015/proctitis.htm Accessed on August 29, 2016
- ↑ Hamlyn E, Taylor C (2006). "Sexually transmitted proctitis". Postgrad Med J. 82 (973): 733–6. doi:10.1136/pmj.2006.048488. PMC 2660501. PMID 17099092.
- ↑ WikiMedia Commons https://commons.wikimedia.org/wiki/File:Gastro-intestinal_tract.png. Accessed on September 09, 2016
- ↑ 4.0 4.1 4.2 4.3 4.4 Nowak-Węgrzyn A (2015). "Food protein-induced enterocolitis syndrome and allergic proctocolitis". Allergy Asthma Proc. 36 (3): 172–84. doi:10.2500/aap.2015.36.3811. PMC 4405595. PMID 25976434.
- ↑ 5.0 5.1 Pumberger W, Pomberger G, Geissler W (2001). "Proctocolitis in breast fed infants: a contribution to differential diagnosis of haematochezia in early childhood". Postgrad Med J. 77 (906): 252–4. PMC 1741985. PMID 11264489.
- ↑ 6.0 6.1 6.2 Alfadda AA, Storr MA, Shaffer EA (2011). "Eosinophilic colitis: epidemiology, clinical features, and current management". Therap Adv Gastroenterol. 4 (5): 301–9. doi:10.1177/1756283X10392443. PMC 3165205. PMID 21922029.
- ↑ 7.0 7.1 Hauer-Jensen M, Denham JW, Andreyev HJ (2014). "Radiation enteropathy--pathogenesis, treatment and prevention". Nat Rev Gastroenterol Hepatol. 11 (8): 470–9. doi:10.1038/nrgastro.2014.46. PMC 4346191. PMID 24686268.
- ↑ 8.0 8.1 Lucarelli S, Di Nardo G, Lastrucci G, D'Alfonso Y, Marcheggiano A, Federici T; et al. (2011). "Allergic proctocolitis refractory to maternal hypoallergenic diet in exclusively breast-fed infants: a clinical observation". BMC Gastroenterol. 11: 82. doi:10.1186/1471-230X-11-82. PMC 3224143. PMID 21762530.
- ↑ Chesworth BM, Hamilton CB, Walton DM, Benoit M, Blake TA, Bredy H; et al. (2014). "Reliability and validity of two versions of the upper extremity functional index". Physiother Can. 66 (3): 243–53. doi:10.3138/ptc.2013-45. PMC 4130402. PMID 25125777.
- ↑ Academy of Breastfeeding Medicine (2011). "ABM Clinical Protocol #24: Allergic Proctocolitis in the Exclusively Breastfed Infant". Breastfeed Med. 6 (6): 435–40. doi:10.1089/bfm.2011.9977. PMID 22050274.
- ↑ Fagundes-Neto U, Ganc AJ (2013). "Allergic proctocolitis: the clinical evolution of a transitory disease with a familial trend. Case reports". Einstein (Sao Paulo). 11 (2): 229–33. PMC 4872900. PMID 23843067.
- ↑ 12.0 12.1 12.2 Sekerkova A, Fuchs M, Cecrdlova E, Svachova V, Kralova Lesna I, Striz I; et al. (2015). "High Prevalence of Neutrophil Cytoplasmic Autoantibodies in Infants with Food Protein-Induced Proctitis/Proctocolitis: Autoimmunity Involvement?". J Immunol Res. 2015: 902863. doi:10.1155/2015/902863. PMC 4592904. PMID 26484355.
- ↑ Levinson, Warren E (2006). Review of Medical Microbiology and Immunology (9 ed.). McGraw-Hill Medical Publishing Division. p. 30. ISBN 978-0-07-146031-6. Retrieved February 27, 2012.
- ↑ Template:Rompalo AM. Chapter 9: Proctitis and Proctocolitis. In Klausner JD, Hook III EW. CURRENT Diagnosis & Treatment of Sexually Transmitted Diseases. McGraw Hill Professional; 2007
- ↑ Taraktchoglou M, Pacey AA, Turnbull JE, Eley A (2001). "Infectivity of Chlamydia trachomatis serovar LGV but not E is dependent on host cell heparan sulfate". Infect Immun. 69 (2): 968–76. doi:10.1128/IAI.69.2.968-976.2001. PMC 97976. PMID 11159992.
