Psoriasis
| Psoriasis | |
 | |
|---|---|
| A young man whose back and arms are affected by psoriasis. | |
| ICD-10 | L40 |
| ICD-9 | 696 |
| OMIM | 177900 |
| DiseasesDB | 10895 |
| MedlinePlus | 000434 |
| MeSH | D011565 |
|
Psoriasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Psoriasis On the Web |
|
American Roentgen Ray Society Images of Psoriasis |
For patient information, click Psoriasis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5] Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [6]
Overview
Etiology
The cause of psoriasis is not known, but it is believed to have a genetic component. Several factors are thought to aggravate psoriasis. These include stress, excessive alcohol consumption, and smoking. Individuals with psoriasis may suffer from depression and loss of self-esteem. As such, quality of life is an important factor in evaluating the severity of the disease. There are many treatments available but because of its chronic recurrent nature psoriasis is a challenge to treat.
Historical Perspective
Classification
Diagnosis
A diagnosis of psoriasis is usually based on the appearance of the skin. There are no special blood tests or diagnostic procedures for psoriasis. Sometimes a skin biopsy, or scraping, may be needed to rule out other disorders and to confirm the diagnosis. Skin from a biopsy will show clubbed Rete pegs if positive for psoriasis.
Physical Examination
Skin
Severity

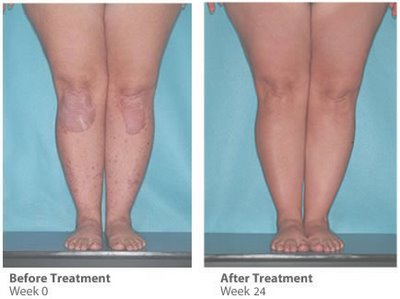
Psoriasis is usually graded as mild (affecting less than 3% of the body), moderate (affecting 3-10% of the body) or severe. Several scales exist for measuring the severity of psoriasis.
The degree of severity is generally based on the following factors: the proportion of body surface area affected; disease activity (degree of plaque redness, thickness and scaling); response to previous therapies; and the impact of the disease on the person.
The Psoriasis Area Severity Index (PASI) is the most widely used measurement tool for psoriasis. PASI combines the assessment of the severity of lesions and the area affected into a single score in the range 0 (no disease) to 72 (maximal disease).[2]
Nevertheless, the PASI can be too unwieldy to use outside of trials, which has led to attempts to simplify the index for clinical use.[3]
Effect on the quality of life
Psoriasis has been shown to affect health-related quality of life to an extent similar to the effects of other chronic diseases such as depression, myocardial infarction, hypertension, congestive heart failure or type 2 diabetes. Depending on the severity and location of outbreaks, individuals may experience significant physical discomfort and some disability. Itching and pain can interfere with basic functions, such as self-care, walking, and sleep. Plaques on hands and feet can prevent individuals from working at certain occupations, playing some sports, and caring for family members or a home. The frequency of medical care is costly and can interfere with an employment or school schedule.
Individuals with psoriasis may also feel self-conscious about their appearance and have a poor self-image that stems from fear of public rejection and psychosexual concerns. Psychological distress can lead to significant depression and social isolation.
Epidemiology
Psoriasis affects both sexes equally and can occur at any age, although it most commonly appears for the first time between the ages of 15 and 25 years.
The prevalence of psoriasis in Western populations is estimated to be around 2-3%. A survey [7] conducted by the National Psoriasis Foundation (a US based psoriasis education and advocacy group, which is partly funded by pharmaceutical companies) found a prevalence of 2.1% among adult Americans. The study also found that 35% of people with psoriasis could be classified as having moderate to severe psoriasis.
Around one-third of people with psoriasis report a family history of the disease, and researchers have identified genetic loci associated with the condition. Studies of monozygotic twins suggest a 70% chance of a twin developing psoriasis if the other twin has psoriasis. The concordance is around 20% for dizygotic twins. These findings suggest both a genetic predisposition and an environmental response in developing psoriasis.[4]
Onset before age 40 usually indicates a greater genetic susceptibility and a more severe or recurrent course of psoriasis.
