Colitis: Difference between revisions
Qasim Salau (talk | contribs) No edit summary |
Tarek Nafee (talk | contribs) No edit summary |
||
| Line 74: | Line 74: | ||
* Immune mediated colitis is the experimental name in animal studies of ulcerative colitis. It is a synonym of ulcerative colitis, but it should not be used as a synonym when referring to ulcerative colitis. | * Immune mediated colitis is the experimental name in animal studies of ulcerative colitis. It is a synonym of ulcerative colitis, but it should not be used as a synonym when referring to ulcerative colitis. | ||
== | == Images == | ||
===Gross pathology=== | ===Gross pathology=== | ||
| Line 522: | Line 517: | ||
* [[Colonoscopy]] | * [[Colonoscopy]] | ||
Additional tests include [[stool culture]]s and [[blood test]]s, including blood chemistry tests. A high [[erythrocyte sedimentation rate]] (ESR) is one typical finding in acute | Additional tests include [[stool culture]]s and [[blood test]]s, including blood chemistry tests. A high [[erythrocyte sedimentation rate]] (ESR) is one typical finding in acute exacerbation of colitis. | ||
==References== | ==References== | ||
Revision as of 17:16, 17 January 2017
|
Colitis Microchapters |
For patient information on this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: M.Umer Tariq [2]; Maham Khan [3]; Ogheneochuko Ajari, MB.BS, MS [4]; Rim Halaby, M.D. [5]; Qasim Salau, M.B.B.S., FMCPaed [6]
Synonyms and keywords: Colitis, Proctocolitis, Proctitis, Enterocolitis.
Overview
Colitis is the inflammation of the colon, that can be either acute or chronic. Causes of colitis include infectious causes such as Chlamydia trachomatis, Neisseria gonorrhoeae, Shigella dysenteriae, HSV, allergy (food potein-induced proctocolitis) and radiation. Colitis may co-exist with enteritis (inflammation of the small bowel), proctitis (inflammation of the rectum) or both. The mainstay of therapy for infectious proctocolitis is antimicrobial therapy. The preferred regimen is a combination of Ceftriaxone and Doxycycline.
Classification
There is no established classification system for colitis. However, it may be classified based on etiology, age and duration of symptom.
Classification by etiology
| Classes of Colitis | Disorders |
| Autoimmune | |
| Allergic | |
| Infectious colitis |
|
| Idiopathic | |
| Iatrogenic | |
| Vascular | |
| Drug induced | |
| Unclassifiable |
|
Classification by Anatomy
Colitis may co-exist with inflammation involving other parts of the gastrointestinal tract. It can be classified based on anatomy into;
- Proctitis: When it involves the rectum
- Colitis: When it involves the inflammation is limited to the colon
- Proctocolitis: When it involves the rectum and colon (usually the distal part of the colon 12cm to 15cm above the anus (sigmoid colon)[1][2]
- Enterocolitis: When it involves the small intestine in addition to the colon
Schematic of Anatomical Classification of Colitis
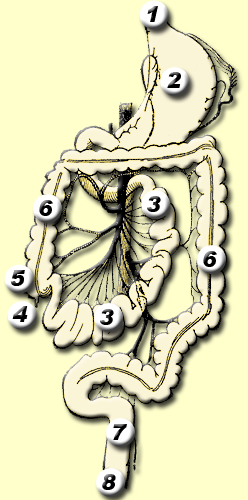
*Regions 4 to 6: Enterocolitis
*Region 6: Colitis
*Regions 6 to 8: Proctocolitis
*Regions 7 to 8:Proctitis
Classification by Age
Classification by duration of symptoms
Notes:
- Fulminant colitis is any colitis with a rapid downhill clinical course; in addition to the diarrhea, fever, and anemia seen in colitis, the patient has severe abdominal pain and presents a clinical picture similar to that of septicemia, where shock is present.
- Irritable bowel syndrome, a separate disease, has been called spastic colitis or spastic colon. This name causes confusion, since colitis is not a feature of irritable bowel syndrome.
- Immune mediated colitis is the experimental name in animal studies of ulcerative colitis. It is a synonym of ulcerative colitis, but it should not be used as a synonym when referring to ulcerative colitis.
