Quinolone
|
WikiDoc Resources for Quinolone |
|
Articles |
|---|
|
Most recent articles on Quinolone |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Quinolone at Clinical Trials.gov Clinical Trials on Quinolone at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Quinolone
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Quinolone Discussion groups on Quinolone Directions to Hospitals Treating Quinolone Risk calculators and risk factors for Quinolone
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Quinolone |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |


Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
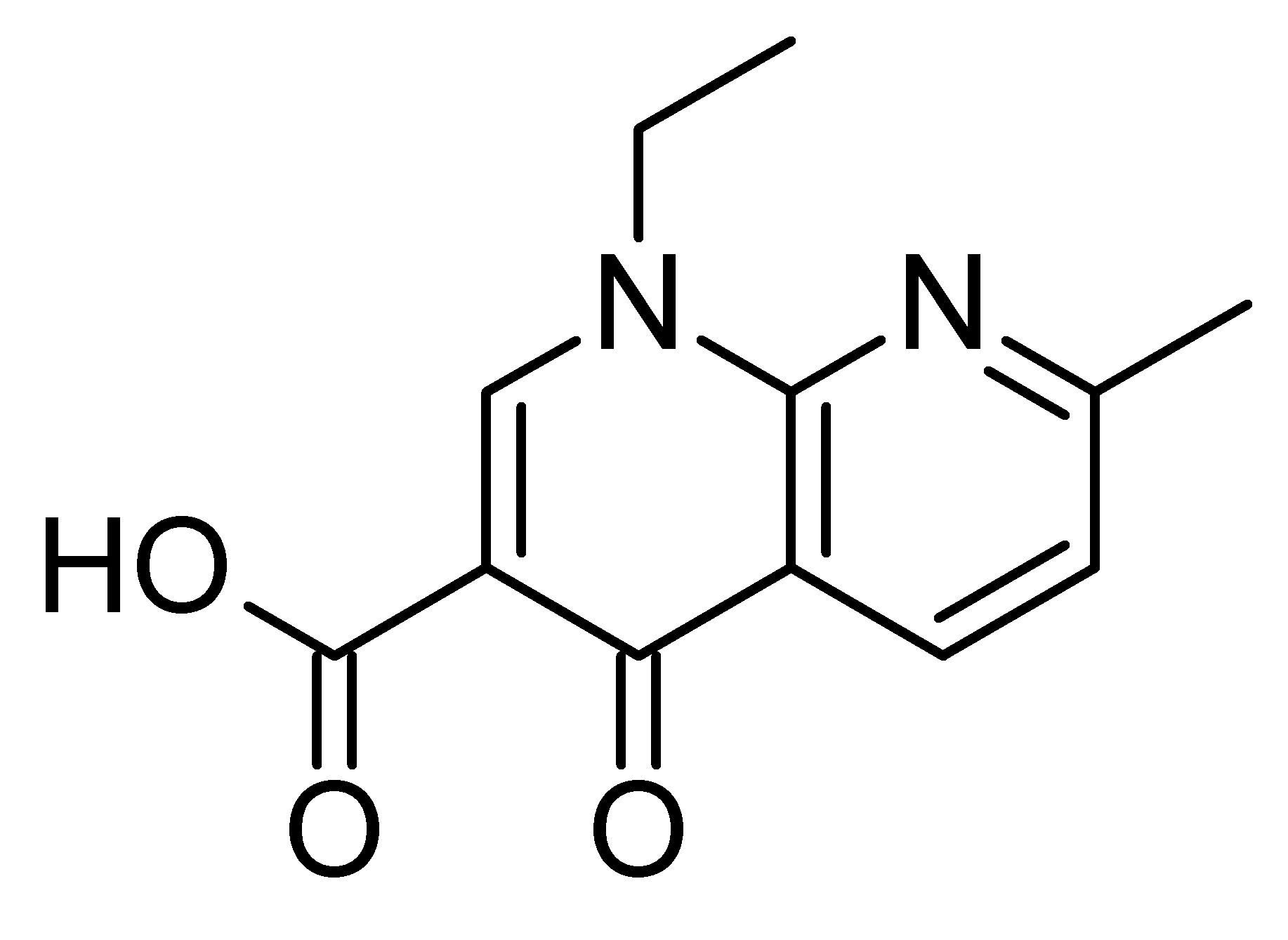
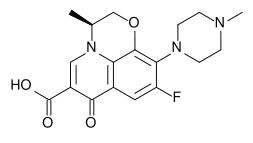
The quinolones are a family of broad-spectrum antibiotics. The parent of the group is nalidixic acid. The majority of quinolones in clinical use belong to the subset of fluoroquinolones, which have a fluoro group attached the central ring system, typically at the 6-position.
Mechanism
Quinolones and fluoroquinolones are bactericidal drugs, actively killing bacteria. Quinolones inhibit the bacterial DNA gyrase or the topoisomerase IV enzyme, thereby inhibiting DNA replication and transcription. Quinolones can enter cells easily and therefore are often used to treat intracellular pathogens such as Legionella pneumophila and Mycoplasma pneumoniae. For many gram-negative bacteria DNA gyrase is the target, whereas topoisomerase IV is the target for many gram-positive bacteria. Eukaryotic cells do not contain DNA gyrase or topoisomerase IV.
