Bowel obstruction pathophysiology: Difference between revisions
m (Categories) |
|||
| (24 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Bowel obstruction}} | {{Bowel obstruction}} | ||
{{CMG}} | {{CMG}};{{AE}}{{HM}} | ||
==Overview== | ==Overview== | ||
It is thought that bowel obstruction may occur functionally as a result of abnormal [[anatomy]] or impairment of the [[autonomic nervous system]] or mechanically, which may occur [[Acute (medicine)|acutely]] or [[Chronic (medical)|chronically]]. An obstruction that occurs functionally or mechanically can be classified as extrinsic, intrinsic or intraluminal including [[Tumor|tumors]], [[Stenosis|strictures]] and [[foreign bodies]]. Excessive [[Bloating|bowel distention]] can lead to [[ischemia]], [[necrosis]] and [[perforation]]. A functional obstruction may be due to a number of [[genetic defects]] including [[Down syndrome|trisomy 21]] and the [[RET proto-oncogene]] mutation. Associated conditions include post-operative [[Adhesion (medicine)|adhesions]], complicated [[Hernia|hernias]], gastrointestinal cancers and [[endometriosis]]. Gross pathology may demonstrate [[Adhesion (medicine)|adhesions]], narrow [[Lumen (anatomy)|lumens]] and [[volvulus]]. Microscopic pathology may show evidence of [[fibrosis]], [[necrosis]] and [[ischemia]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis of true bowel obstructions=== | |||
*Normally, the [[small intestine]] functions to pass [[Gastrointestinal tract|gastrointestinal]] contents for [[absorption]]. The large surface area provided by the [[Intestinal villus|villi]], [[Circular folds|plicae circularis]] and valvulae conniventes (Kerckring folds) allow for this exchange to happens.<ref name="pmid5540839">{{cite journal |vauthors=Wright HK, O'Brien JJ, Tilson MD |title=Water absorption in experimental closed segment obstruction of the ileum in man |journal=Am. J. Surg. |volume=121 |issue=1 |pages=96–9 |year=1971 |pmid=5540839 |doi= |url=}}</ref><ref name="pmid17859455">{{cite journal |vauthors=Noer RJ, Derr JW, Johnston CG |title=The Circulation of the Small Intestine: An Evaluation of its Revascularizing Potential |journal=Ann. Surg. |volume=130 |issue=4 |pages=608–21 |year=1949 |pmid=17859455 |pmc=1616446 |doi= |url=}}</ref><ref name="pmid17230614">{{cite journal |vauthors=Markogiannakis H, Messaris E, Dardamanis D, Pararas N, Tzertzemelis D, Giannopoulos P, Larentzakis A, Lagoudianakis E, Manouras A, Bramis I |title=Acute mechanical bowel obstruction: clinical presentation, etiology, management and outcome |journal=World J. Gastroenterol. |volume=13 |issue=3 |pages=432–7 |year=2007 |pmid=17230614 |pmc=4065900 |doi= |url=}}</ref> | |||
*In addition, the [[small bowel]] is free of [[microbes]], in comparison to the [[large bowel]] that houses commensal [[flora]] that facilitate [[digestion]] and [[vitamin]] synthesis, namely [[vitamin K]]. | |||
*Continuous transit throughout the bowel is important to prevent bowel [[Dilation|dilatation]], [[ischemia]] and [[necrosis]]. | |||
*Obstruction of the bowel can occur functionally (due to abnormal anatomy) or mechanically, which can be [[Acute (medicine)|acute]] or [[chronic]]. | |||
*Obstructions that occur functionally or mechanically, can be classified as extrinsic, intrinsic or intraluminal obstruction: | |||