Cause
The cause of psoriasis is not fully understood. There are two main hypotheses about the process that occurs in the development of the disease. The first considers psoriasis as primarily a disorder of excessive growth and reproduction of skin cells. The problem is simply seen as a fault of the epidermis and its keratinocytes. The second hypothesis sees the disease as being an immune-mediated disorder in which the excessive reproduction of skin cells is secondary to factors produced by the immune system. T cells (which normally help protect the body against infection) become active, migrate to the dermis and trigger the release of cytokines (tumor necrosis factor-alpha TNFα, in particular) which cause inflammation and the rapid production of skin cells. It is not known what initiates the activation of the T cells.
The immune-mediated model of psoriasis has been supported by the observation that immunosuppressant medications can clear psoriasis plaques. However, the role of the immune system is not fully understood, and it has recently been reported that an animal model of psoriasis can be triggered in mice lacking T cells.[5] Animal models, however, reveal only a few aspects resembling human psoriasis.
Psoriasis is a fairly idiosyncratic disease. The majority of people's experience of psoriasis is one in which it may worsen or improve for no apparent reason. Studies of the factors associated with psoriasis tend to be based on small (usually hospital based) samples of individuals. These studies tend to suffer from representative issues, and an inability to tease out causal associations in the face of other (possibly unknown) intervening factors. Conflicting findings are often reported. Nevertheless, the first outbreak is sometimes reported following stress (physical and mental), skin injury, and streptococcal infection. Conditions that have been reported as accompanying a worsening of the disease include infections, stress, and changes in season and climate. Certain medicines, including lithium salt and beta blockers, have been reported to trigger or aggravate the disease. Excessive alcohol consumption, smoking and obesity may exacerbate psoriasis or make the management of the condition difficult.[6][7]
Individuals suffering from the advanced effects of the Human immunodeficiency virus, or HIV, often exhibit psoriasis.[8] This presents a paradox to researchers as traditional therapies that reduce T-cell counts generally cause psoriasis to improve. Yet, as CD4-T-cell counts decrease with the progression of HIV, psoriasis worsens.[9] In addition, HIV is typically characterized by a strong Th2 cytokine profile, whereas psoriasis vulgaris is characterized by a strong Th1 secretion pattern.[10] It's hypothesized that the diminished CD4-T-Cell presence causes an over-activation of CD8-T-Cells, which are responsible for the exacerbation of psoriasis in HIV positive patients. It is important to remember that most individuals with psoriasis are otherwise healthy and the presence of HIV accounts for less than 1% of cases. The prevalence of psoriasis in the HIV positive population ranges from 1 to 6 percent, which is about 3 times higher than the normal population.[11]
Psoriasis occurs more likely in dry skin than oily or well-moisturized skin, and specifically after an external skin injury such as a scratch or cut. This is believed to be caused by an infection, in which the infecting organism thrives under dry skin conditions with minimal skin oil, which otherwise protects skin from infections. The case for psoriasis is opposite to the case of athlete's foot, which occurs because of a fungus infection under wet conditions as opposed to dry in psoriasis. This infection induces inflammation, which causes the symptoms commonly associated with psoriasis, such as itching and rapid skin turnover, and leads to drier skin as the infecting organism absorbs the moisture that would otherwise go to the skin. To prevent dry skin and reduce psoriasis symptoms, it is advised to not use shower scrubs, as they not only damage skin by leaving tiny scratches, they also scrape off the naturally occurring skin oil. Additionally, moisturizers can be applied to moisturize the skin, and lotions used to promote skin oil gland functions.
Treatment

There can be substantial variation between individuals in the effectiveness of specific psoriasis treatments. Because of this, dermatologists often use a trial-and-error approach to finding the most appropriate treatment for their patient. The decision to employ a particular treatment is based on the type of psoriasis, its location, extent and severity. The patient’s age, sex, quality of life, comorbidities, and attitude toward risks associated with the treatment are also taken into consideration.