Adverse effects
Quinolone antibiotics were once considered relatively safe, but several side-effects have become evident with experience. For example, numerous case reports have implicated their use since 1965 in spontaneous tendon ruptures or damage, especially with the concurrent use of a systemic corticosteroid. In the fall of 2004, the Food and Drug Administration upgraded the warnings found within the package inserts for all drugs within this class regarding such serious adverse reactions. It is important to note, however, that the incidence of this is quite rare, with occurrences at less than one per ten thousand person-years.[1]
- Peripheral neuropathy (nerve damage): "Rare cases of sensory or sensor motor axonal polyneuropathy affecting small and or large axons resulting in paresthesias, hypoaesthesias, dysesthesias, and weakness have been reported in patients taking quinolones. Therapy should be discontinued if the patient experiences symptoms of neuropathy, including pain, burning, tingling, numbness and/or weakness, or is found to have deficits in light touch, pain, temperature, position sense, vibratory sensation, and/or motor strength in order to prevent the development of an irreversible condition."
- Tendon damage: "Ruptures of the shoulder, hand, Achilles tendon, or other tendons that require surgical repair or resulted in prolonged disability have been reported in patients receiving quinolones. Post-marketing surveillance reports indicate that this risk may be increased in patients receiving concomitant corticosteroids, especially the elderly. Fluoroquinolone therapy should be discontinued if the patient experiences pain, inflammation, or rupture of a tendon. Patients should rest and refrain from exercise until diagnosis of tendinitis or tendon rupture had been excluded. Tendon rupture can occur during or after therapy with quinolones."
Other problems include:
- Heart problems (prolonged QT Interval / Torsades de pointes)
- Pseudomembranous colitis
- Rhabdomyolysis (breakdown of muscle tissue)
- Stevens-Johnson syndrome
- Lowered seizure threshold
- Hypoglycemia
- Kidney stones due to loss of Oxalobacter formigenes[2]
Resistance
Resistance to quinolones can develop rapidly, even during a course of treatment. Numerous pathogens, including Staphylococcus aureus, enterococci, and Streptococcus pyogenes now exhibit resistance worldwide.[3] Widespread veterinary usage of quinolones, in particular in Europe, has been implicated.
There are three known mechanisms of resistance.[4] Efflux pumps can be used to decrease intracellular drug concentration. In gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase, protecting it from the action of quinolones. Finally, mutations at key sites in DNA gyrase or topoisomerase IV can decrease their binding affinity to quinolones, decreasing the drug effectiveness.
Generations
The quinolones are divided into generations based on their antibacterial spectrum. The earlier generation agents are, in general, more narrow spectrum than the later ones.
1st generation
- cinoxacin (Cinoxacin®)
- flumequine (Flubactin®) (Veterinary use)
- nalidixic acid (NegGam®, Wintomylon®)
- oxolinic acid
- piromidic acid
- pipemidic acid (Dolcol®)
2nd generation
- ciprofloxacin (Ciprobay®, Cipro®, Ciproxin®)
- enoxacin (Enroxil®, Penetrex®)
- fleroxacin (Megalone®) (withdrawn)
- lomefloxacin (Maxaquin®)
- nadifloxacin
- norfloxacin (Lexinor®, Noroxin®, Quinabic®, Janacin®)
- ofloxacin (Floxin®, Oxaldin®, Tarivid®)
- pefloxacin
- rufloxacin (Uroflox®)
3rd generation
- balofloxacin
- grepafloxacin (Raxar®) (withdrawn)
- levofloxacin (Cravit®, Levaquin®)
- pazufloxacin Mesilate
- sparfloxacin (Zagam®)
- temafloxacin (Omniflox®) (withdrawn)
- tosufloxacin
4th generation
- clinafloxacin
- gemifloxacin (Factive®)
- moxifloxacin (Avelox®)
- gatifloxacin (Tequin® (withdrawn), Zymar®)
- sitafloxacin
- trovafloxacin (Trovan®) (withdrawn)
In development
- ecinofloxacin
- prulifloxacin
Veterinary use
The quinolones have been widely used in agriculture and several agents exist which have veterinary but not human use.
- danofloxacin (Advocin, Advocid) (for veterinary use)
- difloxacin (Dicural, Vetequinon)
- enrofloxacin (Baytril) (for veterinary use)
- marbofloxacin (Marbocyl, Zenequin) (for veterinary use)
- orbifloxacin (Orbax, Victas) (for veterinary use)
- sarafloxacin (Floxasol, Saraflox, Sarafin) (for veterinary use)
External links
- Fact Sheet: Quinolones
- The Flox Report An investigative approach to the true toxicity of quinolone antibiotics.
- Research on Adverse Effects of Fluoroquinolones
- Fluoroquinolone-Induced Tendinopathy: What do we know? Richard M. Harrell, MD.
- Fluoroquinolones "Family Practice Notebook" entry page for Fluoroquinolones
- Structure Activity Relationships "Antibacterial Agents; Structure Activity Relationships," André Bryskier MD
References
- ↑ Maury M. Breecher, PhD, MPH (October 17, 2003). "IDSA: Achilles Tendon Rupture after use of antibiotics". Doctor's Guide, Global Edition.
- ↑ [1] - Interim reference; cites Troxel SA, Low RK. Intestinal Oxalobacter Formigenes Colonization Urinary Oxalate Levels in Calcium Oxalate Stone Formers. Journal of Urology 165:245A, 2001. (Please replace with that citation if the full text of the article agrees with the linked summary)
- ↑ M Jacobs, Worldwide Overview of Antimicrobial Resistance. International Symposium on Antimicrobial Agents and Resistance 2005.
- ↑ A Robicsek, GA Jacoby and DC Hooper, The worldwide emergence of plasmid-mediated quinolone resistance. 2006. The Lancet Infectious Diseases 6-10:629-640
de:Fluorchinolone eu:Kinolona fo:Quinolon it:Chinoloni nl:Fluoroquinolone no:Quinoloner sk:Chinolón