Addison's disease laboratory findings: Difference between revisions
| Line 40: | Line 40: | ||
** Mild non–anion-gap [[metabolic acidosis]] | ** Mild non–anion-gap [[metabolic acidosis]] | ||
* Serum [[cortisol]] - decreased (<25mcg/dL) | * Serum [[cortisol]] - decreased (<25mcg/dL) | ||
* Urine and sweat [[sodium]] - elevated | |||
* Elevated [[BUN]] and [[creatinine]] - when [[hypovolemia]] is the cause. | |||
==References== | ==References== | ||
Revision as of 14:56, 13 August 2012
|
Addison's disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Addison's disease laboratory findings On the Web |
|
American Roentgen Ray Society Images of Addison's disease laboratory findings |
|
Risk calculators and risk factors for Addison's disease laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Laboratory Findings
A diagnosis of Addison's disease is made by laboratory tests. The aim of these tests is first to determine whether levels of cortisol are insufficient and then to establish the cause. X-ray exams of the adrenal and pituitary glands also are useful in helping to establish the cause. In its early stages, adrenal insufficiency can be difficult to diagnose. A review of a patient's medical history based on the symptoms, especially the dark tanning of the skin, will lead a doctor to suspect Addison's disease.
In suspected cases of Addison's disease, one needs to demonstrate that adrenal hormone levels are low even after appropriate stimulation with synthetic pituitary hormone tetracosactide. Two tests are performed, the short and the long test.
The short test compares blood cortisol levels before and after 250 micrograms of tetracosactide (IM/IV) is given. If, one hour later, plasma cortisol exceeds 170 nmol/L and has risen by at least 330 nmol/L to at least 690 nmol/L, adrenal failure is excluded. If the short test is abnormal, the long test is used to differentiate between primary adrenal failure and secondary adrenocortical failure.
The long test uses 1 mg tetracosactide (IM). Blood is taken 1, 4, 8, and 24 hours later. Normal plasma cortisol level should reach 1000 nmol/L by 4 hours. In primary Addison's disease, the cortisol level is reduced at all stages whereas in secondary corticoadrenal insufficiency, a delayed but normal response is seen.
Other tests that may be performed to distinguish between various causes of hypoadrenalism are renin and adrenocorticotropic hormone levels, as well as medical imaging - usually in the form of ultrasound, computed tomography or magnetic resonance imaging (MRI).
ACTH Stimulation Test
This is the most specific test for diagnosing Addison's disease. In this test, blood cortisol, urine cortisol, or both are measured before and after a synthetic form of ACTH is given by injection. In the so-called short, or rapid, ACTH test, measurement of cortisol in blood is repeated 30 to 60 minutes after an intravenous ACTH injection. The normal response after an injection of ACTH is a rise in blood and urine cortisol levels. Patients with either form of adrenal insufficiency respond poorly or do not respond at all.
CRH Stimulation Test
When the response to the short ACTH test is abnormal, a "long" CRH stimulation test is required to determine the cause of adrenal insufficiency. In this test, synthetic CRH is injected intravenously and blood cortisol is measured before and 30, 60, 90, and 120 minutes after the injection. Patients with primary adrenal insufficiency have high ACTHs but do not produce cortisol. Patients with secondary adrenal insufficiency have deficient cortisol responses but absent or delayed ACTH responses. Absent ACTH response points to the pituitary as the cause; a delayed ACTH response points to the hypothalamus as the cause.
In patients suspected of having an addisonian crisis, the doctor must begin treatment with injections of salt, fluids, and glucocorticoid hormones immediately. Although a reliable diagnosis is not possible while the patient is being treated for the crisis, measurement of blood ACTH and cortisol during the crisis and before glucocorticoids are given is enough to make the diagnosis. Once the crisis is controlled and medication has been stopped, the doctor will delay further testing for up to 1 month to obtain an accurate diagnosis.