**Extrinsic obstructions can happen as the result of a [[tumor]], post-operative [[Adhesion (medicine)|adhesions]] or [[Hernia|hernias]]. | |||
**Intrinsic obstructions can happen as a result of a [[tumor]], [[stenosis]] or [[hematoma]]. | |||
**Intraluminal obstructions are sometimes referred to intramural obstructions and include, [[foreign bodies]], [[intussusception]] and [[Gallstone disease|gallstones]]. | |||
*However an obstruction occurs, [[proximal]] to the blockage there will be a dilated segment, whilst [[distal]] to the obstruction the segment of bowel will collapse as the contents cannot pass. | |||
*[[Bloating|Bowel distention]] occurs as air that is swallowed and gases produced by the commensal [[flora]] begins to accumulate. | |||
*Eventually, the bowel wall becomes [[Edema|edematous]] and fluid gathers inside the lumen of the bowel. This disrupts the absorptive properties of the gut. | |||
*Some fluid may be lost to the [[peritoneal cavity]], moreover, the proximal obstruction can cause severe [[emesis]] which will lead to further loss of fluid that contains vital [[Electrolyte|electrolytes]]. This process may result in [[metabolic alkalosis]] and [[hypovolemia]]. | |||
*The obstruction also causes the normally sterile proximal bowel to become overgrown with [[bacteria]] and vomitus may contain feces. | |||
*When a massive dilation of the bowel occurs, the vessels that perfuse the walls of the bowel become compressed and will not be able to supply the bowel loop adequately, which leads to [[ischemia]]. | |||
*If [[ischemia]] is not reversed within a timely manner, then [[necrosis]], [[volvulus]] and [[perforation]] may ensue. | |||
=== | ===Pathogenesis of bowel pseudo-obstructions=== | ||
====Ogilvie's syndrome==== | |||
*The association of [[Spinal anaesthesia|spinal anaesthesias]], drugs and nervous trauma has lead to the understanding that [[Ogilvie syndrome]] (colonic dilatation without true obstruction) may be caused by impairment of the [[autonomic nervous system]].<ref name="pmid3753674">{{cite journal |vauthors=Vanek VW, Al-Salti M |title=Acute pseudo-obstruction of the colon (Ogilvie's syndrome). An analysis of 400 cases |journal=Dis. Colon Rectum |volume=29 |issue=3 |pages=203–10 |year=1986 |pmid=3753674 |doi= |url=}}</ref><ref name="pmid3319452">{{cite journal |vauthors=Ogilvie WH |title=William Heneage Ogilvie 1887-1971. Large-intestine colic due to sympathetic deprivation. A new clinical syndrome |journal=Dis. Colon Rectum |volume=30 |issue=12 |pages=984–7 |year=1987 |pmid=3319452 |doi= |url=}}</ref><ref name="pmid17643908">{{cite journal |vauthors=Saunders MD |title=Acute colonic pseudo-obstruction |journal=Best Pract Res Clin Gastroenterol |volume=21 |issue=4 |pages=671–87 |year=2007 |pmid=17643908 |doi=10.1016/j.bpg.2007.03.001 |url=}}</ref> | |||
*Damage to the [[Parasympathetic nervous system|parasympathetic]] fibers of S2 - S4 causes the distal colon to become atonic and become obstructed proximally. | |||
*However, the exact mechanism is unknown, especially in patients who present with this syndrome without an obvious injury to the [[Parasympathetic nervous system|parasympathetic nerves]]. | |||
*Acute colonic [[Pseudo-obstruction-intestinal|pseudo-obstruction]] occurs when the colon's diameter rises quickly, which increases the tension in the colonic wall, leading to colonic [[ischemia]] and possibly, [[perforation]] with a diameter exceeding 10 - 12cm. | |||
*A rare case of [[Ogilvie syndrome]] showed atrophic [[myopathy]] with a thinned out colonic wall, despite a perfectly intact [[myenteric plexus]] and unaffected [[Ganglion cell|ganglion cells]], with no evidence of [[fibrosis]] or [[inflammation]]. | |||