In 2008, the FDA approved three new treatment options[12] available to psoriasis patients:
1) Taclonex Scalp, a new topical ointment for treating scalp psoriasis;
2) the Xtrac Velocity excimer laser system, which emits a high-intensity beam of ultraviolet light, can treat moderate to severe psoriasis; and 3) the biologic drug adalimumab (brand name Humira) was also approved to treat moderate to severe psoriasis. Adalimumab had already been approved to treat psoriatic arthritis.
Medications with the least potential for adverse reactions are preferentially employed. If the treatment goal is not achieved then therapies with greater potential toxicity may be used. Medications with significant toxicity are reserved for severe unresponsive psoriasis. This is called the psoriasis treatment ladder.[13] As a first step, medicated ointments or creams, called topical treatments, are applied to the skin. If topical treatment fails to achieve the desired goal then the next step would be to expose the skin to ultraviolet (UV) radiation. This type of treatment is called phototherapy. The third step involves the use of medications which are taken internally by pill or injection. This approach is called systemic treatment.
Over time, psoriasis can become resistant to a specific therapy. Treatments may be periodically changed to prevent resistance developing (tachyphylaxis) and to reduce the chance of adverse reactions occurring. This is called treatment rotation.
Antibiotics are generally not indicated in routine treatment of psoriasis. However, antibiotics may be employed when an infection, such as that caused by the bacteria Streptococcus, triggers an outbreak of psoriasis, as in certain cases of guttate psoriasis.
A psychological symptom management programme has been reported as being a helpful adjunct to traditional therapies in the management of psoriasis.[14]
Topical treatment
Bath solutions and moisturizers help sooth affected skin and reduce the dryness which accompanies the build-up of skin on psoriatic plaques. Medicated creams and ointments applied directly to psoriatic plaques can help reduce inflammation, remove built-up scale, reduce skin turn over, and clear affected skin of plaques. Ointment and creams containing coal tar (no longer available on prescription in the UK), dithranol (anthralin), corticosteroids, vitamin D3 analogues (for example, calcipotriol), and retinoids are routinely used. The mechanism of action of each is probably different but they all help to normalise skin cell production and reduce inflammation. Activated vitamin D and its analogues are highly effective inhibitors of skin cell proliferation.
The disadvantages of topical agents are variably that they can often irritate normal skin, can be time consuming and awkward to apply, cannot be used for long periods, can stain clothing or have a strong odour. As a result, it is sometimes difficult for people to maintain the regular application of these medications. Abrupt withdrawal of some topical agents, particularly corticosteroids, can cause an aggressive recurrence of the condition. This is known as a rebound of the condition.
Some topical agents are used in conjunction with other therapies, especially phototherapy.
Phototherapy
It has long been recognized that daily, short, non-burning exposure to sunlight helped to clear or improve psoriasis. Niels Finsen was the first physician to investigate the therapeutic effects of sunlight scientifically and to use sunlight in clinical practice. This became known as phototherapy.
Sunlight contains many different wavelengths of light. It was during the early part of the 20th century that it was recognised that for psoriasis the therapeutic property of sunlight was due to the wavelengths classified as ultraviolet (UV) light.
Ultraviolet wavelengths are subdivided into UVA (380–315 nm) UVB (315–280 nm), and UVC (< 280 nm). Ultraviolet B (UVB) (315–280 nm) is absorbed by the epidermis and has a beneficial effect on psoriasis. Narrowband UVB (311 to 312 nm), is that part of the UVB spectrum that is most helpful for psoriasis. Exposure to UVB several times per week, over several weeks can help people attain a remission from psoriasis.
Ultraviolet light treatment is frequently combined with topical (coal tar, calcipotriol) or systemic treatment (retinoids) as there is a synergy in their combination. The Ingram regime, involves UVB and the application of anthralin paste. The Goeckerman regime combines coal tar ointment with UVB.