- ↑ Mabey D, Peeling RW (2002). "Lymphogranuloma venereum". Sex Transm Infect. 78 (2): 90–2. PMC 1744436. PMID 12081191.
- ↑ Moulder JW (1991). "Interaction of chlamydiae and host cells in vitro". Microbiol Rev. 55 (1): 143–90. PMC 372804. PMID 2030670 PMID 2030670 Check
|pmid=value (help). - ↑ Mounier, Joëlle; Vasselon, T; Hellio, R; Lesourd, M; Sansonetti, PJ (January 1992). "Shigella flexneri Enters Human Colonic Caco-2 Epithelial Cells through the Basolateral Pole". Infection and Immunity. 60 (1): 237–248. PMC 257528. PMID 1729185.
- ↑ 19.0 19.1 Capra JD, Kehoe JM (1974). "Variable region sequences of five human immunoglobulin heavy chains of the VH3 subgroup: definitive identification of four heavy chain hypervariable regions". Proc Natl Acad Sci U S A. 71 (3): 845–8. PMC 388111. PMID 4522793.
- ↑ 20.0 20.1 Espinosa-Cantellano M, Martínez-Palomo A (2000). "Pathogenesis of intestinal amebiasis: from molecules to disease". Clin Microbiol Rev. 13 (2): 318–31. PMC 100155. PMID 10756002.
- ↑ Müller FW, Franz A, Werries E (1988). "Secretory hydrolases of Entamoeba histolytica". J Protozool. 35 (2): 291–5. PMID 2456386.
- ↑ Spice WM, Ackers JP (1998). "The effects of Entamoeba histolytica lysates on human colonic mucins". J Eukaryot Microbiol. 45 (2): 24S–27S. PMID 9561780.
- ↑ 23.0 23.1 Surawicz CM, McFarland LV (1999). "Pseudomembranous colitis: causes and cures". Digestion. 60 (2): 91–100. doi:7633 Check
|doi=value (help). PMID 10095149. - ↑ Sarah A. Kuehne, Stephen T. Cartman, John T. Heap, Michelle L. Kelly, Alan Cockayne & Nigel P. Minton (2010). "The role of toxin A and toxin B inClostridium difficile infection". Nature. 467 (7316): 711–3. doi:10.1038/nature09397. PMID 20844489.
- ↑ Keith NM, Whelan M (1926). "A STUDY OF THE ACTION OF AMMONIUM CHLORID AND ORGANIC MERCURY COMPOUNDS". J Clin Invest. 3 (1): 149–202. doi:10.1172/JCI100072. PMC 434619. PMID 16693707.
- ↑ Bansal N, Soni A, Kaur P, Chauhan AK, Kaushal V (2016). "Exploring the Management of Radiation Proctitis in Current Clinical Practice". J Clin Diagn Res. 10 (6): XE01–XE06. doi:10.7860/JCDR/2016/17524.7906. PMC 4963751. PMID 27504391.
- ↑ Nelamangala Ramakrishnaiah VP, Krishnamachari S (2016). "Chronic haemorrhagic radiation proctitis: A review". World J Gastrointest Surg. 8 (7): 483–91. doi:10.4240/wjgs.v8.i7.483. PMC 4942748. PMID 27462390.
- ↑ 28.0 28.1 Do NL, Nagle D, Poylin VY (2011). "Radiation proctitis: current strategies in management". Gastroenterol Res Pract. 2011: 917941. doi:10.1155/2011/917941. PMC 3226317. PMID 22144997.
- ↑ 29.0 29.1 29.2 29.3 29.4 Abhishek K, Kaushik S, Kazemi MM, El-Dika S (2008). "An unusual case of hematochezia: acute ischemic proctosigmoiditis". J Gen Intern Med. 23 (9): 1525–7. doi:10.1007/s11606-008-0673-2. PMC 2518031. PMID 18521689.
- ↑ 30.0 30.1 Cai M, Zeng L, Li LJ, Mo LH, Xie RD, Feng BS; et al. (2016). "Specific immunotherapy ameliorates ulcerative colitis". Allergy Asthma Clin Immunol. 12: 37. doi:10.1186/s13223-016-0142-0. PMC 4975874. PMID 27499766.
