Tipranavir clinical studies
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Zaghw, M.D. [2]
Clinical Studies
Adult Patients
The following clinical data is derived from analyses of 48-week data from ongoing studies measuring effects on plasma HIV-1 RNA levels and CD4+ cell counts. At present there are no results from controlled studies evaluating the effect of APTIVUS/ritonavir on clinical progression of HIV-1.
APTIVUS/ritonavir 500/200 mg BID + optimized background regimen (OBR) vs. Comparator Protease Inhibitor/ritonavir BID + OBR The two clinical trials 1182.12 and 1182.48 (RESIST 1 and RESIST 2) are ongoing, randomized, controlled, open-label, multicenter studies in HIV-1 positive, triple antiretroviral class experienced patients. All patients were required to have previously received at least two protease inhibitor-based antiretroviral regimens and were failing a protease inhibitor-based regimen at the time of study entry with baseline HIV-1 RNA at least 1000 copies/mL and any CD4+ cell count. At least one primary protease gene mutation from among 30N, 46I, 46L, 48V, 50V, 82A, 82F, 82L, 82T, 84V or 90M had to be present at baseline, with not more than two mutations at codons 33, 82, 84 or 90.
These studies evaluated treatment response at 48 weeks in a total of 1483 patients receiving either APTIVUS co-administered with 200 mg of ritonavir plus OBR versus a control group receiving a ritonavir-boosted protease inhibitor (lopinavir, amprenavir, saquinavir or indinavir) plus OBR. Prior to randomization, OBR was individually defined for each patient based on genotypic resistance testing and patient history. The investigator had to declare OBR, comparator protease inhibitor, and use of new enfuvirtide prior to randomization. Randomization was stratified by choice of comparator protease inhibitor and use of new enfuvirtide.
After Week 8, patients in the control group who met the protocol defined criteria of initial lack of virologic response or confirmed virologic failure had the option of discontinuing treatment and switching to APTIVUS/ritonavir in a separate roll-over study.
Demographics and baseline characteristics were balanced between the APTIVUS/ritonavir arm and control arm. In both studies combined, the 1483 patients had a median age of 43 years (range 17-80), and were 86.3% male, 75.6% white, 12.9% black, and 0.9% Asian. The median baseline plasma HIV-1 RNA for both treatment groups was 4.8 (range 2.0 to 6.8) log10 copies/mL and median baseline CD4+ cell count was 162 (range 1 to 1894) cells/mm3. Overall, 38.4% of patients had a baseline HIV-1 RNA of >100,000 copies/mL, 58.6% had a baseline CD4+ cell count ≤200 cells/mm3, and 57.8% had experienced an AIDS defining Class C event at baseline.
Patients had prior exposure to a median of 6 NRTIs, 1 NNRTI, and 4 PIs. A total of 10.1% of patients had previously used enfuvirtide. In baseline patient samples (n=454), 97% of the HIV-1 isolates were resistant to at least one protease inhibitor, 95% of the isolates were resistant to at least one NRTI, and >75% of the isolates were resistant to at least one NNRTI.
The individually pre-selected protease inhibitor based on genotypic testing and the patient’s medical history was lopinavir in 48.7%, amprenavir in 26.4%, saquinavir in 21.8% and indinavir in 3.1% of patients. A total of 85.1% were possibly resistant or resistant to the pre-selected comparator protease inhibitors. Approximately 21% of patients used enfuvirtide during the study of which 16.6% in the APTIVUS/ritonavir arm and 13.2% in the comparator/ritonavir arm represented first time use of enfuvirtide (new enfuvirtide).