Photochemotherapy
Psoralen and ultraviolet A phototherapy (PUVA) combines the oral or topical administration of psoralen with exposure to ultraviolet A (UVA) light. Precisely how PUVA works is not known. The mechanism of action probably involves activation of psoralen by UVA light which inhibits the abnormally rapid production of the cells in psoriatic skin. There are multiple mechanisms of action associated with PUVA, including effects on the skin immune system.
Dark glasses must be worn during PUVA treatment because there is a risk of cataracts developing from exposure to ultraviolet A light. PUVA is associated with nausea, headache, fatigue, burning, and itching. Long-term treatment is associated with squamous-cell and melanoma skin cancers.
Systemic treatment
Psoriasis which is resistant to topical treatment and phototherapy is treated by medications that are taken internally by pill or injection. This is called systemic treatment. Patients undergoing systemic treatment are required to have regular blood and liver function tests because of the toxicity of the medication. Pregnancy must be avoided for the majority of these treatments. Most people experience a recurrence of psoriasis after systemic treatment is discontinued.
The three main traditional systemic treatments are the immunosupressant drugs methotrexate and cyclosporine, and retinoids, which are synthetic forms of vitamin A. Other additional drugs, not specifically licensed for psoriasis, have been found to be effective. These include the antimetabolite tioguanine, the cytotoxic agent hydroxyurea, sulfasalazine, the immunosupressants mycophenolate mofetil, azathioprine and oral tacrolimus. These have all been used effectively to treat psoriasis when other treatments have failed. Although not licensed in many other countries fumaric acid esters have also been used to treat severe psoriasis in Germany for over 20 years.
Biologics are manufactured proteins that interrupt the immune process involved in psoriasis. Unlike generalised immunosuppressant therapies such as methotrexate, biologics focus on specific aspects of the immune function leading to psoriasis. These drugs (interleukin antagonists) are relatively new, and their long-term impact on immune function is unknown. They are very expensive and only suitable for very few patients with psoriasis. Ustekinumab (IL-12 and IL-23 blocker) shows hopeful results for psoriasis therapy.
Alternative therapy
- Antibiotics are not indicated in routine treatment of psoriasis. However, antibiotics may be employed when an infection, such as that caused by the bacteria Streptococcus, triggers an outbreak of psoriasis, as in certain cases of guttate psoriasis.
- Climatotherapy involves the notion that some diseases can be successfully treated by living in particular climate. Several psoriasis clinics are located throughout the world based on this idea. The Dead Sea is one of the most popular locations for this type of treatment.
- In Turkey & in Croatia (Altermedica), doctor fish which live in the outdoor pools of spas, are encouraged to feed on the psoriatic skin of people with psoriasis. The fish only consume the affected areas of the skin. The outdoor location of the spa may also have a beneficial effect. This treatment can provide temporary relief of symptoms. A revisit to the spas every few months is often required. Best known is the spa “Kangal Thermal Springs”, near the Turkish village of Kavak. According to the testimony of numerous psoriasis patients, the fish lead to a significant relief. This spa is located south of the historic silk road in Anatolia. The next big city is Sivas. Treatment in this hot spring has been examined until now in two small clinical trials, with positive results.[15] [16]
- Some people subscribe to the view that psoriasis can be effectively managed through a healthy lifestyle. This view is based on anecdote, and has not been subjected to formal scientific evaluation. Nevertheless, some people report that minimizing stress and consuming a healthy diet, combined with rest, sunshine and swimming in saltwater keep lesions to a minimum. This type of "lifestyle" treatment is suggested as a long-term management strategy, rather than an initial treatment of severe psoriasis.
- A number of patients have reported significant improvements from sun and sea water: unfortunately, salt alone does not have any effect. Sea water contains so many minerals and different life forms (thousands of species of bacteria alone[17]) that it will be hard to determine which of these is causing the observed effects. Interestingly, people in the tropics differentiate between "live" and "dead" sea water: "live" sea water is water that has never been covered.