Suggestive features
Routine investigations may show:
- Complete blood count and differential count - Eosinophilia and lymphocytosis (increased number of eosinophils or lymphocytes, two types of white blood cells)
- Hypoglycemia, low blood sugar (worse in children)
- Serum electrolytes:
- Hyponatraemia (low blood sodium levels)
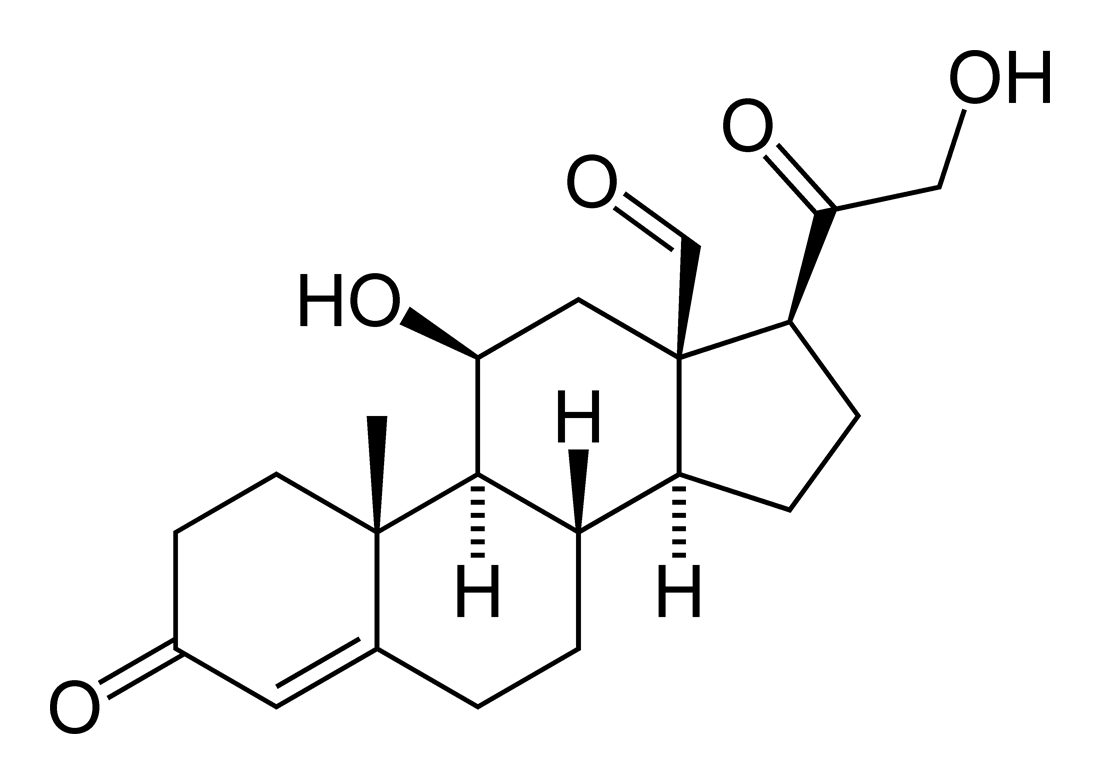
- Hyperkalemia (raised blood potassium levels), due to loss of production of the hormone aldosterone
- Mild hypercalcemia - in 20% patients
- Mild non–anion-gap metabolic acidosis
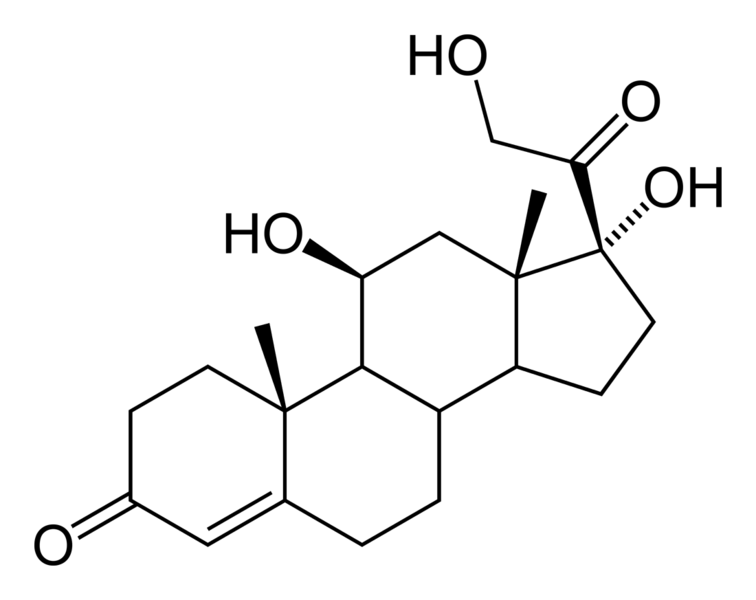
- Serum cortisol - decreased (<25mcg/dL)
- Urine and sweat sodium - elevated
- Elevated BUN and creatinine - when hypovolemia is the cause.