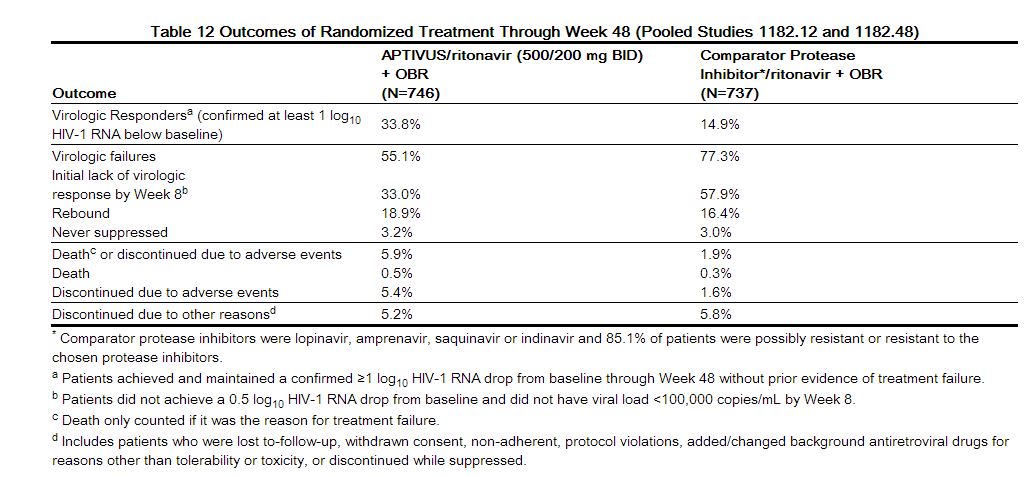
Treatment response and efficacy outcomes of randomized treatment through Week 48 of studies 1182.12 and 1182.48 are shown in Table 12.
|
Through 48 weeks of treatment, the proportion of patients in the APTIVUS/ritonavir arm compared to the comparator PI/ritonavir arm with HIV-1 RNA <400 copies/mL was 30.3% and 13.6% respectively, and with HIV-1 RNA <50 copies/mL was 22.7% and 10.2% respectively. Among all randomized and treated patients, the median change from baseline in HIV-1 RNA at the last measurement up to Week 48 was -0.64 log10 copies/mL in patients receiving APTIVUS/ritonavir versus -0.22 log10 copies/mL in the comparator PI/ritonavir arm.
Among all randomized and treated patients, the median change from baseline in CD4+ cell count at the last measurement up to Week 48 was +23 cells/mm3 in patients receiving APTIVUS/ritonavir (N=740) versus +4 cells/mm3 in the comparator PI/ritonavir (N=727) arm.
Patients in the APTIVUS/ritonavir arm achieved a significantly better virologic outcome when APTIVUS/ritonavir was combined with enfuvirtide. Among patients with new enfuvirtide use, the proportion of patients in the APTIVUS/ritonavir arm compared to the comparator PI/ritonavir arm with HIV-1 RNA <400 copies/mL was 52.4% and 19.6% respectively, and with HIV-1 RNA <50 copies/mL was 37.3% and 14.4% respectively [see Clinical Pharmacology (12.2, 12.4)]. The median change from baseline in CD4+ cell count at the last measurement up to Week 48 was +89 cells/mm3 in patients receiving APTIVUS/ritonavir in combination with newly introduced enfuvirtide (N=124) and +18 cells/mm3 in the comparator PI/ritonavir (N=96) arm.
Pediatric Patients
The pharmacokinetic profile, safety and activity of APTIVUS/ritonavir was evaluated in a randomized, open-label, multicenter study. This study enrolled HIV-1 infected, treatment-experienced pediatric patients (with the exception of 3 treatment-naïve patients), with baseline HIV-1 RNA of at least 1500 copies/mL. The age ranged from 2 through 18 years and patients were stratified by age (2 to <6 years, 6 to <12 years and 12 to 18 years). One hundred and ten (110) patients were randomized to receive one of two APTIVUS/ritonavir dose regimens: 375 mg/m2/150 mg/m2 dose (N=55) or 290 mg/m2/115 mg/m2 dose (N=55), plus background therapy of at least two non-protease inhibitor antiretroviral drugs, optimized using baseline genotypic resistance testing. All patients initially received APTIVUS oral solution. Pediatric patients who were 12 years or older and received the maximum dose of 500/200 mg BID could subsequently change to APTIVUS capsules at day 28 [see Adverse Reactions (6.2), Use in Specific Populations (8.4), Clinical Pharmacology(12.3), and Microbiology (12.4)].