[ | ====Paralytic ileus==== | ||
*The majority of [[Ileus|paralytic (adynamic) ileus]] cases occur after major [[abdominal surgery]], such as [[hysterectomy]]. | |||
*[[Paralytic ileus]] is thought to occur with manipulation and trauma of the intestinal tract. | |||
*Post operative dysmotility is associated with [[inflammation]], impaired neural reflexes and the release of neural hormone peptides. | |||
**[[Inflammation]]:<ref name="pmid14699497">{{cite journal |vauthors=Schwarz NT, Kalff JC, Türler A, Speidel N, Grandis JR, Billiar TR, Bauer AJ |title=Selective jejunal manipulation causes postoperative pan-enteric inflammation and dysmotility |journal=Gastroenterology |volume=126 |issue=1 |pages=159–69 |year=2004 |pmid=14699497 |doi= |url=}}</ref> | |||
***Intestinal manipulation leads to intestinal [[ischemia]], and shifting of endogenous cellular danger molecules and [[Cytokine|cytokines]] away from the site of trauma. | |||
***[[White blood cells|Leukocytic]] infiltration, [[macrophage]] and [[mast cell]] stimulation commences and causes muscular dysfunction, and therefore [[inflammation]] in the manipulated segment. | |||
**Neural reflexes:<ref name="pmid14699497">{{cite journal |vauthors=Schwarz NT, Kalff JC, Türler A, Speidel N, Grandis JR, Billiar TR, Bauer AJ |title=Selective jejunal manipulation causes postoperative pan-enteric inflammation and dysmotility |journal=Gastroenterology |volume=126 |issue=1 |pages=159–69 |year=2004 |pmid=14699497 |doi= |url=}}</ref> | |||
***Inhibitory [[Sympathetic control|sympathetic]] neural reflexes increase due to noxious spinal afferent signals, therefore, the use of [[epidural]] local [[anesthetics]] or topical [[capsaicin]] is encouraged to prevent [[paralytic ileus]].<ref name="pmid11034732">{{cite journal |vauthors=Jørgensen H, Wetterslev J, Møiniche S, Dahl JB |title=Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery |journal=Cochrane Database Syst Rev |volume= |issue=4 |pages=CD001893 |year=2000 |pmid=11034732 |doi=10.1002/14651858.CD001893 |url=}}</ref> | |||
**Neurohormonal peptides:<ref name="pmid10648460">{{cite journal |vauthors=Kalff JC, Schraut WH, Billiar TR, Simmons RL, Bauer AJ |title=Role of inducible nitric oxide synthase in postoperative intestinal smooth muscle dysfunction in rodents |journal=Gastroenterology |volume=118 |issue=2 |pages=316–27 |year=2000 |pmid=10648460 |doi= |url=}}</ref><ref name="pmid7515341">{{cite journal |vauthors=Cullen JJ, Eagon JC, Kelly KA |title=Gastrointestinal peptide hormones during postoperative ileus. Effect of octreotide |journal=Dig. Dis. Sci. |volume=39 |issue=6 |pages=1179–84 |year=1994 |pmid=7515341 |doi= |url=}}</ref> | |||
***Inhibitory [[Neurotransmitter|neurotransmitters]] are released and cause the gut motility to slow down. | |||
***Inhibitory [[Neurotransmitter|neurotransmitters]] include, [[nitric oxide]], [[Vasoactive intestinal peptide|vasoactive intestinal polypeptide]], and [[substance P]]. | |||
< | ==Genetics== | ||