- Some psoriasis patients use herbology as a holistic approach that aims to treat the underlying causes of psoriasis. Some alternative therapies consider Oil of Oregano to be a powerful herbal method of treatment.
- A psychological symptom management programme has been reported as being a helpful adjunct to traditional therapies in the management of psoriasis.[18]
- It is claimed that Epsom salt may have a positive effect in reducing the effects of psoriasis.(The Home Remedies Handbook)
- There are claims that Neem oil has been in documented use in India for 6000 years. There are claims that this documentation is fraudulent.[19]
- It is claimed that yoga and meditative practices help psoriasis patients by 'detoxifying' the body and by the reduction of stress.
- Sulphur has been used for many years as a safe treatment in the alleviation of Psoriasis.
- Fasting is used by some to treat mild forms of psoriasis.
Historical treatment
The history of psoriasis is littered with treatments of dubious effectiveness and high toxicity. These treatments received brief popularity at particular time periods or within certain geographical regions. The application of cat faeces to red lesions on the skin, for example, was one of the earliest topical treatments employed in ancient Egypt. Onions, sea salt and urine, goose oil and semen, wasp droppings in sycamore milk, and soup made from vipers have all been reported as being ancient treatments.
In the more recent past Fowler's solution, which contains a poisonous and carcinogenic arsenic compound, was used by dermatologists as a treatment for psoriasis during the 18th and 19th centuries. Grenz Rays (also called ultrasoft X-rays or Bucky rays) was a popular treatment of psoriasis during the middle of the 20th century. This type of therapy was superseded by ultraviolet therapy.
Undecylenic acid was investigated and used for psoriasis some 40 years ago.[20]
All these treatments have fallen out of favour.
Sulphur was fashionable as a treatment for psoriasis in the Victorian and Edwardian eras. It has recently re-gained some credibilty as a safe alternative to steroids and coal tar.
Future drug development
Historically, agents used to treat psoriasis were discovered by experimentation or by accident. In contrast, current novel therapeutic agents are designed from a better understanding of the immune processes involved in psoriasis and by the specific targeting of molecular mediators. Examples can be seen in the use of biologics which target T cells and TNF inhibitors.
It has been suggested that marijuana might treat psoriasis, due to the anti-inflammatory properties of its cannabinoids, and the regulatory effects of THC on the immune system.[21] The adverse effects of marijuana might be overcome by use of more specific cannabinoid receptor medications,[22] to inhibit keratinocyte proliferation.[23]
Future innovation should see the creation of additional drugs that refine the targeting of immune-mediators further.[24]
Research into antisense oligonucleotides carries the potential to provide novel therapeutic strategies for treating psoriasis.[25]
ABT-874 is a human anti-IL-12 monoclonal antibody being developed by Abbott Laboratories in conjunction with Cambridge Antibody Technology for the treatment of multiple autoimmune diseases including psoriasis. Phase II trials have been completed and showed promising results.[26] Abbott is planning to initiate Phase III trials in 2007.[27]
Pseudoceramides
On August 27, 2006, scientists led by Jeung-Hoon Lee created in the laboratory synthetic lipids called pseudoceramides which are involved in skin cell growth and could be used in treating skin diseases such as atopic dermatitis, a form of eczema characterized by red, flaky and very itchy skin; psoriasis, a disease that causes red scaly patches on the skin; and glucocorticoid-induced epidermal atrophy, in which the skin shrinks due to skin cell loss.[28]
Prognosis
Psoriasis is a lifelong condition.[29] There is currently no cure but various treatments can help to control the symptoms. Many of the most effective agents used to treat severe psoriasis carry an increased risk of significant morbidity including skin cancers, lymphoma and liver disease. However, the majority of people's experience of psoriasis is that of minor localized patches, particularly on the elbows and knees, which can be treated with topical medication. Psoriasis does get worse over time but it is not possible to predict who will go on to develop extensive psoriasis or those in whom the disease may appear to vanish. Individuals will often experience flares and remissions throughout their lives. Controlling the signs and symptoms typically requires lifelong therapy.
