STEMI resident survival guide: Difference between revisions
Rim Halaby (talk | contribs) |
No edit summary |
||
| (147 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="width: 80%;"> | |||
__NOTOC__ | __NOTOC__ | ||
{{STEMI resident survival guide}} | |||
{{CMG}}; {{AE}} {{AL}}; {{Rim}} | {{CMG}}; {{AE}} {{AL}}; {{Rim}} | ||
==Overview== | ==Overview== | ||
[[ST elevation myocardial infarction]] ([[STEMI]]) is a syndrome characterized by the presence of symptoms of [[myocardial ischemia]] associated with persistent [[ST elevation]] on [[ | [[ST elevation myocardial infarction]] ([[STEMI]]) is a syndrome characterized by the presence of symptoms of [[myocardial ischemia]] associated with persistent [[ST elevation]] on [[electrocardiogram]] and elevated [[cardiac enzymes]]. The management of [[STEMI]] should be initiated without delay and the following timelines should be minimized (the 4 D's): | ||
===Door to Data=== | |||
If a patient presents with [[chest discomfort]], an [[electrocardiogram]] must be obtained immediately and no later than 5-10 minutes after arrival. In the patient with [[chest discomfort]], an [[electrocardiogram]] should be obtained prior to obtaining insurance / payment information. | |||
===Data to Decision=== | |||
If the [[electrocardiogram]] shows [[ST segment elevation]], [[ST segment depression]] consistent with [[posterior MI]], or a new [[left bundle branch block]], a decision must be made within 5 to 10 minutes as to whether to administer a [[fibrinolytic agent]] or to proceed to [[primary angioplasty]]. | |||
===Decision to Drug or Device=== | |||
Once a decision is made to administer a [[fibrinolytic agent]] or to proceed to [[primary angioplasty]] this should be carried out within 30 minutes. | |||
==Causes== | ==Causes== | ||
===Life Threatening Causes=== | ===Life Threatening Causes=== | ||
[[STEMI]] is a life-threatening condition and must be treated as such irrespective of the underlying cause. | |||
===Common Causes=== | ===Common Causes=== | ||
* [[Plaque rupture]] | |||
* [[Takotsubo cardiomyopathy]] (also known as [[broken heart syndrome]] or [[stress cardiomyopathy]]) | |||
* [[Aortic dissection]] with propagation to the [[right coronary artery]] | * [[Aortic dissection]] with propagation to the [[right coronary artery]] | ||
* [[Cocaine]] | * [[Cocaine]] | ||
== | ==Pre-Hospital Care== | ||
Pre-hospital care can begin in the ambulance by [[Emergency Medical Services]] (EMS) personnel and it can decrease the delay in the management of [[STEMI]] patients. In the United States, volunteers and fire fighters are permitted to initiate emergency care prior to the arrival of highly trained [[paramedics]] by beginning [[CPR]] and if adequately trained, can defibrillate the patient using an [[Defibrillation|automatic external defibrillator]]. Early access to [[EMS]] is promoted by a 9-1-1 system. | |||
{{Family tree/start}} | |||
{{familytree | A01 | | |A01= <div style="float: left; text-align: left; width: 30em; padding:1em;"> '''Prehospital Care'''<br> | |||
❑ Check the [[vital signs]] <br> | |||
❑ Perform [[ECG|12 lead ECG]] and transmit it to the receiving hospital<br> | |||
❑ Establish large bore [[Intravenous therapy|IV access]]<br> | |||
❑ Administer [[oxygen]]<br> | |||
❑ Administer medications (depending on the level of training) | |||
:❑ [[Aspirin|Non-enteric coated aspirin]] | |||
:❑ [[Nitroglycerin|Sublingual nitroglycerin]] if an [[RV infarct]] and / or [[hypotension]] are not present | |||
:❑ In so far as the risk of emergency [[CABG|coronary artery bypass surgery]] is <u><</u>1%, a [[thienopyridine]] such as [[Prasugrel]], [[Ticagrelor]] or [[Clopidogrel]] can be administered | |||
:❑ [[Unfractionated heparin]] | |||
:❑ [[Glycoprotein IIb IIIa inhibitors]] | |||
:❑ [[Fibrinolytic therapy]] (especially in rural areas) | |||
❑ Activate the cardiac cath team in the hospital<br> | |||
❑ [[Resuscitation]] in case of [[cardiac arrest]]<br> | |||
:❑ [[CPR]] | |||
:❑ [[Defibrillation|Automated defibrillator]]</div> }} | |||
{{Family tree/end}} | |||
< | ==FIRE: Focused Initial Rapid Evaluation== | ||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | |||
<span style="font-size:85%"> '''Abbreviations:''' | |||
'''LBBB:''' [[left bundle branch block]]; '''CABG:''' [[coronary artery bypass graft]]; '''COPD:''' [[chronic obstructive pulmonary disease]]; '''DVT:''' [[deep vein thrombosis]]; '''ECG:''' [[electrocardiography]]; '''GP IIb IIIa:''' [[glycoprotein IIb IIIa inhibitor|glycoprotein IIb IIIa]]; '''LAD:''' [[left anterior descending]]; '''MI:''' [[myocardial infarction]]; '''PCI:''' [[percutaneous coronary intervention]]; '''SC:''' [[subcutaneous injection]]; '''STEMI:''' [[ST elevation myocardial infarction]]</span> | |||
Boxes in red signify that an urgent management is needed. | |||
{{Family tree/start}} | {{Family tree/start}} | ||
{{familytree | | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | A00 | | A00=<div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Identify cardinal findings of STEMI:''' <br> | ||
❑ [[Chest pain]] or [[chest discomfort]] <br> | ❑ '''[[Chest pain|<span style="color:white;"> Chest pain</span>]] or [[chest discomfort|<span style="color:white;">chest discomfort</span>]]''' <br> | ||
:❑ Sudden onset | :❑ Sudden onset | ||
:❑ Sensation of tightness, pressure, or squeezing | :❑ Sensation of heaviness, tightness, pressure, or squeezing | ||
:❑ Duration> 20 minutes <br> | :❑ Duration> 20 minutes <br> | ||
:❑ Radiation to the left arm, jaw, neck, right arm, back or [[epigastrium]] | :❑ Radiation to the left arm, jaw, neck, right arm, back or [[epigastrium|<span style="color:white;">epigastrium</span>]] | ||
:❑ No relief with medications<br> | :❑ No relief with medications<br> | ||
:❑ No relief with rest <br> | :❑ No relief with rest <br> | ||
:❑ Worse with time <br> | :❑ Worse with time <br> | ||
❑ | :❑ Worse with exertion<br> | ||
❑ [[ | :❑ Associated symptoms of [[palpitations|<span style="color:white;">palpitations</span>]], [[nausea|<span style="color:white;">nausea</span>]], [[vomiting|<span style="color:white;">vomiting</span>]] and [[sweating|<span style="color:white;">sweating</span>]] | ||
❑ '''Characteristic [[ECG|<span style="color:white;">ECG</span>]] changes consistent with [[STEMI|<span style="color:white;">STEMI</span>]]''' | |||
:❑ [[ST elevation|<span style="color:white;">ST elevation</span>]] in at least 2 contiguous leads of 2 mm (0.2 mV) in men or 1.5 mm (0.15 mV) in women in leads V2–V3 and/or of 1 mm (0.1mV) in other contiguous chest leads or the limb leads | |||
:❑ [[ST depression|<span style="color:white;">ST depression</span>]] in at least two precordial leads V1-V4 (suggestive of [[posterior myocardial infarction|<span style="color:white;">posterior MI</span>]]) | |||
:❑ [[ST depression|<span style="color:white;">ST depression</span>]] in several leads plus [[ST elevation|<span style="color:white;">ST elevation</span>]] in lead aVR (suggestive of occlusion of the [[left main|<span style="color:white;">left main</span>]] or proximal [[LAD|<span style="color:white;">LAD</span>]] artery) | |||
:❑ New [[LBBB|<span style="color:white;">LBBB</span>]]<br> | |||
''Click [[STEMI resident survival guide#Gallery|<span style="color:white;">here </span>]] for the gallery of ECG examples below.'' | |||
< | ❑ '''Increase in [[troponin|<span style="color:white;">troponin</span>]] and / or [[CKMB|<span style="color:white;">CK MB </span>]]'''</div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G02 | G02= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Rule out life threatening alternative diagnoses:'''<br> | |||
❑ [[Aortic dissection|<span style="color:white;">Aortic dissection</span>]] <br> (suggestive findings: [[back pain|<span style="color:white;">back pain</span>]], [[interscapular pain|<span style="color:white;">interscapular pain</span>]], [[aortic regurgitation|<span style="color:white;">aortic regurgitation</span>]], [[pulsus paradoxus|<span style="color:white;">pulsus paradoxus</span>]], [[blood pressure|<span style="color:white;">blood pressure</span>]] discrepancy between the arms) <br> | |||
❑ [[Pulmonary embolism|<span style="color:white;">Pulmonary embolism</span>]] <br> (suggestive findings: acute onset of [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachypnea|<span style="color:white;">tachypnea</span>]], [[hemoptysis|<span style="color:white;">hemoptysis</span>]], previous [[DVT|<span style="color:white;">DVT</span>]]) <br> | |||
❑ [[Cardiac tamponade|<span style="color:white;">Cardiac tamponade</span>]] <br> (suggestive findings: [[hypotension|<span style="color:white;">hypotension</span>]], [[jugular venous distention|<span style="color:white;">jugular venous distention</span>]], [[muffled heart sounds|<span style="color:white;">muffled heart sounds</span>]], [[pulsus paradoxus|<span style="color:white;">pulsus paradoxus</span>]])<br> | |||