< | The development of [[Congenital disorder|congenital]] bowel obstruction is the result of multiple [[genetic mutations]]:<ref name="pmid27896149">{{cite journal |vauthors=Mitul AR |title=Congenital Neonatal Intestinal Obstruction |journal=J Neonatal Surg |volume=5 |issue=4 |pages=41 |year=2016 |pmid=27896149 |pmc=5117264 |doi=10.21699/jns.v5i4.472 |url=}}</ref><ref name="pmid16802577">{{cite journal |vauthors=Huis M, Stulhofer M, Szerda F, Vukić T, Bubnjar J |title=[Obstruction icterus--our experience] |journal=Acta Med Croatica |volume=60 |issue=1 |pages=71–6 |year=2006 |pmid=16802577 |doi= |url=}}</ref><ref name="pmid14896034">{{cite journal |vauthors=BODIAN M, WHITE LL, CARTER CO, LOUW JH |title=Congenital duodenal obstruction and mongolism |journal=Br Med J |volume=1 |issue=4749 |pages=77–9 |year=1952 |pmid=14896034 |pmc=2022519 |doi= |url=}}</ref><ref name="pmid9605910">{{cite journal |vauthors=Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA |title=Intestinal atresia and stenosis: a 25-year experience with 277 cases |journal=Arch Surg |volume=133 |issue=5 |pages=490–6; discussion 496–7 |year=1998 |pmid=9605910 |doi= |url=}}</ref> | ||
*[[Down syndrome|Chromosome 21 trisomy]] can lead to [[imperforate anus]] and [[Duodenal atresia|duodenal atresias]] in 50% of babies with [[down syndrome]]. | |||
*[[Cystic fibrosis transmembrane conductance regulator|Chromosome 7]] mutation locus leads to [[cystic fibrosis]] that predisposes to a thickened [[Meconium ileus|meconium]] which may lead to an intraluminal obstruction of the [[terminal ileum]] and microcolon. | |||
</ | *[[Hirschsprung's disease]] is associated with several gene mutations: | ||
</ | **The [[RET proto-oncogene]] located on chromosome 10q11.21 that interacts with the EDNRB protein located on chromosome 13. | ||
**Mutations in the [[RET gene|RET]] and 3p21, 9q31, and 19q12 genes leads to failure of migration of the enteric [[Neural crest|neural crest cells]]. | |||
**[[Hirschsprung|Hirschsprung syndrome]] is associated with PHOX2B [[homeobox gene]] [[mutation]]<nowiki/>s. | |||
**The following protein mutations may also lead to [[Hirschsprung's disease]]: | |||
***Chromosome 5 - GDNF protein | |||
*** Chromosome 20 - EDN3 protein | |||
***Chromosome 22 - SOX10 protein | |||
*** Chromosom 1 - ECE1 protein | |||
*** Chromosome 19 - NTN protein | |||
***Chromosome 2 - SIP1 protein | |||
==Associated Conditions== | |||
*Conditions associated with extrinsic bowel obstruction include:<ref name="pmid10971435">{{cite journal |vauthors=Miller G, Boman J, Shrier I, Gordon PH |title=Natural history of patients with adhesive small bowel obstruction |journal=Br J Surg |volume=87 |issue=9 |pages=1240–7 |year=2000 |pmid=10971435 |doi=10.1046/j.1365-2168.2000.01530.x |url=}}</ref><ref name="pmid7573729">{{cite journal |vauthors=Barkan H, Webster S, Ozeran S |title=Factors predicting the recurrence of adhesive small-bowel obstruction |journal=Am. J. Surg. |volume=170 |issue=4 |pages=361–5 |year=1995 |pmid=7573729 |doi= |url=}}</ref><ref name="pmid19756860">{{cite journal |vauthors=Butt MU, Velmahos GC, Zacharias N, Alam HB, de Moya M, King DR |title=Adhesional small bowel obstruction in the absence of previous operations: management and outcomes |journal=World J Surg |volume=33 |issue=11 |pages=2368–71 |year=2009 |pmid=19756860 |doi=10.1007/s00268-009-0200-6 |url=}}</ref><ref name="pmid24565365">{{cite journal |vauthors=Beardsley C, Furtado R, Mosse C, Gananadha S, Fergusson J, Jeans P, Beenen E |title=Small bowel obstruction in the virgin abdomen: the need for a mandatory laparotomy explored |journal=Am. J. Surg. |volume=208 |issue=2 |pages=243–8 |year=2014 |pmid=24565365 |doi=10.1016/j.amjsurg.2013.09.034 |url=}}</ref> | |||