According to one study,[30] psoriasis is linked to 2.5-fold increased risk for nonmelanoma skin cancer in men and women, with no preponderance of any specific histologic subtype of cancer. This, however could be linked to antipsoriatic treatment.
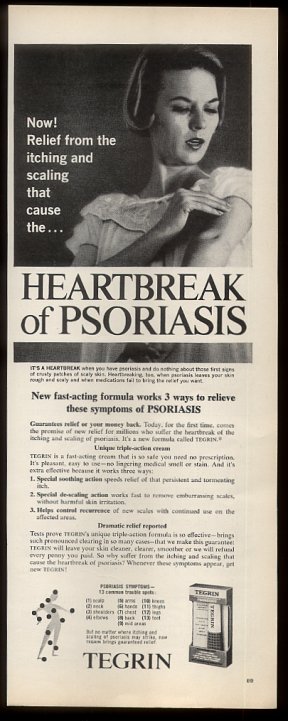
"The heartbreak of psoriasis"
The phrase "the heartbreak of psoriasis" is often used both seriously and ironically to describe the emotional impact of the disease. It may include both the effect of having a chronic uncomfortable disorder and the social effects of being self conscious of one's appearance. The term can be found in various advertisements for topical and other treatments; conversely, it has been used to mock the tendency of advertisers to exaggerate (or even fabricate) aspects of a malady for financial gain. While many products today use the phrase in their advertising, it originated in a 1960s advertising campaign for Tegrin, a coal tar-based ointment.
References
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/
- ↑ "Psoriasis Update -Skin & Aging". Retrieved 2007-07-28.
- ↑ Louden BA, Pearce DJ, Lang W, Feldman SR (2004). "A Simplified Psoriasis Area Severity Index (SPASI) for rating psoriasis severity in clinic patients". Dermatol. Online J. 10 (2): 7. PMID 15530297.
- ↑ Krueger G, Ellis CN (2005). "Psoriasis--recent advances in understanding its pathogenesis and treatment". J. Am. Acad. Dermatol. 53 (1 Suppl 1): S94–100. doi:10.1016/j.jaad.2005.04.035. PMID 15968269.
- ↑ Zenz R, Eferl R, Kenner L; et al. (2005). "Psoriasis-like skin disease and arthritis caused by inducible epidermal deletion of Jun proteins". Nature. 437 (7057): 369–75. doi:10.1038/nature03963. PMID 16163348.
- ↑ [1] Psoriasis Triggers at Psoriasis Net. SkinCarePhysicians.com 9-28-05. American Academy of Dermatology, 2008.
- ↑ Behnam SM, Behnam SE, Koo JY (2005). "Smoking and psoriasis". Skinmed. 4 (3): 174–6. PMID 15891254.
- ↑ [2][3] Fife, Jeffes, Koo, Waller. Unraveling the Paradoxes of HIV-associated Psoriasis: A Review of T-cell Subsets and Cytokine Profiles. 5-18-07. Retrieved 5-13-08.
- ↑ Ortonne JP, Lebwohl M, Em Griffiths C (2003). "Alefacept-induced decreases in circulating blood lymphocyte counts correlate with clinical response in patients with chronic plaque psoriasis". Eur J Dermatol. 13 (2): 117–23. PMID 12695125.