Demographics and baseline characteristics were balanced between the APTIVUS/ritonavir dose groups. The 110 randomized pediatric patients had a median age of 11.7 years (range 2 to 18), and were 57.2% male, 68.1% white, 30% black, and 1.8% Asian. The median baseline plasma HIV-1 RNA was 4.7 (range 3.0 to 6.8) log10 copies/mL and median baseline CD4+ cell count was 379 (range 2 to 2578) cells/mm3. Overall, 37.4% of patients had a baseline HIV-1 RNA of >100,000 copies/mL; 28.7% had a baseline CD4+ cell count ≤200 cells/mm3, and 48% had experienced a prior AIDS defining Class C event at baseline. Patients had prior exposure to a median of 4 NRTIs, 1 NNRTI, and 2 PIs.
Eighty three (75%) completed the 48 week period while 25% discontinued prematurely. Of the patients who discontinued prematurely, 9 (8%) discontinued due to virologic failure, and 9 (8%) discontinued due to adverse reactions.
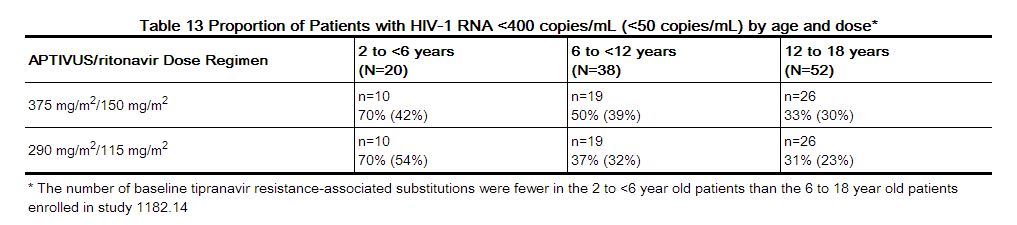
At 48 weeks, 40% of patients had viral load <400 copies/mL. The proportion of patients with viral load <400 copies/mL tended to be greater (70%) in the youngest group of patients, who had less baseline viral resistance, compared to the older groups (37% and 31%). The HIV-1 RNA results are presented in Table 13.
|
The dose selection for all age groups was based on the following:
A greater proportion of patients receiving APTIVUS/ritonavir 375 mg/m2/150 mg/m2 compared to 290 mg/m2/115 mg/m2 achieved HIV-1 RNA <400 and <50 copies/mL. A greater proportion of patients 6 to 18 years of age with multiple baseline protease inhibitor resistance-associated substitutions receiving APTIVUS/ritonavir 375 mg/m2/150 mg/m2 achieved HIV-1 RNA <400 copies/mL at 48 weeks compared to patients receiving APTIVUS/ritonavir 290 mg/m2/115 mg/m2. No clinically significant increase in adverse event rates observed with 375 mg/m2/150 mg/m2 compared to 290 mg/m2/115 mg/m2. Overall, 6 (5%) patients ages 6 to 18 had AIDS defining illness during the treatment period and all received the 290 mg/m2/115 mg/m2 dose.
The guidance for possible dose reduction for patients who develop intolerance or toxicity and cannot continue with APTIVUS/ritonavir 14 mg/kg/6 mg/kg (or 375 mg/m2/150 mg/m2) is based on the following:
The 290 mg/m2/115 mg/m2 twice daily regimen provided tipranavir plasma concentrations similar to those obtained in adults receiving 500/200 mg twice daily. The 375 mg/m2/150 mg/m2 twice daily regimen provided tipranavir plasma concentrations 37% higher than those obtained in adults receiving 500/200 mg twice daily. The observed response rates for APTIVUS/ritonavir dose of 290 mg/m2/115 mg/m2 as shown in Table 13.
Dose reduction is not appropriate for patients whose virus is resistant to more than one protease inhibitor.
When body surface area (BSA) dosing is converted to mg/kg dosing, the APTIVUS/ritonavir 375 mg/m2/150 mg/m2 twice daily regimen is similar to 14 mg/kg/6 mg/kg and APTIVUS/ritonavir 290 mg/m2/115 mg/m2 twice daily regimen is similar to 12 mg/kg/5 mg/kg twice daily.[1]
References
Adapted from the FDA Package Insert.