**[[Adhesions]] | |||
**[[Hernia]] | |||
**[[Volvulus]] | |||
**[[Endometriosis]] | |||
*Conditions associated with intrinsic bowel obstruction include:<ref name="pmid10971435" /><ref name="pmid7573729" /><ref name="pmid19756860" /><ref name="pmid24565365" /> | |||
**Large and small bowel cancers | |||
**[[Cystic fibrosis]] | |||
**[[Hirschsprung's disease]] | |||
**[[Down syndrome]] | |||
**[[Stenosis|Strictures]]: | |||
***[[Anatomical]] | |||
***[[Inflammatory]] | |||
***[[Ischemic]] | |||
***[[Radiation]] | |||
*Conditions associated with intraluminal bowel obstruction include:<ref name="pmid10971435" /><ref name="pmid7573729" /><ref name="pmid19756860" /><ref name="pmid24565365" /> | |||
**Gastrointestinal [[foreign body]] | |||
**[[Intussusception]] | |||
**[[Gallstone disease|Gallstones]] | |||
**[[Constipation]] | |||
**[[Bezoar]] | |||
**[[Volvulus]] | |||
**[[Hematoma]] | |||
==Gross Pathology== | |||
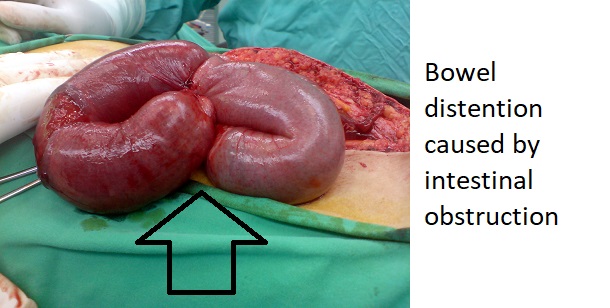
*On gross pathology, [[Adhesion (medicine)|adhesions]], [[volvulus]], narrow lumen with proximal dilatations and [[exudate]] are characteristic findings of bowel obstruction.<ref name="pmid24565365">{{cite journal |vauthors=Beardsley C, Furtado R, Mosse C, Gananadha S, Fergusson J, Jeans P, Beenen E |title=Small bowel obstruction in the virgin abdomen: the need for a mandatory laparotomy explored |journal=Am. J. Surg. |volume=208 |issue=2 |pages=243–8 |year=2014 |pmid=24565365 |doi=10.1016/j.amjsurg.2013.09.034 |url=}}</ref> | |||
[[Image:bob.jpg|thumb|center|500px|Image shows a distended bowel after intestinal obstruction. By haitham alfalah - haitham alfalah, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=7313100]] | |||
==Microscopic Pathology== | |||
*On microscopic histopathological analysis, [[fibrosis]], [[necrosis]], and [[ischemia]] are characteristic findings of bowel obstruction.<ref name="pmid24565365">{{cite journal |vauthors=Beardsley C, Furtado R, Mosse C, Gananadha S, Fergusson J, Jeans P, Beenen E |title=Small bowel obstruction in the virgin abdomen: the need for a mandatory laparotomy explored |journal=Am. J. Surg. |volume=208 |issue=2 |pages=243–8 |year=2014 |pmid=24565365 |doi=10.1016/j.amjsurg.2013.09.034 |url=}}</ref> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Up-To-Date]] | |||
| |||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 16:47, 26 February 2018
|
Bowel obstruction Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Bowel obstruction pathophysiology On the Web |
|
American Roentgen Ray Society Images of Bowel obstruction pathophysiology |
|
Risk calculators and risk factors for Bowel obstruction pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Hadeel Maksoud M.D.[2]
Overview
It is thought that bowel obstruction may occur functionally as a result of abnormal anatomy or impairment of the autonomic nervous system or mechanically, which may occur acutely or chronically. An obstruction that occurs functionally or mechanically can be classified as extrinsic, intrinsic or intraluminal including tumors, strictures and foreign bodies. Excessive bowel distention can lead to ischemia, necrosis and perforation. A functional obstruction may be due to a number of genetic defects including trisomy 21 and the RET proto-oncogene mutation. Associated conditions include post-operative adhesions, complicated hernias, gastrointestinal cancers and endometriosis. Gross pathology may demonstrate adhesions, narrow lumens and volvulus. Microscopic pathology may show evidence of fibrosis, necrosis and ischemia.