❑ [[Tension pneumothorax|<span style="color:white;">Tension pneumothorax</span>]] <br> (suggestive findings: sudden [[dyspnea|<span style="color:white;">dyspnea</span>]], [[tachycardia|<span style="color:white;">tachycardia</span>]], [[trauma|<span style="color:white;">chest trauma</span>]], unilateral absence of [[breath sounds|<span style="color:white;">breath sound</span>]])<br> | |||
❑ [[Esophageal rupture|<span style="color:white;">Esophageal rupture</span>]] <br> (suggestive findings: [[vomiting|<span style="color:white;">vomiting</span>]], [[subcutaneous emphysema|<span style="color:white;">subcutaneous emphysema</span>]])</div>}} | |||
:❑ [[ | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Assess appropriateness of patients for perfusion therapy:''' | |||
❑ [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">Contraindications to fibrinolytics</span>]] [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">(click here for the complete list shown below)</span>]] <br> | |||
❑ Assess the [[femoral pulse|<span style="color:white;">femoral pulses</span>]] (strength, [[bruit|<span style="color:white;">bruit</span>]]) <br> | |||
❑ [[Pericarditis resident survival guide|<span style="color:white;">Pericarditis</span>]] (suggestive finding: [[Pericarditis resident survival guide|<span style="color:white;">pericardial friction rub</span>]])<br> </div> }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | G01 | G01= <div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Consider [[RVMI|<span style="color:white;">right ventricular MI</span>]] in case of:''' | |||
❑ [[Hypotension|<span style="color:white;">Hypotension</span>]]<br> | |||
❑ Elevated [[jugular venous pressure|<span style="color:white;">jugular venous pressure</span>]]<br> | |||
❑ Clear lung fields<br> | |||
❑ [[Peripheral edema|<span style="color:white;">Peripheral edema</span>]] <br> | |||
❑ [[ECG|<span style="color:white;">ECG</span>]] changes suggestive of an [[inferior MI|<span style="color:white;">inferior MI</span>]] <br> | |||
:❑ [[ST elevation|<span style="color:white;">ST elevation</span>]] in leads [[Electrocardiogram#Limb Leads|<span style="color:white;">II</span>]], [[Electrocardiogram#Limb Leads|<span style="color:white;">III</span>]] and [[Electrocardiogram#Limb Leads|<span style="color:white;">aVF</span>]] </div>}} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | }} | |||
❑ [[ | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | H01 | H01= <div style="float: left; text-align: left; width: 35em; padding:1em;">'''Order a right sided ECG in all patients with [[ST elevation|<span style="color:white;">ST elevation</span>]] in leads [[Electrocardiogram#Limb Leads|<span style="color:white;">II</span>]], [[Electrocardiogram#Limb Leads|<span style="color:white;">III</span>]] and [[Electrocardiogram#Limb Leads|<span style="color:white;">aVF</span>]]:''' <br> | ||
❑ Clearly label the [[ECG|<span style="color:white;">ECG</span>]] as right sided <br> | |||
❑ [[ST elevation|<span style="color:white;">ST elevation</span>]] of >1 mm in lead V4R suggests a [[right ventricular MI|<span style="color:white;">right ventricular MI</span>]] | |||
<br><br> | |||
''' | '''[[Right ventricular myocardial infarction resident survival guide|<span style="color:white;">Click here for right ventricular myocardial infarction resident survival guide</span>]]'''</div>}} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | I01 | | | I01= <div style="float: left; text-align: left; width: 35em; padding:1em;">'''Check for hypoperfusion and [[left ventricular failure|<span style="color:white;">left ventricular failure </span>]]:'''<br> | |||
❑ [[Hypotension|<span style="color:white;">Hypotension</span>]] <br> | |||
❑ [[Tachycardia|<span style="color:white;">Tachycardia</span>]] <br> | |||
: | ❑ [[Cyanosis|<span style="color:white;">Cyanotic skin and nail bed</span>]] <br> | ||
❑ [[Clammy skin|<span style="color:white;">Cold skin</span>]] <br> | |||
❑ [[Skin mottling|<span style="color:white;">Skin mottling</span>]] <br> | |||
: | ❑ Patient lies still <br> | ||
: | ❑ [[Confusion|<span style="color:white;">Confusion</span>]] or [[disorientation|<span style="color:white;">disorientation</span>]] | ||
<br><br> | |||
''' | '''[[Cardiogenic shock resident survival guide|<span style="color:white;">Click here for cardiogenic shock resident survival guide</span>]]'''</div>}} | ||
❑ | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | }} | ||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | A01 | | | | | A01= <div style="float: left; text-align: left; width: 25em; padding:1em;">'''Begin initial treatment:'''<br> ❑ Administer 162 - 325 mg of non enteric [[aspirin|<span style="color:white;">aspirin</span>]] | |||
:❑ Orally, crushed or chewed, OR | |||
: | |||
</ | |||
❑ [[ | |||
: | |||
{{familytree | |||
❑ | |||
: | |||
: | |||
: | |||
</div>}} | |||
{{ | |||
:❑ Intravenously | :❑ Intravenously | ||
❑ Administer 2-4 L/min | ❑ Administer 2-4 L/min [[oxygen|<span style="color:white;">oxygen</span>]] via nasal cannula when saturation <90% | ||
:❑ Caution in COPD patients | :❑ Caution in [[COPD|<span style="color:white;">COPD</span>]] patients: maintain an oxygen saturation between 88% and 92% | ||
❑ Administer [[beta-blockers]] (unless contraindicated)<br> | ❑ Administer [[beta-blockers|<span style="color:white;">beta-blockers</span>]] (unless contraindicated) and titrate to the [[heart rate|<span style="color:white;">heart rate</span>]] and [[blood pressure|<span style="color:white;">blood pressure </span>]]<br> | ||
:❑ [[Metoprolol]] IV, 5 mg every 5 min, up to 3 doses | <span style="font-size:85%;">Contraindicated in [[heart failure|<span style="color:white;">heart failure </span>]], [[AV block |<span style="color:white;">prolonged or high degree AV block </span>]], [[reactive airway disease|<span style="color:white;">reactive airway disease </span>]], high risk of [[cardiogenic shock|<span style="color:white;">cardiogenic shock </span>]] and low [[cardiac output|<span style="color:white;">cardiac output</span>]] state</span> <br> | ||
:❑ [[Carvedilol]] IV | :❑ [[Metoprolol|<span style="color:white;">Metoprolol</span>]] IV, 5 mg every 5 min, up to 3 doses | ||
❑ Administer sublingual [[nitroglycerin]] 0.4 mg every 5 minutes for a total of 3 doses<br> | :❑ [[Carvedilol|<span style="color:white;">Carvedilol</span>]] IV, 25 mg, two times a day | ||
❑ Administer IV [[morphine]] if needed | ❑ Administer sublingual [[nitroglycerin|<span style="color:white;">nitroglycerin</span>]] 0.4 mg every 5 minutes for a total of 3 doses<br> | ||
:❑ Initial dose | <span style="font-size:85%;">Contraindicated in suspected [[RVMI|<span style="color:white;">right ventricular MI </span>]], recent use of [[phosphodiesterase inhibitors|<span style="color:white;">phosphodiesterase inhibitors </span>]], decreased [[blood pressure|<span style="color:white;">blood pressure </span>]] 30 mmHg below baseline</span> <br> | ||
❑ Administer IV [[morphine|<span style="color:white;">morphine</span>]] if needed | |||
:❑ Initial dose 4-8 mg | |||
:❑ 2-8 mg every 5 to 15 minutes, as needed <br> | :❑ 2-8 mg every 5 to 15 minutes, as needed <br> | ||
❑ Administer 80 mg [[atorvastatin]] <br> | ❑ Administer 80 mg [[atorvastatin|<span style="color:white;">atorvastatin</span>]] <br> | ||
❑ Monitor with a 12-lead [[ | ❑ Monitor with a 12-lead [[ECG|<span style="color:white;">ECG</span>]] all the time | ||
</div>}} | </div>}} | ||
{{familytree | | | | |!| | | | | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | |!| | | | | | }} | ||
{{familytree | | | | B01 | | | | | | B01=<div style="float: left; text-align: center; width: 25em; padding:1em;">''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | | | | B01 | | | | | | B01=<div style="float: left; text-align: center; width: 25em; padding:1em;">'''Is PCI available?''' </div>}} | ||
{{familytree | |,|-|-|^|-|-|.| | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |,|-|-|^|-|-|.| | }} | ||
{{familytree | C01 | | | | C02 | | | C01=<div style="float: left; text-align: center; width: 25em; padding:1em;">''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | C01 | | | | C02 | | | C01=<div style="float: left; text-align: center; width: 25em; padding:1em;">'''YES''' </div>| C02= <div style="float: left; text-align: center; width: 25em; padding:1em;">'''NO''' </div> }} | ||
{{familytree | |!| | | |,|-|^|-|.| | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | | | |!| | }} | ||
{{familytree | |!| | | C03 | | C04 | C03= | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | | | C00 | | C00= '''Is first medical contact to device ≤ 120 min?''' }} | ||
{{familytree | |!| | | |!| | | |!| | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |,|-|^|-|.| | }} | ||
{{familytree | D01 | | D02 | | D03 | |D01=<div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''Primary PCI within 90 minutes''' <br></div> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | C03 | | C04 | C03= '''NO''' | C04= '''YES'''}} | ||
| D02= <div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''Fibrinolytic therapy within 30 min''' </div> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | |!| | }} | ||