Images
Gross pathology
-
Allergic proctocolitis[8]
-
Radiation Proctitis[9]
-
Pseudomembranous colitis. (WC) [10]
-
Pseudomembranous colitis. [11]
-
Ulcerative colitis.[12]
Microscopic pathology
-
Ulcerative colitis. H&E staining showing crypt abscess, a characteristic finding in ulcerative colitis [13]
-
Ulcerative colitis. H&E stain showing marked lymphocytic infiltration (blue/purple) of the intestinal mucosa and distortion of the architecture of the crypts. [14]
-
Ischemic colitis. H&E staining showing changes seen in ischemic colitis [15]
-
Pseudomembranous colitis. H& E staining showing pseudomembranes in Clostridium colitis [16]
Differentiating Colitis from Other Diseases
Causes of colitis are diverse and may overlap with other disease. The differential diagnosis of colitis can be classified into two according to age group.
Differential diagnosis in Infants
- Swallowed maternal blood syndrome
- Anorectal fissure
- Necrotizing enterocolitis especially in preterm babies
- Vitamin K dependent hemorrhage
- Other Coagulopathies: (hereditary such as coagulation factor deficiency or acquired such as disseminated intravascular coagulopathy)
- Food protein-induced enterocolitis
- Intussusception
- Gastrointestinal Infections
- Meckel diverticulum
- Intestinal duplication cysts
- Vascular malformations
- Inflammatory bowel disease(early onset)
- Hirschsprung disease complicated by enterocolitis
- Volvolus
- Gastro-duodenal ulcers
- Gastrointestinal duplication cyst
- Liver disease with clotting factor deficiency
- Lymphonodular hyperplasia
Differential diagnosis in Infants
- Colorectal malignancy
- Crohn's disease
- Behcet's disease
- Arteriovenous malformation
- Diverticuclosis
- Infection
- Coagulopathy
- Systemic lupus erythematosus(SLE)
Differentiating between different forms of colitis
- The symptoms of colitis such as diarrhea especially bloody diarrhea and abdominal pain are seen are seen in all forms of colitis. The table below lists the differential diagnosis of common causes of colitis:[17][18]
| Diseases | History and Symptoms | Physical Examination | Laboratory findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diarrhea | Rectal bleeding | Abdominal pain | Atopy | Dehydration | Fever | Hypotension | Malnutrition | Blood in stool (frank or occult) | Microorganism in stool | Pseudomembranes on endoscopy | ||
| Allergic Colitis | + | ++ | + | ++ | ++ | |||||||
| Chemical colitis | + | ++ | ++ | + | + | ++ | + | |||||
| Infectious colitis | ++ | ++ | ++ | +++ | +++ | ++ | + | ++ | ++ | + | ||
| Radiation colitis | + | ++ | + | + | + | ++ | ||||||
| Ischemic colitis | + | + | ++ | + | + | + | + | ++ | ||||
| Drug-induced colitis | + | + | ++ | + | ++ | + | ||||||
Causes
Common Causes
Common causes of Proctocolitis include infectious agents such as Chlamydia trachomatis (which causes LGV (Lymphogranuloma Venereum), Neisseria gonorrhoeae, HSV, Shigella dysenteriae and Campylobacter species. It can also be allergic (for example food protein-induced proctocolitis), idiopathic (for example microscopic colitis), vascular (for example ischemic colitis), or autoimmune (for example inflammatory bowel disease).
Causes by Organ System
Causes in Alphabetical Order
Life Threatening Causes
Example include toxic megacolon, ischemic colitis, infectious colitis such as escherichia coli O157:H7 and shigella.
Diagnosis
Symptoms
Physical Examination
Diagnostic Tests
Colitis is associated with the following findings:
- Swelling of the colon tissue
- Bleeding
- Erythema (redness) of the surface of the colon
- Ulcerations of the colon
Common tests which reveal these signs include:
- X-rays of the colon
- Testing the stool for blood and pus
- Sigmoidoscopy
- Colonoscopy
Additional tests include stool cultures and blood tests, including blood chemistry tests. A high erythrocyte sedimentation rate (ESR) is one typical finding in acute exacerbation of colitis.
References
- ↑ 2015 Sexually Transmitted Diseases Treatment Guidelines. Centers for Disease Control and Prevention (2015).http://www.cdc.gov/std/tg2015/proctitis.htm Accessed on August 29, 2016
- ↑ Hamlyn E, Taylor C (2006). "Sexually transmitted proctitis". Postgrad Med J. 82 (973): 733–6. doi:10.1136/pmj.2006.048488. PMC 2660501. PMID 17099092.
- ↑ WikiMedia Commons https://commons.wikimedia.org/wiki/File:Gastro-intestinal_tract.png. Accessed on September 09, 2016
- ↑ Nowak-Węgrzyn A (2015). "Food protein-induced enterocolitis syndrome and allergic proctocolitis". Allergy Asthma Proc. 36 (3): 172–84. doi:10.2500/aap.2015.36.3811. PMC 4405595. PMID 25976434.