- ↑ 31.0 31.1 Lopez J, Grinspan A (2016). "Fecal Microbiota Transplantation for Inflammatory Bowel Disease". Gastroenterol Hepatol (N Y). 12 (6): 374–9. PMC 4971820. PMID 27493597.
- ↑ 32.0 32.1 32.2 Loddo I, Romano C (2015). "Inflammatory Bowel Disease: Genetics, Epigenetics, and Pathogenesis". Front Immunol. 6: 551. doi:10.3389/fimmu.2015.00551. PMC 4629465. PMID 26579126.
- ↑ Tonolini M (2013). "Acute nonsteroidal anti-inflammatory drug-induced colitis". J Emerg Trauma Shock. 6 (4): 301–3. doi:10.4103/0974-2700.120389. PMC 3841543. PMID 24339669.
- ↑ Ravi S, Keat AC, Keat EC (1986). "Colitis caused by non-steroidal anti-inflammatory drugs". Postgrad Med J. 62 (730): 773–6. PMC 2418853. PMID 3774712.
- ↑ 35.0 35.1 West AB, Kuan SF, Bennick M, Lagarde S (1995). "Glutaraldehyde colitis following endoscopy: clinical and pathological features and investigation of an outbreak". Gastroenterology. 108 (4): 1250–5. PMID 7698592.
- ↑ Shih HY, Wu DC, Huang WT, Chang YY, Yu FJ (2011). "Glutaraldehyde-induced colitis: case reports and literature review". Kaohsiung J Med Sci. 27 (12): 577–80. doi:10.1016/j.kjms.2011.06.036. PMID 22208542.
- ↑ 37.0 37.1 37.2 Hwang JB, Hong J (2013). "Food protein-induced proctocolitis: Is this allergic disorder a reality or a phantom in neonates?". Korean J Pediatr. 56 (12): 514–8. doi:10.3345/kjp.2013.56.12.514. PMC 3885785. PMID 24416045.
- ↑ Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S (2007). "Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis". J Korean Med Sci. 22 (2): 213–7. doi:10.3346/jkms.2007.22.2.213. PMC 2693584. PMID 17449926.
- ↑ The Korean Academy of Medical Sciences. Allergic proctocolitis. http://dx.doi.org/10.3346/jkms.2007.22.2.213 Accessed on 31 August, 2016
- ↑ Wikipedia. Proctitis. https://en.wikipedia.org/wiki/Proctitis#/media/File:Radiation_proctitis3.jpg Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org/wiki/Pseudomembranous_colitis Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org Accessed on September 1, 2016
- ↑ Ulcerative colitis. Wikidoc. http://www.wikidoc.org/index.php/File:UC_granularity.png#filehistory Accessed on August 31, 2016
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID http://dx.doi.org/10.1016/S0022-3476(95)70540-6 Check
|pmid=value (help). - ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 837-8. ISBN 0-7216-0187-1}}
- ↑ Libre Pathology. https://librepathology.org/wiki/File:Ulcerative_colitis_(2)_active.jpg Accessed on September 1, 2016
- ↑ Libre Pathology. https://librepathology.org/wiki/File:Ulcerative_colitis_(2)_endoscopic_biopsy.jpg Accessed on September 1, 2016
- ↑ Wikipedia. Ischemic colitis. https://en.wikipedia.org/wiki/Ischemic_colitis#/media/File:Ischemic_colitis_-_high_mag.jpg Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org/wiki/File:Colonic_pseudomembranes_low_mag.jpg Accessed on September 1, 2016
- ↑ Mohan P, Ramakrishnan MK, Revathy S, Jayanthi V (2011). "Granulomatous colitis in oculocutaneous albinism". Dig Liver Dis. 43 (1): e1. doi:10.1016/j.dld.2009.09.006. PMID 19833565.
- ↑ Gié O, Clerc D, Giulieri S, Demartines N (2014). "[Clostridial colitis: diagnosis and strategies for management]". Rev Med Suisse. 10 (434): 1309–13. PMID 25073304.
- ↑ Elizur A, Cohen M, Goldberg MR, Rajuan N, Cohen A, Leshno M; et al. (2012). "Cow's milk associated rectal bleeding: a population based prospective study". Pediatr Allergy Immunol. 23 (8): 766–70. doi:10.1111/pai.12009. PMID 23050491.