| D03= <div style="float: left; text-align: center; width: 15em; padding:1em;">❑ '''Transfer for primary PCI''' </div> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | D01 | | D02 | | D03 | |D01=<div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''[[Primary PCI|<span style="color:white;">Primary PCI</span>]] within 90 minutes''' <br></div> | ||
| D02= <div style="float: left; text-align: center; width: 25em; padding:1em;">❑ '''[[Fibrinolytic therapy|<span style="color:white;">Fibrinolytic therapy</span>]] within 30 min''' </div> | |||
| D03= <div style="float: left; text-align: center; width: 15em; padding:1em;">❑ '''Transfer for [[primary PCI|<span style="color:white;">primary PCI </span>]]''' </div> | |||
}} | }} | ||
{{familytree | |!| | | |!| | | | | }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| | | | | }} | ||
{{familytree | E01 | | E02 | E01= <div style="float: left; text-align: left; width: 25em; padding:1em;">'''Confirm that the patient has one of the following indications:'''<br> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | E01 | | E02 | E01= <div style="float: left; text-align: left; width: 25em; padding:1em;">'''Confirm that the patient has one of the following indications:'''<br> | ||
❑ Symptoms of [[ischemia]] <12 hours ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]) <br> | ❑ Symptoms of [[ischemia|<span style="color:white;">ischemia</span>]] <12 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence A</span>]]) <br> | ||
❑ Symptoms of [[ischemia]] <12 hours and contraindications to fibrinolytics irrespective of time delay ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]])<br> | ❑ Symptoms of [[ischemia|<span style="color:white;">ischemia</span>]] <12 hours and [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">contraindications to fibrinolytics</span>]] irrespective of time delay ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]])<br> | ||
❑ [[Cardiogenic shock]] irrespective of time delay ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]])<br> | ❑ [[Cardiogenic shock|<span style="color:white;">Cardiogenic shock</span>]] irrespective of time delay ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]])<br> | ||
❑ [[Heart failure]] irrespective of time delay ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) <br> | ❑ [[Heart failure|<span style="color:white;">Heart failure</span>]] irrespective of time delay ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ||
❑ Ongoing [[ischemia]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence B]])<br></div> | ❑ Ongoing [[ischemia|<span style="color:white;">ischemia</span>]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]])<br></div> | ||
| E02 =<div style="float: left; text-align: left; width: 25em; padding:1em;"> ❑ '''Confirm that the patient has one of the following indications:'''<br> | | E02 =<div style="float: left; text-align: left; width: 25em; padding:1em;"> ❑ '''Confirm that the patient has one of the following indications:'''<br> | ||
:❑ Symptoms of [[ischemia]] <12 hours ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]) <br> | :❑ Symptoms of [[ischemia|<span style="color:white;">ischemia</span>]] <12 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence A</span>]]) <br> | ||
:❑ Ongoing [[ischemia]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence C]])<br> | :❑ Ongoing [[ischemia|<span style="color:white;">ischemia</span>]] 12-24 hours following onset ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence C</span>]])<br> | ||
❑ '''Confirm that the patient has no contraindications for | ❑ '''Confirm that the patient has no [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">contraindications to fibrinolytics</span>]] [[STEMI resident survival guide#Contraindications to Fibrinolytic Therapy|<span style="color:white;">(click here for the complete list shown below)</span>]] <br>''' | ||
</div>}} | </div>}} | ||
{{familytree | |!| | | |!| }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| }} | ||
{{familytree | F01 | | F03 |F01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | F01 | | F03 |F01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> | ||
'''Administer ONE of the following antiplatelet agents (before or at the time of PCI):''' <br> | '''Administer ONE of the following antiplatelet agents (before or at the time of PCI):''' <br> | ||
❑ [[P2Y12]] receptor inhibitors <br> | ❑ [[P2Y12|<span style="color:white;">P2Y12</span>]] receptor inhibitors <br> | ||
:❑ [[Clopidogrel]] 600 mg | :❑ [[Clopidogrel|<span style="color:white;">Clopidogrel</span>]] 600 mg | ||
:❑ [[Ticagrelor]] 180 mg | :❑ [[Ticagrelor|<span style="color:white;">Ticagrelor</span>]] 180 mg | ||
:❑ [[Prasugrel]] 60 mg | :❑ [[Prasugrel|<span style="color:white;">Prasugrel</span>]] 60 mg <br> | ||
❑ IV [[GP IIb/IIIa]] | <span style="font-size:85%;">Prasugrel is contraindicated in case of prior history of strokes or TIAs, active pathological bleeding, age ≥75 years, when urgent coronary artery bypass graft surgery (CABG) is likely, body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding </span> <br> | ||
:❑ [[Abciximab]]<br> | ❑ IV [[GP IIb/IIIa inhibitors|<span style="color:white;">GP IIb/IIIa inhibitors</span>]] <br> | ||
:❑ [[Abciximab|<span style="color:white;">Abciximab</span>]]<br> | |||
::❑ Loading dose 0.25 mg/kg IV bolus <br> | ::❑ Loading dose 0.25 mg/kg IV bolus <br> | ||
::❑ Maintenance dose 0.125 mg/kg/min <br> | ::❑ Maintenance dose 0.125 mg/kg/min <br> | ||
:❑ [[Eptifibatide]]<br> | :❑ [[Eptifibatide|<span style="color:white;">Eptifibatide</span>]]<br> | ||
::❑ Loading dose 180 mcg/kg IV bolus | ::❑ Loading dose 180 mcg/kg IV bolus | ||
::❑ Another 180 mcg/kg IV bolus after 10 minutes<br> | ::❑ Another 180 mcg/kg IV bolus after 10 minutes<br> | ||
| Line 189: | Line 171: | ||
::❑ Decrease infusion by 50% if creatinine clearance <50 mL/min | ::❑ Decrease infusion by 50% if creatinine clearance <50 mL/min | ||
::❑ Avoid in hemodialysis patients | ::❑ Avoid in hemodialysis patients | ||
:❑ [[Tirofiban]] <br> | :❑ [[Tirofiban|<span style="color:white;">Tirofiban</span>]] <br> | ||
::❑ Loading dose 25 mcg/kg<br> | ::❑ Loading dose 25 mcg/kg<br> | ||
::❑ Maintenance dose 0.15 mcg/kg/min | ::❑ Maintenance dose 0.15 mcg/kg/min | ||
::❑ Decrease infusion by 50% if creatinine clearance <30 mL/min | ::❑ Decrease infusion by 50% if [[creatinine|<span style="color:white;">creatinine</span>]] clearance <30 mL/min | ||
---- | ---- | ||
'''Administer ONE of the following anticoagulant therapy:'''<br> | '''Administer ONE of the following anticoagulant therapy:'''<br> | ||
❑ [[UFH|Unfractionated heparin]] <br> | ❑ [[UFH|<span style="color:white;">Unfractionated heparin</span>]] <br> | ||
:♦ ''If GP IIb/IIIa receptor antagonist is planned'' | :♦ ''If GP IIb/IIIa receptor antagonist is planned'' | ||
:❑ 50- to 70-U/kg IV bolus <br> | :❑ 50- to 70-U/kg IV bolus <br> | ||
:♦ ''If no GP IIb/IIIa receptor antagonist is planned'' | :♦ ''If no GP IIb/IIIa receptor antagonist is planned'' | ||
:❑ 70- to 100-U/kg bolus <br> | :❑ 70- to 100-U/kg bolus <br> | ||
❑ [[Bivalirudin]] | ❑ [[Bivalirudin|<span style="color:white;">Bivalirudin</span>]] | ||
::❑ 0.75-mg/kg IV bolus, then 1.75–mg/kg/h infusion | ::❑ 0.75-mg/kg IV bolus, then 1.75–mg/kg/h infusion | ||
::❑ Additional bolus of 0.3 mg/kg if needed | ::❑ Additional bolus of 0.3 mg/kg if needed | ||
::❑ Decrease infusion to 1 mg/kg/h when creatinine clearance <30 mL/min | ::❑ Decrease infusion to 1 mg/kg/h when [[creatinine|<span style="color:white;">creatinine</span>]] clearance <30 mL/min | ||
</div> | </div> | ||
| F03=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Administer ONE of the following fibrinolytic therapy''' <br> | | F03=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Administer ONE of the following [[fibrinolytic therapy|<span style="color:white;">fibrinolytic therapy</span>]]:''' <br> | ||
❑ [[Tenecteplase]] single IV bolus | ❑ [[Tenecteplase|<span style="color:white;">Tenecteplase</span>]] single IV bolus | ||
:❑ 30 mg for weight <60 kg | :❑ 30 mg for weight <60 kg | ||
:❑ 35 mg for weight 60-69 kg | :❑ 35 mg for weight 60-69 kg | ||
:❑ 40 mg for weight 70-79 kg | :❑ 40 mg for weight 70-79 kg | ||
:❑ 45 mg for weight 80-89 kg | :❑ 45 mg for weight 80-89 kg | ||
:❑ 50 mg for weight | :❑ 50 mg for weight ≥90 kg<ref name="pmid11136484">{{cite journal| author=Wang-Clow F, Fox NL, Cannon CP, Gibson CM, Berioli S, Bluhmki E et al.| title=Determination of a weight-adjusted dose of TNK-tissue plasminogen activator. | journal=Am Heart J | year= 2001 | volume= 141 | issue= 1 | pages= 33-40 | pmid=11136484 | doi=10.1067/mhj.2001.112092 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11136484 }} </ref> | ||
❑ [[Reteplase]] 10 units IV boluses every 30 min <br> | ❑ [[Reteplase|<span style="color:white;">Reteplase</span>]] 10 units IV boluses every 30 min <br> | ||
❑ [[Alteplase]] | ❑ [[Alteplase|<span style="color:white;">Alteplase</span>]] | ||
:❑ Bolus 15 mg, infusion 0.75 mg/kg for 30 min (maximum 50 mg) | :❑ Bolus 15 mg, infusion 0.75 mg/kg for 30 min (maximum 50 mg) | ||