Pathophysiology
Pathogenesis of true bowel obstructions
- Normally, the small intestine functions to pass gastrointestinal contents for absorption. The large surface area provided by the villi, plicae circularis and valvulae conniventes (Kerckring folds) allow for this exchange to happens.[1][2][3]
- In addition, the small bowel is free of microbes, in comparison to the large bowel that houses commensal flora that facilitate digestion and vitamin synthesis, namely vitamin K.
- Continuous transit throughout the bowel is important to prevent bowel dilatation, ischemia and necrosis.
- Obstruction of the bowel can occur functionally (due to abnormal anatomy) or mechanically, which can be acute or chronic.
- Obstructions that occur functionally or mechanically, can be classified as extrinsic, intrinsic or intraluminal obstruction:
- Extrinsic obstructions can happen as the result of a tumor, post-operative adhesions or hernias.
- Intrinsic obstructions can happen as a result of a tumor, stenosis or hematoma.
- Intraluminal obstructions are sometimes referred to intramural obstructions and include, foreign bodies, intussusception and gallstones.
- However an obstruction occurs, proximal to the blockage there will be a dilated segment, whilst distal to the obstruction the segment of bowel will collapse as the contents cannot pass.
- Bowel distention occurs as air that is swallowed and gases produced by the commensal flora begins to accumulate.
- Eventually, the bowel wall becomes edematous and fluid gathers inside the lumen of the bowel. This disrupts the absorptive properties of the gut.
- Some fluid may be lost to the peritoneal cavity, moreover, the proximal obstruction can cause severe emesis which will lead to further loss of fluid that contains vital electrolytes. This process may result in metabolic alkalosis and hypovolemia.
- The obstruction also causes the normally sterile proximal bowel to become overgrown with bacteria and vomitus may contain feces.
- When a massive dilation of the bowel occurs, the vessels that perfuse the walls of the bowel become compressed and will not be able to supply the bowel loop adequately, which leads to ischemia.
- If ischemia is not reversed within a timely manner, then necrosis, volvulus and perforation may ensue.
Pathogenesis of bowel pseudo-obstructions
Ogilvie's syndrome
- The association of spinal anaesthesias, drugs and nervous trauma has lead to the understanding that Ogilvie syndrome (colonic dilatation without true obstruction) may be caused by impairment of the autonomic nervous system.[4][5][6]
- Damage to the parasympathetic fibers of S2 - S4 causes the distal colon to become atonic and become obstructed proximally.
- However, the exact mechanism is unknown, especially in patients who present with this syndrome without an obvious injury to the parasympathetic nerves.
- Acute colonic pseudo-obstruction occurs when the colon's diameter rises quickly, which increases the tension in the colonic wall, leading to colonic ischemia and possibly, perforation with a diameter exceeding 10 - 12cm.
- A rare case of Ogilvie syndrome showed atrophic myopathy with a thinned out colonic wall, despite a perfectly intact myenteric plexus and unaffected ganglion cells, with no evidence of fibrosis or inflammation.
Paralytic ileus
- The majority of paralytic (adynamic) ileus cases occur after major abdominal surgery, such as hysterectomy.