- ↑ Austin LM, Ozawa M, Kikuchi T, Walters IB, Krueger JG (1999). "The majority of epidermal T cells in Psoriasis vulgaris lesions can produce type 1 cytokines, interferon-gamma, interleukin-2, and tumor necrosis factor-alpha, defining TC1 (cytotoxic T lymphocyte) and TH1 effector populations: a type 1 differentiation bias is also measured in circulating blood T cells in psoriatic patients". J. Invest. Dermatol. 113 (5): 752–9. doi:10.1046/j.1523-1747.1999.00749.x. PMID 10571730. Unknown parameter
|month=ignored (help) - ↑ [4] A Case Report of Severe Psoriasis in a Patient with AIDS: The Role of the HIV Virus and the Therapeutic Challenges Involved. Vol: 13 No 2, 2002. National Skin Center. Retrieved 05-13-08.
- ↑ "Psoriasis Medical Breakthroughs" Parade.com
- ↑ Lofholm PW (2000). "The psoriasis treatment ladder: a clinical overview for pharmacists". US Pharm. 25 (5): 26–47.
- ↑ "Research Findings Register: summary number 637". Retrieved 2007-07-22.
- ↑ Ozcelik S, Polat HH, Akyol M, Yalcin AN, Ozcelik D, Marufihah M. Kangal hot spring with fish and psoriasis treatment. J Dermatol. 2000 Jun;27(6):386-90.
- ↑ Grassberger M, Hoch W. Ichthyotherapy as alternative treatment for patients with psoriasis: a pilot study. Evid Based Complement Alternat Med. 2006 Dec;3(4):483-8.
- ↑ "News in Science - Oceans a complex, diverse bug soup - 01/08/2006". Retrieved 2007-07-22.
- ↑ "Research Findings Register: summary number 637". Retrieved 2007-07-22.
- ↑ "Psoriasis Hall of PShame". Retrieved 2007-07-22.
- ↑ Ereaux L, Craig G (1949). "The Oral Administration Of Undecylenic Acid In The Treatment Of Psoriasis" (PDF). Canad. M. A. J. 61: 361–4. Retrieved 2007-01-05. Unknown parameter
|month=ignored (help) - see page 4/364 of link - ↑ Namazi MR (2005). "Cannabinoids, loratadine and allopurinol as novel additions to the antipsoriatic ammunition". Journal of the European Academy of Dermatology and Venereology : JEADV. 19 (3): 319–22. doi:10.1111/j.1468-3083.2004.01184.x. PMID 15857457.
- ↑ Fowler CJ (2005). "Pharmacological properties and therapeutic possibilities for drugs acting upon endocannabinoid receptors". Current drug targets. CNS and neurological disorders. 4 (6): 685–96. PMID 16375686.
- ↑ Wilkinson JD, Williamson EM (2007). "Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis". J. Dermatol. Sci. 45 (2): 87–92. doi:10.1016/j.jdermsci.2006.10.009. PMID 17157480.
- ↑ Nickoloff BJ, Nestle FO (2004). "Recent insights into the immunopathogenesis of psoriasis provide new therapeutic opportunities". J. Clin. Invest. 113 (12): 1664–75. doi:10.1172/JCI200422147. PMID 15199399.
- ↑ White PJ, Atley LM, Wraight CJ (2004). "Antisense oligonucleotide treatments for psoriasis". Expert opinion on biological therapy. 4 (1): 75–81. doi:10.1517/14712598.4.1.75. PMID 14680470.
- ↑ Heller M. (2007) Positive results for ABT-874 in the treatment of psoriasis J Drugs Dermatol
- ↑ http://www.cambridgeantibody.com/home/products/licensed_products/abbott/abt874
- ↑ Science Daily, New Skin-healing Chemicals
- ↑ Jobling R (2007). "A patient's journey:Psoriasis". Br Med J. 334: 953&ndash, 4. doi:10.1136/bmj.39184.615150.802.
- ↑ Olsen JH, Frentz G, Møller H (1993). "[Psoriasis and cancer]". Ugeskr. Laeg. (in Danish). 155 (35): 2687–91. PMID 8212383.
Some of the information on this page was taken from the following public-domain resource: "Questions and Answers about Psoriasis", National Institute of Arthritis and Musculoskeletal and Skin Diseases