:❑ Then 0.5 mg/kg (maximum 35 mg) over the next 60 min | :❑ Then 0.5 mg/kg (maximum 35 mg) over the next 60 min | ||
❑ [[Streptokinase]] 1.5 million units IV administered over 30-60 min | ❑ [[Streptokinase|<span style="color:white;">Streptokinase</span>]] 1.5 million units IV administered over 30-60 min | ||
---- | ---- | ||
'''Administer a | '''Administer a [[Antiplatelet drugs|<span style="color:white;">P2Y12</span>]] inhibitor:''' <br> | ||
❑ [[Clopidogrel]] <br> | ❑ [[Clopidogrel|<span style="color:white;">Clopidogrel</span>]] <br> | ||
:♦ ''If age ≤ 75 years'' | :♦ ''If age ≤ 75 years'' | ||
:❑ Loading dose 300 mg | :❑ Loading dose 300 mg | ||
| Line 227: | Line 209: | ||
:❑ 75 mg daily for at least 14 days, up to one year | :❑ 75 mg daily for at least 14 days, up to one year | ||
---- | ---- | ||
'''Administer ONE of the following anticoagulant therapy''' <br> | '''Administer ONE of the following anticoagulant therapy:''' <br> | ||
❑ [[UFH|Unfractionated heparin]] <br> | ❑ [[UFH|<span style="color:white;">Unfractionated heparin</span>]] <br> | ||
:❑ IV bolus of 60 units/kg (maximum 4000 units) | :❑ IV bolus of 60 units/kg (maximum 4000 units) | ||
:❑ Then infusion of 12 units/kg/hour (maximum 1000 units) | :❑ Then infusion of 12 units/kg/hour (maximum 1000 units) | ||
:❑ Adjust the infusion for a aPTT of 50-70 sec for 48 hours or until revascularization | :❑ Adjust the infusion for a aPTT of 50-70 sec for 48 hours or until revascularization | ||
❑ [[Enoxaparin]] (for up to 8 days or until revascularization)<br> | ❑ [[Enoxaparin|<span style="color:white;">Enoxaparin</span>]] (for up to 8 days or until revascularization)<br> | ||
:'' If age <75 years'' | :'' If age <75 years'' | ||
:❑ IV bolus 30 mg | :❑ IV bolus 30 mg | ||
| Line 240: | Line 222: | ||
:♦ ''If creatinine clearance <30 mL/min'' | :♦ ''If creatinine clearance <30 mL/min'' | ||
:❑ SC 1 mg/kg every 24 hours | :❑ SC 1 mg/kg every 24 hours | ||
❑ [[Fondaparinux]] | ❑ [[Fondaparinux|<span style="color:white;">Fondaparinux</span>]] | ||
:❑ Initial dose of 2.5 mg IV | :❑ Initial dose of 2.5 mg IV | ||
:❑ Then, SC 2.5 mg daily (for up to 8 days or until revascularization) | :❑ Then, SC 2.5 mg daily (for up to 8 days or until revascularization) | ||
:❑ Do not administer if creatinine clearance <30 mL/min | :❑ Do not administer if creatinine clearance <30 mL/min | ||
</div>}} | </div>}} | ||
{{familytree | |!| | | |!| }} | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | |!| | | |!| }} | ||
{{familytree | G01 | | G02 | G01= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Consider urgent CABG if the coronary anatomy is not amenable to PCI and one of the following:'''<br> | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF; | G01 | | G02 | G01= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Consider urgent [[CABG|<span style="color:white;">CABG</span>]] if the coronary anatomy is not amenable to PCI and one of the following:'''<br> | ||
❑ Ongoing and recurrent [[ischemia]] <br> | ❑ Ongoing and recurrent [[ischemia|<span style="color:white;">ischemia</span>]] <br> | ||
❑ [[Cardiogenic shock]] <br> | ❑ [[Cardiogenic shock|<span style="color:white;">Cardiogenic shock</span>]] <br> | ||
❑ Severe [[heart failure]] <br> | ❑ Severe [[heart failure|<span style="color:white;">heart failure</span>]] <br> | ||
❑ Other high risk features | ❑ Other high risk features | ||
</div> | </div> | ||
|G02= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Transfer to a PCI- | |G02= <div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Transfer to a PCI-capable hospital for non primary PCI, if there is:''' <br> | ||
❑ [[Cardiogenic shock]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) <br> | ❑ [[Cardiogenic shock|<span style="color:white;">Cardiogenic shock</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ||
❑ Acute severe [[heart failure]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) <br> | ❑ Acute severe [[heart failure|<span style="color:white;">heart failure</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence B</span>]]) <br> | ||
❑ Spontaneous or easily provoked myocardial ischemia ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]) <br> | ❑ Spontaneous or easily provoked myocardial ischemia ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class I, level of evidence C</span>]]) <br> | ||
❑ Failed reperfusion after fibrinolytics ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence B]]) <br> | ❑ Failed reperfusion after [[fibrinolytic therapy|<span style="color:white;">fibrinolytics</span>]] ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ||
❑ Reocclusion after fibrinolytics ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence B]]) <br> | ❑ Reocclusion after [[fibrinolytic therapy|<span style="color:white;">fibrinolytics</span>]]([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) <br> | ||
❑ Successful fibrinolytic reperfusion, between 3 and 24 hours ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence B]]) | ❑ Successful fibrinolytic reperfusion, between 3 and 24 hours ([[ACC AHA guidelines classification scheme|<span style="color:white;">Class IIa, level of evidence B</span>]]) | ||
</div> }} | </div> }} | ||
{{familytree/end}} | {{familytree/end}} | ||
<br> | |||
<br> | |||
===Contraindications to Fibrinolytic Therapy=== | ===Contraindications to Fibrinolytic Therapy=== | ||
Shown below is a table summarizing the absolute and relative contraindications | Shown below is a table summarizing the absolute and relative contraindications to [[fibrinolytic therapy]] among [[STEMI]] patients. | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |- | ||
| Line 269: | Line 253: | ||
|- | |- | ||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |❑ Prior [[intracranial hemorrhage]] <br> | | style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left |❑ Prior [[intracranial hemorrhage]] <br> | ||
❑ [[Ischemic stroke]] within the last 3 months ( | ❑ [[Ischemic stroke]] within the last 3 months (unless within 4.5 hours)<br> | ||
❑ Structural cerebral vascular lesion<br> | ❑ Structural cerebral vascular lesion<br> | ||
❑ Primary | ❑ Primary or [[metastasis|metastatic]] intracranial [[malignancy]] <br> | ||
❑ Suspicion of [[aortic dissection]]<br> | ❑ Suspicion of [[aortic dissection]]<br> | ||
❑ Increased bleeding tendency or active bleeding <br> | ❑ Increased bleeding tendency or active [[bleeding]] <br> | ||
❑ Severe head or facial [[trauma]] within the last 3 months <br> | ❑ Severe head or facial [[trauma]] within the last 3 months <br> | ||
❑ Intracranial or intraspinal surgery within the last 2 months <br> | ❑ Intracranial or intraspinal surgery within the last 2 months <br> | ||
❑ Severe [[hypertension]] uncontrolled by emergency therapy <br> | ❑ Severe [[hypertension]] uncontrolled by emergency therapy <br> | ||
❑ Previous treatment with [[streptokinase]] within the last 6 months | ❑ Previous treatment with [[streptokinase]] within the last 6 months | ||
| style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ❑ Oral anticoagulation therapy <br> | | style="font-size: 90%; padding: 0 5px; background: #DCDCDC" align=left | ❑ [[Oral anticoagulation therapy]] <br> | ||
❑ Pregnancy <br> | ❑ [[Pregnancy]] <br> | ||
❑ Active [[peptic ulcer]] <br> | ❑ Active [[peptic ulcer]] <br> | ||
❑ Previous history of chronic severe [[hypertension]] that is poorly controlled<br> | ❑ Previous history of chronic severe [[hypertension]] that is poorly controlled<br> | ||
❑ Elevated [[blood pressure]] at presentation, such as [[ | ❑ Elevated [[blood pressure]] at presentation, such as [[systolic blood pressure]] >180 mmHg or [[diastolic blood pressure]] >110mmHg<br> | ||
❑ Previous history of [[ischemic stroke]] <br> | ❑ Previous history of [[ischemic stroke]] <br> | ||
❑ [[Dementia]] <br> | ❑ [[Dementia]] <br> | ||
| Line 288: | Line 272: | ||
❑ [[CPR]] that lasted more than 10 min or that is traumatic <br> | ❑ [[CPR]] that lasted more than 10 min or that is traumatic <br> | ||
❑ Major surgery in the last 3 weeks <br> | ❑ Major surgery in the last 3 weeks <br> | ||
❑ Internal bleeding within the last 2-4 weeks <br> | ❑ Internal [[bleeding]] within the last 2-4 weeks <br> | ||
❑ Non compressible vascular punctures | ❑ Non compressible vascular punctures | ||
|} | |} | ||
=== | ==Complete Diagnostic Approach== | ||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | |||
<span style="font-size:85%"> '''Abbreviations:''' '''CABG:''' [[coronary artery bypass graft]]; '''ECG:''' [[electrocardiogram]]; '''LAD:''' [[LAD|left anterior descending]]; '''LBBB:''' [[left bundle branch block]]; '''MI:''' [[myocardial infarction]]; '''PCI:''' [[percutaneous coronary intervention]]; '''S3:''' [[S3|third heart sound]]; '''S4:''' [[S4|fourth heart sound]]; '''VSD:''' [[ventricular septal defect]] </span> | |||
{{Family tree/start}} | {{Family tree/start}} | ||