- ↑ Pumberger W, Pomberger G, Geissler W (2001). "Proctocolitis in breast fed infants: a contribution to differential diagnosis of haematochezia in early childhood". Postgrad Med J. 77 (906): 252–4. PMC 1741985. PMID 11264489.
- ↑ Alfadda AA, Storr MA, Shaffer EA (2011). "Eosinophilic colitis: epidemiology, clinical features, and current management". Therap Adv Gastroenterol. 4 (5): 301–9. doi:10.1177/1756283X10392443. PMC 3165205. PMID 21922029.
- ↑ 7.0 7.1 Hauer-Jensen M, Denham JW, Andreyev HJ (2014). "Radiation enteropathy--pathogenesis, treatment and prevention". Nat Rev Gastroenterol Hepatol. 11 (8): 470–9. doi:10.1038/nrgastro.2014.46. PMC 4346191. PMID 24686268.
- ↑ The Korean Academy of Medical Sciences. Allergic proctocolitis. http://dx.doi.org/10.3346/jkms.2007.22.2.213 Accessed on 31 August, 2016
- ↑ Wikipedia. Proctitis. https://en.wikipedia.org/wiki/Proctitis#/media/File:Radiation_proctitis3.jpg Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org/wiki/Pseudomembranous_colitis Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org Accessed on September 1, 2016
- ↑ Ulcerative colitis. Wikidoc. http://www.wikidoc.org/index.php/File:UC_granularity.png#filehistory Accessed on August 31, 2016
- ↑ Libre Pathology. https://librepathology.org/wiki/File:Ulcerative_colitis_(2)_active.jpg Accessed on September 1, 2016
- ↑ Libre Pathology. https://librepathology.org/wiki/File:Ulcerative_colitis_(2)_endoscopic_biopsy.jpg Accessed on September 1, 2016
- ↑ Wikipedia. Ischemic colitis. https://en.wikipedia.org/wiki/Ischemic_colitis#/media/File:Ischemic_colitis_-_high_mag.jpg Accessed on August 31, 2016
- ↑ Libre Pathology. Pseudomembranous colitis. https://librepathology.org/wiki/File:Colonic_pseudomembranes_low_mag.jpg Accessed on September 1, 2016
- ↑ Thielman NM, Guerrant RL (2004). "Clinical practice. Acute infectious diarrhea". N Engl J Med. 350 (1): 38–47. doi:10.1056/NEJMcp031534. PMID 14702426.
- ↑ Khan AM, Faruque AS, Hossain MS, Sattar S, Fuchs GJ, Salam MA (2004). "Plesiomonas shigelloides-associated diarrhoea in Bangladeshi children: a hospital-based surveillance study". J Trop Pediatr. 50 (6): 354–6. doi:10.1093/tropej/50.6.354. PMID 15537721.
- ↑ Mohan P, Ramakrishnan MK, Revathy S, Jayanthi V (2011). "Granulomatous colitis in oculocutaneous albinism". Dig Liver Dis. 43 (1): e1. doi:10.1016/j.dld.2009.09.006. PMID 19833565.
- ↑ Gié O, Clerc D, Giulieri S, Demartines N (2014). "[Clostridial colitis: diagnosis and strategies for management]". Rev Med Suisse. 10 (434): 1309–13. PMID 25073304.
![Radiation Proctitis[9]](/images/0/01/Radiation_proctitis3.jpg)
![Pseudomembranous colitis. (WC) [10]](/images/a/a1/Pseudomembranous_colitis.JPG)
![Pseudomembranous colitis. [11]](/images/c/c1/800px-Pseudomembranous_Colitis%2C_Colectomy_%28Gross%29_%287410584264%29.jpg)
![Ulcerative colitis.[12]](/images/c/cf/UC_granularity.png)
![Ulcerative colitis. H&E staining showing crypt abscess, a characteristic finding in ulcerative colitis [13]](/images/2/2e/Ulcerative_colitis_%282%29_active.jpg)
![Ulcerative colitis. H&E stain showing marked lymphocytic infiltration (blue/purple) of the intestinal mucosa and distortion of the architecture of the crypts. [14]](/images/0/02/Ulcerative_colitis_%282%29_endoscopic_biopsy.jpg)
![Ischemic colitis. H&E staining showing changes seen in ischemic colitis [15]](/images/f/f2/Ischemic_colitis.JPG)
![Pseudomembranous colitis. H& E staining showing pseudomembranes in Clostridium colitis [16]](/images/0/09/1440px-Colonic_pseudomembranes_low_mag.jpg)