- Paralytic ileus is thought to occur with manipulation and trauma of the intestinal tract.
- Post operative dysmotility is associated with inflammation, impaired neural reflexes and the release of neural hormone peptides.
- Inflammation:[7]
- Intestinal manipulation leads to intestinal ischemia, and shifting of endogenous cellular danger molecules and cytokines away from the site of trauma.
- Leukocytic infiltration, macrophage and mast cell stimulation commences and causes muscular dysfunction, and therefore inflammation in the manipulated segment.
- Neural reflexes:[7]
- Inhibitory sympathetic neural reflexes increase due to noxious spinal afferent signals, therefore, the use of epidural local anesthetics or topical capsaicin is encouraged to prevent paralytic ileus.[8]
- Neurohormonal peptides:[9][10]
- Inhibitory neurotransmitters are released and cause the gut motility to slow down.
- Inhibitory neurotransmitters include, nitric oxide, vasoactive intestinal polypeptide, and substance P.
- Inflammation:[7]
Genetics
The development of congenital bowel obstruction is the result of multiple genetic mutations:[11][12][13][14]
- Chromosome 21 trisomy can lead to imperforate anus and duodenal atresias in 50% of babies with down syndrome.
- Chromosome 7 mutation locus leads to cystic fibrosis that predisposes to a thickened meconium which may lead to an intraluminal obstruction of the terminal ileum and microcolon.
- Hirschsprung's disease is associated with several gene mutations:
- The RET proto-oncogene located on chromosome 10q11.21 that interacts with the EDNRB protein located on chromosome 13.
- Mutations in the RET and 3p21, 9q31, and 19q12 genes leads to failure of migration of the enteric neural crest cells.
- Hirschsprung syndrome is associated with PHOX2B homeobox gene mutations.
- The following protein mutations may also lead to Hirschsprung's disease:
- Chromosome 5 - GDNF protein
- Chromosome 20 - EDN3 protein
- Chromosome 22 - SOX10 protein
- Chromosom 1 - ECE1 protein
- Chromosome 19 - NTN protein
- Chromosome 2 - SIP1 protein
Associated Conditions
- Conditions associated with extrinsic bowel obstruction include:[15][16][17][18]
- Conditions associated with intrinsic bowel obstruction include:[15][16][17][18]
- Large and small bowel cancers
- Cystic fibrosis
- Hirschsprung's disease
- Down syndrome
- Strictures:
- Conditions associated with intraluminal bowel obstruction include:[15][16][17][18]
- Gastrointestinal foreign body
- Intussusception
- Gallstones
- Constipation
- Bezoar
- Volvulus
- Hematoma
Gross Pathology
- On gross pathology, adhesions, volvulus, narrow lumen with proximal dilatations and exudate are characteristic findings of bowel obstruction.[18]
Microscopic Pathology
- On microscopic histopathological analysis, fibrosis, necrosis, and ischemia are characteristic findings of bowel obstruction.[18]
References
- ↑ Wright HK, O'Brien JJ, Tilson MD (1971). "Water absorption in experimental closed segment obstruction of the ileum in man". Am. J. Surg. 121 (1): 96–9. PMID 5540839.
- ↑ Noer RJ, Derr JW, Johnston CG (1949). "The Circulation of the Small Intestine: An Evaluation of its Revascularizing Potential". Ann. Surg. 130 (4): 608–21. PMC 1616446. PMID 17859455.
- ↑ Markogiannakis H, Messaris E, Dardamanis D, Pararas N, Tzertzemelis D, Giannopoulos P, Larentzakis A, Lagoudianakis E, Manouras A, Bramis I (2007). "Acute mechanical bowel obstruction: clinical presentation, etiology, management and outcome". World J. Gastroenterol. 13 (3): 432–7. PMC 4065900. PMID 17230614.