{{familytree | A01 | | |A01= <div style="float: left; text-align: left; width: 30em; padding:1em;">'''Administer the following medications | {{familytree | A01 | | A01=<div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Characterize the symptoms:''' <br> | ||
❑ [[Chest pain]] or [[chest discomfort]] <br> | |||
:❑ Sudden onset | |||
:❑ Sensation of heaviness, tightness, pressure, or squeezing | |||
:❑ Duration> 20 minutes <br> | |||
:❑ Radiation to the left arm, jaw, neck, right arm, back or [[epigastrium]] | |||
:❑ No relief with medications<br> | |||
:❑ No relief with rest <br> | |||
:❑ Worse with time <br> | |||
:❑ Worse with exertion<br> | |||
❑ [[Dyspnea]] <br> | |||
❑ [[Weakness]] <br> | |||
❑ [[Palpitations]] <br> | |||
❑ [[Nausea]] <br> | |||
❑ [[Vomiting]] <br> | |||
❑ [[Sweating]] <br> | |||
❑ [[Loss of consciousness]]<br> | |||
❑ [[Fatigue]] | |||
</div>}} | |||
{{familytree | |!| | |}} | |||
{{familytree | B01 | | B01=<div style="float: left; text-align: left; width: 35em; padding:1em;"> '''Obtain a detailed history:''' <br> | |||
❑ Age <br> | |||
❑ Baseline [[blood pressure]] <br> | |||
❑ Previous [[MI]] <br> | |||
❑ Previous [[PCI]] or [[CABG]] <br> | |||
❑ Cardiac risk factors<br> | |||
:❑ [[Hypertension]] <br> | |||
:❑ [[Diabetes]] <br> | |||
:❑ [[Hypercholesterolemia]] <br> | |||
:❑ [[Smoking]] <br> | |||
:❑ [[Obesity]] <br> | |||
❑ List of medications <br> | |||
❑ Family history of premature [[coronary artery disease]] | |||
---- | |||
'''Identify possible triggers:'''<br> | |||
❑ Physical exertion <br> | |||
❑ [[Stress|Psychological stress]] (anger, anxiety, bereavement, work related stress, natural disasters, wars or sporting events) <br> | |||
❑ [[Sexual activity]] <br> | |||
❑ Air pollution or fine particulate matter <br> | |||
❑ Antecedant infection <br> | |||
❑ Heavy meal <br> | |||
❑ [[Cocaine]] <br> | |||
❑ [[Marijuana]]</div>}} | |||
{{familytree | |!| | | }} | |||
{{familytree | C01 | | C01=<div style="float: left; text-align: left; width: 35em; padding:1em;">'''Examine the patient:''' <br> | |||
'''Vital signs''' <br> | |||
❑ [[Blood pressure]] <br> | |||
:❑ [[Blood pressure]] lower than baseline, suggestive of: | |||
::❑ [[Cardiogenic shock]] (associated with [[tachycardia]] and end organ hypoperfusion), or | |||
::❑ [[Right ventricular MI]] (associated with increased [[jugular venous pressure]] and clear lung fields), or | |||
::❑ [[Bezold-Jarisch reflex]] (associated with either normal [[heart rate]] or [[bradycardia]]) | |||
:❑ Discrepancy between arms (suggestive of [[aortic dissection]]) | |||
:❑ Narrow [[pulse pressure]] (suggestive of [[heart failure]]) | |||
:❑ Wide [[pulse pressure]] (suggestive of [[mitral regurgitation]] or [[VSD]]) | |||
❑ [[Heart rate]] <br> | |||
:❑ [[Tachycardia]] (suggestive of [[heart failure]]) | |||
:❑ [[Bradycardia]] (suggestive of [[heart block]]) | |||
'''Pulses''' <br> | |||
❑ [[Femoral artery|Femoral pulse]] (if a patient is to undergo [[PCI]])<br> | |||
:❑ Strength | |||
:❑ [[Bruits]] | |||
'''Skin''' <br> | |||
❑ [[Xanthelasma]] (suggestive of [[dyslipidemia]]) <br> | |||
❑ [[Xanthoma]] (suggestive of [[dyslipidemia]]) <br> | |||
❑ [[Edema]] (suggestive of [[heart failure]])<br> | |||
❑ [[Cyanosis|Cyanotic]] and cold skin, lips, nail bed (suggestive of [[cardiogenic shock]]) <br> | |||
'''Heart''' <br> | |||
❑ [[Heart sounds]]<br> | |||
:❑ [[S3]] (suggestive of [[heart failure]]) | |||
:❑ [[S4]] (associated with conditions that increase the stiffness of the ventricle) | |||
❑ [[Murmurs]] | |||
:❑ [[Mitral regurgitation]]: blowing holosystolic murmur best heard at the apex | |||
:❑ [[VSD]]: holosystolic murmur along the left and right sternal border | |||
:❑ [[Free wall rupture]]: holosytolic murmur | |||
:❑ [[Aortic regurgitation]]: early diastolic high-pitched sound best heard at the left sternal border (suggestive of [[aortic dissection]] with propagation to the aortic arch) | |||
❑ [[Friction rub|Pericardial friction rub]] (suggestive of [[pericarditis]]) | |||
'''Signs of right ventricular MI:'''<br> | |||
❑ Elevated [[jugular venous pressure]]<br> | |||
❑ Presence of [[hepatojugular reflux]]<br> | |||
'''Lungs''' <br> | |||
❑ [[Rales]] (suggestive of [[heart failure]]) <br> | |||
</div>}} | |||
{{Family tree/end}} | |||
==Pre-Discharge Care== | |||
<span style="font-size:85%"> '''Abbreviations:''' '''ACE:''' [[angiotensin converting enzyme]]; '''LVEF:''' [[left ventricular ejection fraction]]; '''MI:''' [[myocardial infarction]]; '''PCI:''' [[percutaneous coronary intervention]]; '''PO:''' per os; '''STEMI:''' [[ST elevation myocardial infarction]]; '''VF:''' [[ventricular fibrillation]]; '''VT:''' [[ventricular tachycardia]] </span> | |||
{{Family tree/start}} | |||
{{familytree | A01 | | |A01= <div style="float: left; text-align: left; width: 30em; padding:1em;">'''Administer the following medications in patients without contraindications:'''<br> | |||
❑ [[Aspirin]] 81-325 mg (indefinitely) <br> | ❑ [[Aspirin]] 81-325 mg (indefinitely) <br> | ||
❑ [[Beta blockers]] | ❑ [[Beta blockers]] <br> | ||
<span style="font-size:85%;color:red">Contraindicated in heart failure, prolonged or high degree AV block, reactive airway disease, high risk of cardiogenic shock and low cardiac output state</span> | |||
:❑ [[Metoprolol tartrate]] | :❑ [[Metoprolol tartrate]] | ||
::❑ Begin with 25 to 50 mg PO every 6 to 12 hour | ::❑ Begin with 25 to 50 mg PO every 6 to 12 hour | ||
| Line 304: | Line 388: | ||
:❑ [[Carvedilol]] | :❑ [[Carvedilol]] | ||
::❑ Begin with 6.25 mg twice daily | ::❑ Begin with 6.25 mg twice daily | ||
::❑ Titrate to 25 mg twice daily | ::❑ Titrate to 25 mg twice daily | ||
❑ [[ACE inhibitor]] | ❑ [[ACE inhibitor]] in case of [[anterior MI]], [[ejection fraction]] ≤ 40% or [[heart failure]] <br> | ||
<span style="font-size:85%;color:red">Contraindicated in hypotension, renal failure and hyperkalemia</span> | |||
:❑ [[Lisinopril]] | :❑ [[Lisinopril]] | ||
::❑ Begin with 2.5-5 mg | ::❑ Begin with 2.5-5 mg | ||
| Line 318: | Line 403: | ||
::❑ Begin with 0.5 mg daily | ::❑ Begin with 0.5 mg daily | ||
::❑ Titrate to 4 mg daily, OR | ::❑ Titrate to 4 mg daily, OR | ||
❑ [[Valsartan]] | ❑ [[Valsartan]] (in case of intolerance to [[ACE inhibitors]]) <br> | ||
<span style="font-size:85%;color:red">Contraindicated in hypotension, renal failure and hyperkalemia</span> | |||
:❑ Begin with 20 mg twice daily | :❑ Begin with 20 mg twice daily | ||
:❑ Titrate to 160 mg twice daily | :❑ Titrate to 160 mg twice daily | ||
❑ [[Atorvastatin]] 80 mg daily | ❑ [[Atorvastatin]] 80 mg daily | ||
---- | ---- | ||
| Line 332: | Line 418: | ||
'''''For patients who underwent fibrinolysis, for at least 14 days, up to one year '''<br>'' | '''''For patients who underwent fibrinolysis, for at least 14 days, up to one year '''<br>'' | ||
❑ [[Clopidogrel]] 75 mg daily | ❑ [[Clopidogrel]] 75 mg daily | ||
---- | ---- | ||
'''Manage complications of STEMI''' <br> | '''Manage complications of STEMI''' <br> | ||
❑ [[ICD|Implantable cardioverter-defibrillator]] | ❑ [[ICD|Implantable cardioverter-defibrillator]] at least 40 days following the [[MI]] in cases of:<br> | ||
❑ Temporary pacing for | :❑ [[LVEF]] <30% among patients in NYHA functional Class I ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]) | ||
:❑ [[LVEF]] <35% among patients in NYHA functional Class II or III ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]) | |||
:❑ [[LVEF]] <40% ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]])<br> | |||
:❑ An irreversible non-ischemia related [[VT]]/ [[VF]] after more than 48 hours following [[STEMI]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]])<ref name="pmid18534377">{{cite journal| author=Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS et al.| title=ACC/AHA/HRS 2008 guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: executive summary. | journal=Heart Rhythm | year= 2008 | volume= 5 | issue= 6 | pages= 934-55 | pmid=18534377 | doi=10.1016/j.hrthm.2008.04.015 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18534377 }} </ref> | |||
❑ Temporary pacing for symptomatic [[bradycardia]] refractory to medical therapy ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]])<br> | |||
❑ [[Aspirin]] for [[pericarditis]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) | ❑ [[Aspirin]] for [[pericarditis]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) | ||
:❑ do not administer [[glucocorticoids]] or [[NSAIDs]] for [[pericarditis]] following [[STEMI]] ([[ACC AHA guidelines classification scheme|Class III, level of evidence B]]) | |||
---- | |||
'''Assess the patient for ischemia:'''<br> | |||
❑ Perform non invasive testing before discharge for the evaluation of ischemia among patients who did not undergo [[coronary angiography]] and in whom [[coronary angiography]] is not warranted due to the absence of high risk features ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]) <br> | |||
❑ Assess the [[LVEF]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]) | |||
</div>}} | </div>}} | ||
{{familytree/end}} | {{familytree/end}} | ||
==Long Term Management== | |||