- ↑ 53.0 53.1 Arvola T, Ruuska T, Keränen J, Hyöty H, Salminen S, Isolauri E (2006). "Rectal bleeding in infancy: clinical, allergological, and microbiological examination". Pediatrics. 117 (4): e760–8. doi:10.1542/peds.2005-1069. PMID 16585287.
- ↑ 54.0 54.1 Xanthakos SA, Schwimmer JB, Melin-Aldana H, Rothenberg ME, Witte DP, Cohen MB (2005). "Prevalence and outcome of allergic colitis in healthy infants with rectal bleeding: a prospective cohort study". J Pediatr Gastroenterol Nutr. 41 (1): 16–22. PMID 15990624.
- ↑ Lake AM (2000). "Food-induced eosinophilic proctocolitis". J Pediatr Gastroenterol Nutr. 30 Suppl: S58–60. PMID 10634300.
- ↑ 56.0 56.1 Shivananda S, Peña AS, Mayberry JF, Ruitenberg EJ, Hoedemaeker PJ (1987). "Epidemiology of proctocolitis in the region of Leiden, The Netherlands. A population study from 1979 to 1983". Scand J Gastroenterol. 22 (8): 993–1002. PMID 3685885.
- ↑ 57.0 57.1 57.2 Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID /10.1155/2011/917941 Check
|pmid=value (help). - ↑ Bharucha AE, Tremaine WJ, Johnson CD, Batts KP (1996). "Ischemic proctosigmoiditis". Am J Gastroenterol. 91 (11): 2305–9. PMID 8931407.
- ↑ Gallegos M, Bradly D, Jakate S, Keshavarzian A (2012). "Lymphogranuloma venereum proctosigmoiditis is a mimicker of inflammatory bowel disease". World J Gastroenterol. 18 (25): 3317–21. doi:10.3748/wjg.v18.i25.3317. PMC 3391771. PMID 22783058.
- ↑ de Voux A, Kent JB, Macomber K, Krzanowski K, Jackson D, Starr T; et al. (2016). "Notes from the Field: Cluster of Lymphogranuloma Venereum Cases Among Men Who Have Sex with Men - Michigan, August 2015-April 2016". MMWR Morb Mortal Wkly Rep. 65 (34): 920–1. doi:10.15585/mmwr.mm6534a6. PMID 27583686.
- ↑ 61.0 61.1 Workowski KA, Berman S, Centers for Disease Control and Prevention (CDC) (2010). "Sexually transmitted diseases treatment guidelines, 2010". MMWR Recomm Rep. 59 (RR-12): 1–110. PMID 21160459.
- ↑ Williams D, Churchill D (2006). "Ulcerative proctitis in men who have sex with men: an emerging outbreak". BMJ. 332 (7533): 99–100. doi:10.1136/bmj.332.7533.99. PMC 1326936. PMID 16410585.
- ↑ Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S; et al. (2012). "Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines". J Pediatr Gastroenterol Nutr. 55 (2): 221–9. doi:10.1097/MPG.0b013e31825c9482. PMID 22569527.
![Radiation Proctitis[40]](/images/0/01/Radiation_proctitis3.jpg)
![Pseudomembranous colitis. (WC) [41]](/images/a/a1/Pseudomembranous_colitis.JPG)
![Pseudomembranous colitis. [42]](/images/c/c1/800px-Pseudomembranous_Colitis%2C_Colectomy_%28Gross%29_%287410584264%29.jpg)
![Ulcerative colitis.[43]](/images/c/cf/UC_granularity.png)
![Ulcerative colitis. H&E staining showing crypt abscess, a characteristic finding in ulcerative colitis [46]](/images/2/2e/Ulcerative_colitis_%282%29_active.jpg)
![Ulcerative colitis. H&E stain showing marked lymphocytic infiltration (blue/purple) of the intestinal mucosa and distortion of the architecture of the crypts. [47]](/images/0/02/Ulcerative_colitis_%282%29_endoscopic_biopsy.jpg)
![Ischemic colitis. H&E staining showing changes seen in ischemic colitis [48]](/images/f/f2/Ischemic_colitis.JPG)
![Pseudomembranous colitis. H& E staining showing pseudomembranes in Clostridium colitis [49]](/images/0/09/1440px-Colonic_pseudomembranes_low_mag.jpg)