- ↑ Vanek VW, Al-Salti M (1986). "Acute pseudo-obstruction of the colon (Ogilvie's syndrome). An analysis of 400 cases". Dis. Colon Rectum. 29 (3): 203–10. PMID 3753674.
- ↑ Ogilvie WH (1987). "William Heneage Ogilvie 1887-1971. Large-intestine colic due to sympathetic deprivation. A new clinical syndrome". Dis. Colon Rectum. 30 (12): 984–7. PMID 3319452.
- ↑ Saunders MD (2007). "Acute colonic pseudo-obstruction". Best Pract Res Clin Gastroenterol. 21 (4): 671–87. doi:10.1016/j.bpg.2007.03.001. PMID 17643908.
- ↑ 7.0 7.1 Schwarz NT, Kalff JC, Türler A, Speidel N, Grandis JR, Billiar TR, Bauer AJ (2004). "Selective jejunal manipulation causes postoperative pan-enteric inflammation and dysmotility". Gastroenterology. 126 (1): 159–69. PMID 14699497.
- ↑ Jørgensen H, Wetterslev J, Møiniche S, Dahl JB (2000). "Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery". Cochrane Database Syst Rev (4): CD001893. doi:10.1002/14651858.CD001893. PMID 11034732.
- ↑ Kalff JC, Schraut WH, Billiar TR, Simmons RL, Bauer AJ (2000). "Role of inducible nitric oxide synthase in postoperative intestinal smooth muscle dysfunction in rodents". Gastroenterology. 118 (2): 316–27. PMID 10648460.
- ↑ Cullen JJ, Eagon JC, Kelly KA (1994). "Gastrointestinal peptide hormones during postoperative ileus. Effect of octreotide". Dig. Dis. Sci. 39 (6): 1179–84. PMID 7515341.
- ↑ Mitul AR (2016). "Congenital Neonatal Intestinal Obstruction". J Neonatal Surg. 5 (4): 41. doi:10.21699/jns.v5i4.472. PMC 5117264. PMID 27896149.
- ↑ Huis M, Stulhofer M, Szerda F, Vukić T, Bubnjar J (2006). "[Obstruction icterus--our experience]". Acta Med Croatica. 60 (1): 71–6. PMID 16802577.
- ↑ BODIAN M, WHITE LL, CARTER CO, LOUW JH (1952). "Congenital duodenal obstruction and mongolism". Br Med J. 1 (4749): 77–9. PMC 2022519. PMID 14896034.
- ↑ Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA (1998). "Intestinal atresia and stenosis: a 25-year experience with 277 cases". Arch Surg. 133 (5): 490–6, discussion 496–7. PMID 9605910.
- ↑ 15.0 15.1 15.2 Miller G, Boman J, Shrier I, Gordon PH (2000). "Natural history of patients with adhesive small bowel obstruction". Br J Surg. 87 (9): 1240–7. doi:10.1046/j.1365-2168.2000.01530.x. PMID 10971435.
- ↑ 16.0 16.1 16.2 Barkan H, Webster S, Ozeran S (1995). "Factors predicting the recurrence of adhesive small-bowel obstruction". Am. J. Surg. 170 (4): 361–5. PMID 7573729.
- ↑ 17.0 17.1 17.2 Butt MU, Velmahos GC, Zacharias N, Alam HB, de Moya M, King DR (2009). "Adhesional small bowel obstruction in the absence of previous operations: management and outcomes". World J Surg. 33 (11): 2368–71. doi:10.1007/s00268-009-0200-6. PMID 19756860.
- ↑ 18.0 18.1 18.2 18.3 18.4 Beardsley C, Furtado R, Mosse C, Gananadha S, Fergusson J, Jeans P, Beenen E (2014). "Small bowel obstruction in the virgin abdomen: the need for a mandatory laparotomy explored". Am. J. Surg. 208 (2): 243–8. doi:10.1016/j.amjsurg.2013.09.034. PMID 24565365.