<span style="font-size:85%"> '''Abbreviations:''' '''ACE:''' [[angiotensin converting enzyme]]; '''ARB:''' [[angiotensin receptor blocker]]; '''MI:''' [[myocardial infarction]] </span> | |||
{{Family tree/start}} | |||
{{familytree | A01 | | A01= <div style="float: left; text-align: left; width: 30em; padding:1em;"> ❑ Prepare a list of all the home medications and educate the patient about compliance | |||
:❑ [[Aspirin]] 81-325 mg (indefinitely) | |||
:❑ [[Antiplatelet drug|Antiplatelet therapy]] | |||
:❑ Consider oral factor Xa inhibition with [[Rivaroxaban]] outside the US based upon EMA approval (Note [[Rivaroxaban]] is not FDA approved for use in ACS in the US) | |||
:❑ [[Beta blockers]] | |||
:❑ [[ACE inhibitors]] or [[ARB]] (in case of [[anterior MI]], [[ejection fraction]] ≤ 40% or [[heart failure]]) | |||
:❑ [[Atorvastatin]] 80 mg daily | |||
❑ Encourage lifestyle modification <br> | |||
:❑ [[Smoking]] cessation | |||
:❑ Physical activity | |||
:❑ Dietary changes | |||
❑ Ensure the initiation of the management of comorbidities | |||
:❑ [[Obesity]] | |||
:❑ [[Dyslipidemia]] | |||
:❑ [[Hypertension]] | |||
:❑ [[Diabetes]] | |||
:❑ [[Heart failure]] | |||
❑ Educate the patient about the early recognition of symptoms of [[MI]]<br> | |||
❑ Educate the patient about the use of [[nitroglycerin]] 0.4 mg, sublingually, up to 3 doses every 5 minutes </div> }} | |||
{{Family tree/end}} | |||
==Do's== | ==Do's== | ||
* | * A pre-hospital [[ECG]] is recommended. If [[STEMI]] is diagnosed the [[PCI]] team should be activated while the patient is en route to the hospital. | ||
* Administer reperfusion therapy for all patients presenting with [[STEMI]] within 12 hours of the beginning of the symptoms ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]). | * Administer reperfusion therapy for all patients presenting with [[STEMI]] within 12 hours of the beginning of the symptoms ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]). | ||
| Line 394: | Line 506: | ||
==Don'ts== | ==Don'ts== | ||
* Do not administer IV [[beta-blockers]] among patients with elevated risk for cardiogenic shock, signs of [[heart failure]], low ouput state, prolonged [[PR interval]] more than 0.24 seconds, second or third degree block or [[asthma]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]). | * Do not administer IV [[beta-blockers]] among patients with elevated risk for cardiogenic shock, signs of [[heart failure]], low ouput state, prolonged [[PR interval]] more than 0.24 seconds, [[second degree AV block|second]] or [[third degree block]] or [[asthma]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]]). | ||
* Do not administer IV [[GP IIb/IIIa inhibitors]] to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy. | * Do not administer IV [[GP IIb/IIIa inhibitors]] to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy. | ||
* Do not administer [[nitroglycerine]] to patients with systolic | * Do not administer [[nitroglycerine]] to patients with [[systolic blood pressure]] < 90 mm Hg or ≥ to 30 mm Hg below baseline, severe [[bradycardia]] (< 50 bpm), [[tachycardia]] (> 100 bpm), or suspected [[RVMI|right ventricular myocardial infarction]]. | ||
* Do not delay the time for reperfusion. | * Do not delay the time for reperfusion. | ||
| Line 406: | Line 518: | ||
** Active pathological bleeding | ** Active pathological bleeding | ||
** Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered) | ** Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered) | ||
** Urgent coronary artery bypass graft surgery (CABG) is likely | ** Urgent [[coronary artery bypass graft]] surgery ([[CABG]]) is likely | ||
** Presence of additional risk factors for bleeding such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | publisher = | date = | accessdate = 6 February 2014 }}</ref> | ** Presence of additional risk factors for [[bleeding]] such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of [[bleeding]]<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6 | publisher = | date = | accessdate = 6 February 2014 }}</ref> | ||
* Do not administer [[fibrinolytic therapy]] to patients with known [[cerebral arteriovenous malformation]] or to patients with suspected [[aortic dissection]]. | * Do not administer [[fibrinolytic therapy]] to patients with known history of [[intracranial hemorrhage]], [[cerebral arteriovenous malformation]] or to patients with suspected [[aortic dissection]]. | ||
* Do not withhold [[aspirin]] among patients who are planned to undergo urgent [[CABG]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]).<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | * Do not withhold [[aspirin]] among patients who are planned to undergo urgent [[CABG]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]).<ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref> | ||
==Gallery== | |||
Shown below is an EKG demonstrating the evolution of an [[infarct]] on the EKG. [[ST elevation]], [[Q wave]] formation, [[T wave inversion]], normalization with a persistent Q wave suggest STEMI. | |||
[[Image:STEMI evolution.png|center|800px]] | |||
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:AMI_evolutie.png | |||
---- | |||
Shown below is an EKG demonstrating loss of R waves throughout the anterior wall ([[Electrocardiogram#Precordial|V1]]-[[Electrocardiogram#Precordial|V6]]). QS complexes in [[Electrocardiogram#Precordial|V3]]-[[Electrocardiogram#Precordial|V5]]. [[ST elevation]] in [[Electrocardiogram#Precordial|V1]]-[[Electrocardiogram#Precordial|V5]] with terminal negative T waves. | |||
[[Image:STEMI 7.jpg|center|800px]] | |||
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page | |||
---- | |||
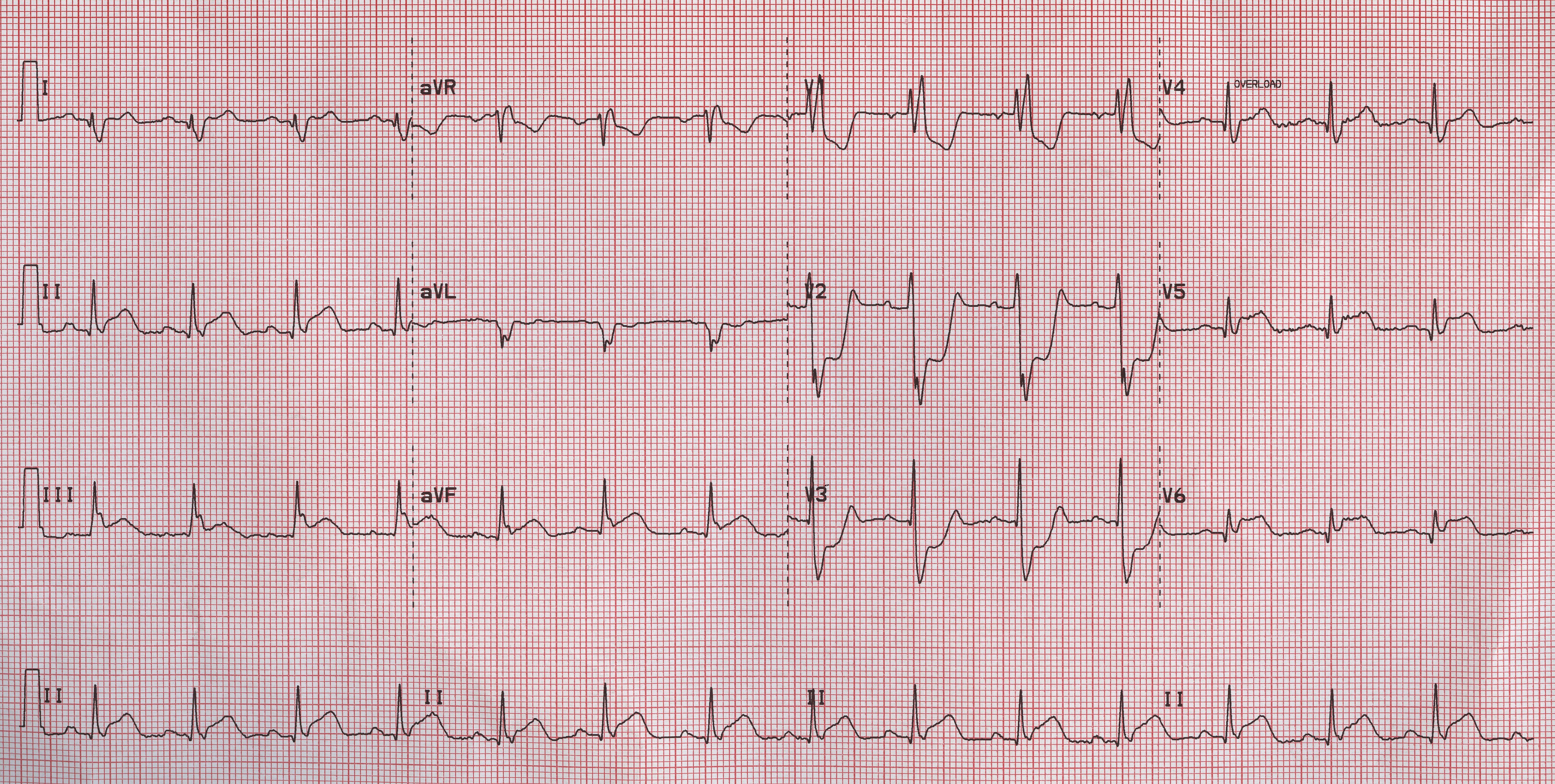
Shown below is an EKG demonstrating ST elevation in leads II, III and aVF and ST depression in leads V1, V2 and V3 depicting a [[posterior MI]]. | |||
[[Image:Posterior MI patient.jpg|center|800px]] | |||
---- | |||
Shown below is an EKG demonstrating acute MI in a patient with [[LBBB]] | |||
[[Image:STEMI 26.jpg|center|800px]] | |||
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page | |||
==References== | ==References== | ||
| Line 419: | Line 550: | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Resident survival guide]] | [[Category:Resident survival guide]] | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
</div> | |||
Latest revision as of 15:26, 8 August 2014
| STEMI Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Pre-Hospital Care |
| FIRE |
| Complete Diagnosis |
| Pre-Discharge Care |
| Long Term Management |
| Do's |
| Don'ts |
| Gallery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]; Rim Halaby, M.D. [3]
Overview
ST elevation myocardial infarction (STEMI) is a syndrome characterized by the presence of symptoms of myocardial ischemia associated with persistent ST elevation on electrocardiogram and elevated cardiac enzymes. The management of STEMI should be initiated without delay and the following timelines should be minimized (the 4 D's):
Door to Data
If a patient presents with chest discomfort, an electrocardiogram must be obtained immediately and no later than 5-10 minutes after arrival. In the patient with chest discomfort, an electrocardiogram should be obtained prior to obtaining insurance / payment information.
Data to Decision
If the electrocardiogram shows ST segment elevation, ST segment depression consistent with posterior MI, or a new left bundle branch block, a decision must be made within 5 to 10 minutes as to whether to administer a fibrinolytic agent or to proceed to primary angioplasty.
Decision to Drug or Device
Once a decision is made to administer a fibrinolytic agent or to proceed to primary angioplasty this should be carried out within 30 minutes.
Causes
Life Threatening Causes
STEMI is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Plaque rupture
- Takotsubo cardiomyopathy (also known as broken heart syndrome or stress cardiomyopathy)
- Aortic dissection with propagation to the right coronary artery
- Cocaine
Pre-Hospital Care
Pre-hospital care can begin in the ambulance by Emergency Medical Services (EMS) personnel and it can decrease the delay in the management of STEMI patients. In the United States, volunteers and fire fighters are permitted to initiate emergency care prior to the arrival of highly trained paramedics by beginning CPR and if adequately trained, can defibrillate the patient using an automatic external defibrillator. Early access to EMS is promoted by a 9-1-1 system.
Prehospital Care ❑ Check the vital signs
❑ Activate the cardiac cath team in the hospital | |||||||||
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[1]
Abbreviations: LBBB: left bundle branch block; CABG: coronary artery bypass graft; COPD: chronic obstructive pulmonary disease; DVT: deep vein thrombosis; ECG: electrocardiography; GP IIb IIIa: glycoprotein IIb IIIa; LAD: left anterior descending; MI: myocardial infarction; PCI: percutaneous coronary intervention; SC: subcutaneous injection; STEMI: ST elevation myocardial infarction
Boxes in red signify that an urgent management is needed.
Identify cardinal findings of STEMI: ❑ Chest pain or chest discomfort
❑ Characteristic ECG changes consistent with STEMI
Click here for the gallery of ECG examples below. ❑ Increase in troponin and / or CK MB | |||||||||||||||||||||||
Rule out life threatening alternative diagnoses: ❑ Aortic dissection (suggestive findings: vomiting, subcutaneous emphysema) | |||||||||||||||||||||||
Assess appropriateness of patients for perfusion therapy:
❑ Contraindications to fibrinolytics (click here for the complete list shown below) | |||||||||||||||||||||||
Consider right ventricular MI in case of:
❑ Hypotension
| |||||||||||||||||||||||
Order a right sided ECG in all patients with ST elevation in leads II, III and aVF: ❑ Clearly label the ECG as right sided | |||||||||||||||||||||||
Check for hypoperfusion and left ventricular failure : ❑ Hypotension | |||||||||||||||||||||||
Begin initial treatment: ❑ Administer 162 - 325 mg of non enteric aspirin
❑ Administer 2-4 L/min oxygen via nasal cannula when saturation <90%
❑ Administer beta-blockers (unless contraindicated) and titrate to the heart rate and blood pressure
❑ Administer sublingual nitroglycerin 0.4 mg every 5 minutes for a total of 3 doses
❑ Administer 80 mg atorvastatin | |||||||||||||||||||||||
Is PCI available? | |||||||||||||||||||||||
YES | NO | ||||||||||||||||||||||
| Is first medical contact to device ≤ 120 min? | |||||||||||||||||||||||
| NO | YES | ||||||||||||||||||||||
❑ Primary PCI within 90 minutes | ❑ Fibrinolytic therapy within 30 min | ❑ Transfer for primary PCI | |||||||||||||||||||||
Confirm that the patient has one of the following indications: ❑ Symptoms of ischemia <12 hours (Class I, level of evidence A) | ❑ Confirm that the patient has one of the following indications:
❑ Confirm that the patient has no contraindications to fibrinolytics (click here for the complete list shown below) | ||||||||||||||||||||||
Administer ONE of the following antiplatelet agents (before or at the time of PCI):
Prasugrel is contraindicated in case of prior history of strokes or TIAs, active pathological bleeding, age ≥75 years, when urgent coronary artery bypass graft surgery (CABG) is likely, body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding
Administer ONE of the following anticoagulant therapy:
| Administer ONE of the following fibrinolytic therapy: ❑ Tenecteplase single IV bolus
❑ Reteplase 10 units IV boluses every 30 min
❑ Streptokinase 1.5 million units IV administered over 30-60 min Administer a P2Y12 inhibitor:
Administer ONE of the following anticoagulant therapy:
❑ Enoxaparin (for up to 8 days or until revascularization)
| ||||||||||||||||||||||
Consider urgent CABG if the coronary anatomy is not amenable to PCI and one of the following: ❑ Ongoing and recurrent ischemia | Transfer to a PCI-capable hospital for non primary PCI, if there is: ❑ Cardiogenic shock (Class I, level of evidence B) | ||||||||||||||||||||||
Contraindications to Fibrinolytic Therapy
Shown below is a table summarizing the absolute and relative contraindications to fibrinolytic therapy among STEMI patients.
| Absolute contraindications | Relative contraindications |
| ❑ Prior intracranial hemorrhage ❑ Ischemic stroke within the last 3 months (unless within 4.5 hours) |
❑ Oral anticoagulation therapy ❑ Pregnancy |
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1]
Abbreviations: CABG: coronary artery bypass graft; ECG: electrocardiogram; LAD: left anterior descending; LBBB: left bundle branch block; MI: myocardial infarction; PCI: percutaneous coronary intervention; S3: third heart sound; S4: fourth heart sound; VSD: ventricular septal defect
Characterize the symptoms: ❑ Chest pain or chest discomfort
❑ Dyspnea | |||||||||
Obtain a detailed history: ❑ Age
❑ List of medications Identify possible triggers: | |||||||||
Examine the patient: Vital signs
Pulses
Skin Heart
❑ Murmurs
❑ Pericardial friction rub (suggestive of pericarditis) Signs of right ventricular MI: Lungs | |||||||||
Pre-Discharge Care
Abbreviations: ACE: angiotensin converting enzyme; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PCI: percutaneous coronary intervention; PO: per os; STEMI: ST elevation myocardial infarction; VF: ventricular fibrillation; VT: ventricular tachycardia
Administer the following medications in patients without contraindications: ❑ Aspirin 81-325 mg (indefinitely)
❑ ACE inhibitor in case of anterior MI, ejection fraction ≤ 40% or heart failure
❑ Valsartan (in case of intolerance to ACE inhibitors)
❑ Atorvastatin 80 mg daily Administer antiplatelet therapy For patients who underwent PCI, for one year Manage complications of STEMI
❑ Temporary pacing for symptomatic bradycardia refractory to medical therapy (Class I, level of evidence C)
Assess the patient for ischemia: | |||||||||
Long Term Management
Abbreviations: ACE: angiotensin converting enzyme; ARB: angiotensin receptor blocker; MI: myocardial infarction
❑ Prepare a list of all the home medications and educate the patient about compliance
❑ Encourage lifestyle modification
❑ Ensure the initiation of the management of comorbidities
❑ Educate the patient about the early recognition of symptoms of MI | |||||||
Do's
- A pre-hospital ECG is recommended. If STEMI is diagnosed the PCI team should be activated while the patient is en route to the hospital.
- Administer reperfusion therapy for all patients presenting with STEMI within 12 hours of the beginning of the symptoms (Class I, level of evidence A).
- Administer a loading dose followed by a maintenance dose of clopidogrel, ticagrelor or prasugrel (if PCI is planned) as initial treatment instead of aspirin among patients with gastrointestinal intolerance or hypersensitivity reaction to aspirin.
- Administer sublingual nitroglycerin in patients with ischemic chest pain; however, administer IV nitroglycerin among patients with persistent chest pain after three sublingual nitroglycerins.[4]
- Discontinue non-steroidal anti-inflamatory drugs immediately.[5][6]
- Rule out any contraindications for fibrinolytic therapy before its administration. If contraindications to fibrinolytics are present, the patient should be transferred to another hospital where PCI is available.
- Initiate therapeutic hypothermia among comatose patients with STEMI (Class I, level of evidence B).
- Perform immediate angiography and PCI among STEMI patients who underwent resuscitation for cardiac arrest (Class I, level of evidence B).
- Consider bare-metal stent among STEMI patients with any of the following (Class I, level of evidence C):
- High bleeding risk
- Lack of compliance for a one year regimen of dual antiplatelet therapy
- Surgery or invasive procedure within the next year
- Achieve the following therapeutic activated clotting time when administering UFH:
- 200 to 250 seconds with the concomitant administration of GPIIbIIIa receptor inhibitor
- 250 to 300 seconds (HemoTec device) without the concomitant administration of a GPIIbIIIa receptor inhibitor
- 300 to 350 seconds (Hemochron device) without the concomitant administration of a GPIIbIIIa receptor inhibitor
- Make sure the dose of P2Y12 receptor inhibitors is appropriate among patients undergoing PCI after fibrinolytic therapy:
- Patients who already received a loading dose of clopidogrel: No loading dose, clopidogrel daily
- Patients who did not receive a loading dose of clopidogrel and PCI is performed ≤ 24 hours after fibrinolytic therapy: loading dose of 300 mg clopidogrel
- Patients who did not receive a loading dose of clopidogrel and PCI is performed > 24 hours after fibrinolytic therapy: loading dose of 600 mg clopidogrel
- Patients who did not receive a loading dose of clopidogrel and PCI is performed >24 hours after therapy with fibrin specific agent, or >48 hours after therapy with a non-fibrin-specific agent: prasugrel 60 mg
- Prepare the patient for urgent CABG when indicated by discontinuing the following:
- Clopidogrel or ticagrelor at least 24 hours prior to CABG
- Eptifibatide or tirofiban at least 2 to 4 hours prior to CABG
- Abciximab 12 hours prior to CABG
- Consider using a mechanical circulatory support among hemodynamically unstable patients with STEMI requiring an urgent CABG (Class IIa, level of evidence C).
- Recommend a long term maintenance dose of 81 mg of aspirin when the patient is administered ticagrelor.
- Include aldosterone antagonist in the discharge medication list among patients who are already on ACE inhibitors and beta-blockers with a left ventricular ejection fraction <40% or diabetes or heart failure.[1]
Don'ts
- Do not administer IV beta-blockers among patients with elevated risk for cardiogenic shock, signs of heart failure, low ouput state, prolonged PR interval more than 0.24 seconds, second or third degree block or asthma (Class I, level of evidence B).
- Do not administer IV GP IIb/IIIa inhibitors to patients with low risk of ischemic events or at high risk of bleeding and who are already on aspirin and P2Y12 receptor inhibitors therapy.
- Do not administer nitroglycerine to patients with systolic blood pressure < 90 mm Hg or ≥ to 30 mm Hg below baseline, severe bradycardia (< 50 bpm), tachycardia (> 100 bpm), or suspected right ventricular myocardial infarction.
- Do not delay the time for reperfusion.
- Do not administer prasugrel among patients with any of the following:
- Prior history of strokes or TIAs (Class III, Level of evidence B)
- Active pathological bleeding
- Age ≥75 years of age, (except in high-risk patients such as diabetes or prior MI, where its use may be considered)
- Urgent coronary artery bypass graft surgery (CABG) is likely
- Presence of additional risk factors for bleeding such as body weight <60 kg, propensity to bleed, concomitant use of medications that increase the risk of bleeding[7]
- Do not administer fibrinolytic therapy to patients with known history of intracranial hemorrhage, cerebral arteriovenous malformation or to patients with suspected aortic dissection.
- Do not withhold aspirin among patients who are planned to undergo urgent CABG (Class I, level of evidence C).[1]
Gallery
Shown below is an EKG demonstrating the evolution of an infarct on the EKG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave suggest STEMI.
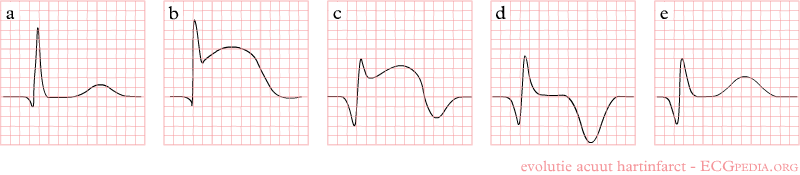
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:AMI_evolutie.png
Shown below is an EKG demonstrating loss of R waves throughout the anterior wall (V1-V6). QS complexes in V3-V5. ST elevation in V1-V5 with terminal negative T waves.
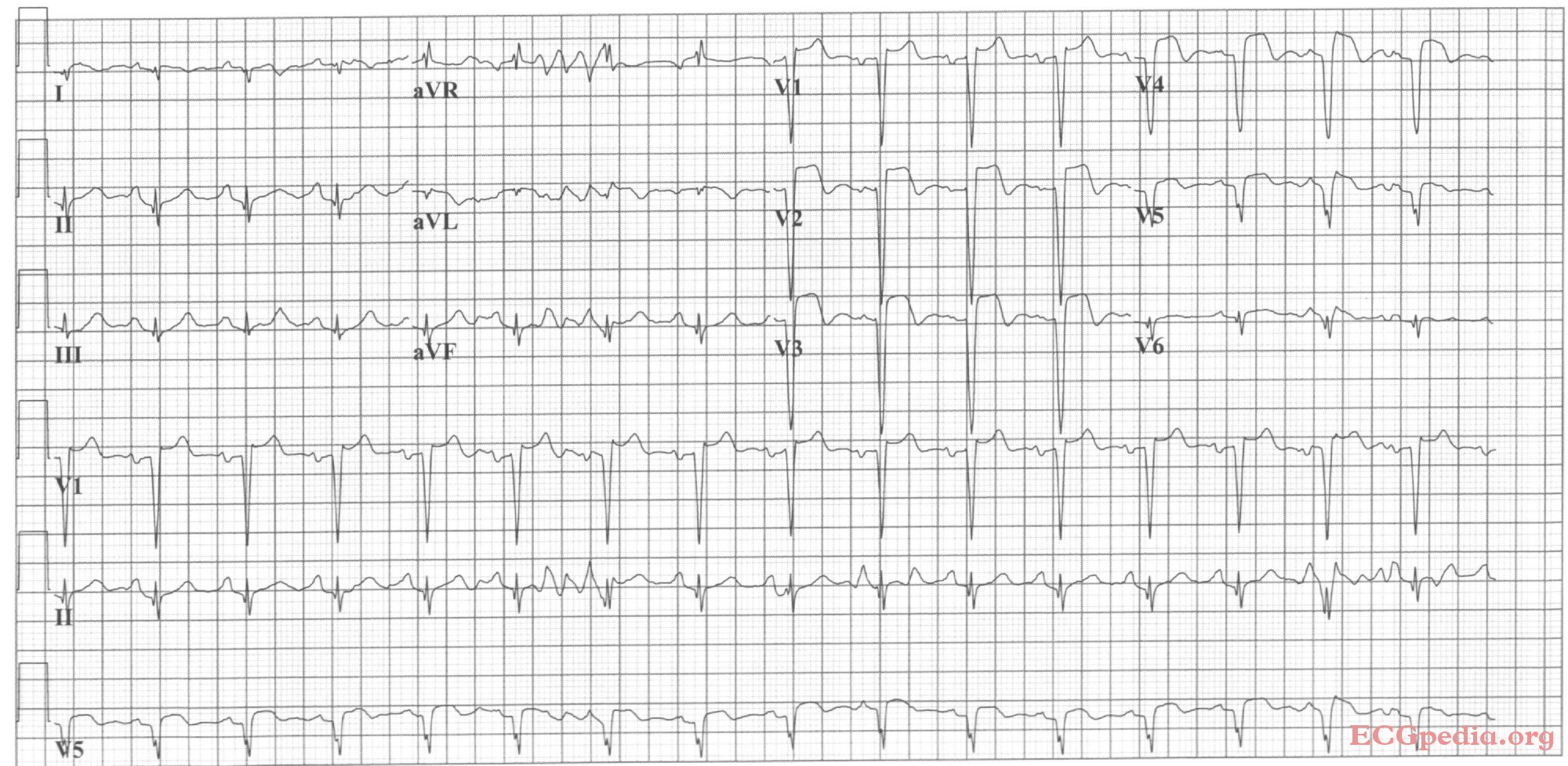
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating ST elevation in leads II, III and aVF and ST depression in leads V1, V2 and V3 depicting a posterior MI.
Shown below is an EKG demonstrating acute MI in a patient with LBBB
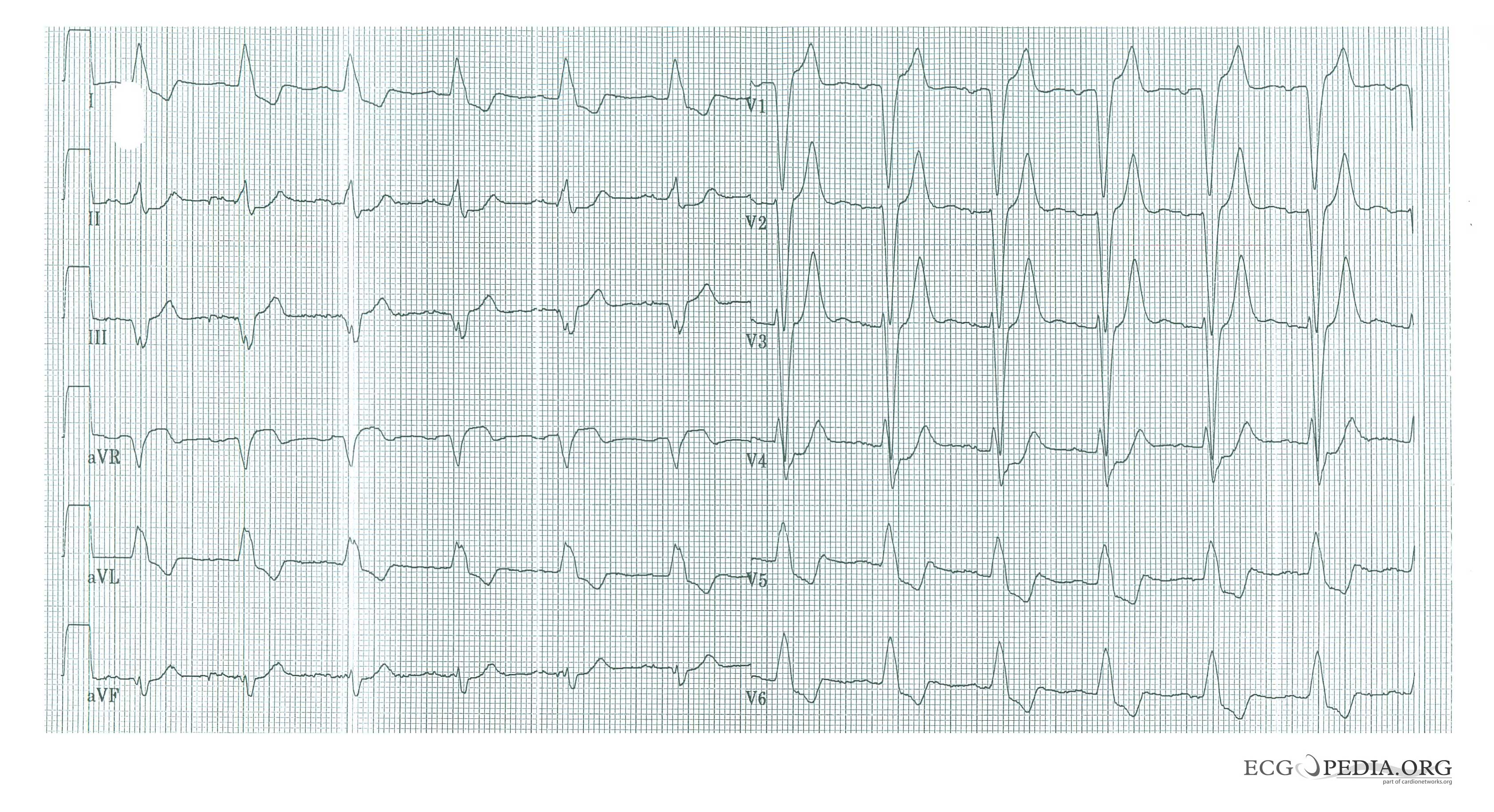
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
References
- ↑ 1.0 1.1 1.2 1.3 O'Gara, Patrick T.; Kushner, Frederick G.; Ascheim, Deborah D.; Casey, Donald E.; Chung, Mina K.; de Lemos, James A.; Ettinger, Steven M.; Fang, James C.; Fesmire, Francis M.; Franklin, Barry A.; Granger, Christopher B.; Krumholz, Harlan M.; Linderbaum, Jane A.; Morrow, David A.; Newby, L. Kristin; Ornato, Joseph P.; Ou, Narith; Radford, Martha J.; Tamis-Holland, Jacqueline E.; Tommaso, Carl L.; Tracy, Cynthia M.; Woo, Y. Joseph; Zhao, David X. (2013). "2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction". Journal of the American College of Cardiology. 61 (4): e78–e140. doi:10.1016/j.jacc.2012.11.019. ISSN 0735-1097.
- ↑ Wang-Clow F, Fox NL, Cannon CP, Gibson CM, Berioli S, Bluhmki E; et al. (2001). "Determination of a weight-adjusted dose of TNK-tissue plasminogen activator". Am Heart J. 141 (1): 33–40. doi:10.1067/mhj.2001.112092. PMID 11136484.
- ↑ Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS; et al. (2008). "ACC/AHA/HRS 2008 guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: executive summary". Heart Rhythm. 5 (6): 934–55. doi:10.1016/j.hrthm.2008.04.015. PMID 18534377.
- ↑ Kaplan K, Davison R, Parker M, Przybylek J, Teagarden JR, Lesch M (1983). "Intravenous nitroglycerin for the treatment of angina at rest unresponsive to standard nitrate therapy". Am J Cardiol. 51 (5): 694–8. PMID 6402912.
- ↑ Trelle S, Reichenbach S, Wandel S, Hildebrand P, Tschannen B, Villiger PM; et al. (2011). "Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis". BMJ. 342: c7086. doi:10.1136/bmj.c7086. PMC 3019238. PMID 21224324. Review in: Evid Based Med. 2011 Oct;16(5):142-3
- ↑ Coxib and traditional NSAID Trialists' (CNT) Collaboration. Bhala N, Emberson J, Merhi A, Abramson S, Arber N; et al. (2013). "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". Lancet. 382 (9894): 769–79. doi:10.1016/S0140-6736(13)60900-9. PMC 3778977. PMID 23726390. Review in: Ann Intern Med. 2013 Oct 15;159(8):JC12
- ↑ "http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=5fe9c118-c44b-48d7-a142-9668ae3df0c6". Retrieved 6 February 2014. External link in
|title=(help)