Tracheal intubation: Difference between revisions
m (Intubation moved to Tracheal intubation over redirect: Article title should be the recognised medical name rather than a lay term) |
No edit summary |
||
| Line 2: | Line 2: | ||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} | ||
{{EH}} | |||
{{Interventions infobox | | |||
Name = {{PAGENAME}} | | |||
Image = Intubation.jpg | | |||
Caption = [[Tracheal intubation]] being practiced on a [[mannequin]] (orotracheal technique using a [[laryngoscope]]. | | |||
ICD10 = | | |||
ICD9 = 96.04 | | |||
MeshID = D007442 | | |||
OtherCodes = | | |||
}} | |||
'''Tracheal intubation''' (often simply referred to as '''intubation''') is the placement of a flexible plastic tube into the [[vertebrate trachea|trachea]] to protect the airway and provide a means of [[mechanical ventilation]]. The most common route for tracheal intubation is '''orotracheal''' where, with the assistance of a [[laryngoscope]], an [[endotracheal tube]] is passed through the [[oropharynx]], [[glottis]], and [[larynx]] into the trachea. A bulb is then inflated near the distal tip of the tube to help secure it in place and protect the airway from blood, gastric contents and other [[secretion]]s. Another route for tracheal intubation is '''nasotracheal''', where an endotracheal tube is passed through the [[nasopharynx]], glottis, and larynx into the trachea. Removal of the tube is referred to as '''extubation''' of the trachea. | |||
==History== | |||
===Pre-19th century=== | |||
The first known description of tracheal intubation was given in the 1020s by [[Avicenna]] in ''[[The Canon of Medicine]]'' in order to facilitate [[breathing]].<ref name=>{{cite book | |||
|author=Patricia Skinner | |||
|title=The Gale Encyclopedia of Alternative Medicine | |||
|editor=Laurie J. Fundukian | |||
|chapter=Unani-tibbi | |||
|publisher=[http://www.gale.com [[Gale (publisher)|Gale Cengage]]] | |||
|location=[[Farmington Hills, Michigan]] | |||
|edition=3rd | |||
|date=2008 | |||
|pages= | |||
|isbn=9781414448725 | |||
|url=http://findarticles.com/p/articles/mi_g2603/is_0007/ai_2603000716/ | |||
|accessdate=17 July 2010}}</ref> The next known report on tracheal intubation and subsequent [[artificial respiration]] of animals was in 1543, when [[Andreas Vesalius]] pointed out that the technique could be life-saving.{{Citation needed|date=July 2010}} This report remained unnoticed for more than 250 years. | |||
{{ | ===19th century=== | ||
In 1805, [[Philip Bozzini]] used a device he invented and called the ''lichtleiter'' (or light-guiding instrument) to examine the human [[urinary bladder]], [[rectum]] and [[Human pharynx|pharynx]].{{Citation needed|date=July 2010}} The practice of gastric [[endoscopy]] in humans was pioneered by [[U.S. Army]] [[surgeon]] [[William Beaumont]] in 1822 with the cooperation of his patient [[Alexis St. Martin]], a victim of an accidental gunshot wound to the [[stomach]].<ref name=>{{cite book | |||
|author=[[William Beaumont]] and [[Andrew Combe]] | |||
|title=Experiments and observations on the gastric juice, and the physiology of digestion | |||
|editor= | |||
|chapter= | |||
|publisher=MacLachlan & Stewart | |||
|location=Edinburgh | |||
|edition= | |||
|date=1838 | |||
|pages=319 | |||
|isbn= | |||
|url=http://books.google.com/books?id=H6F4_9joRkgC&printsec=frontcover&dq=%22experiments+and+observations+on+the+gastric+juice+and+the+physiology+of+digestion%22&source=bl&ots=niFAhg5rg-&sig=CtwyPCZke7Y8DDZbPw9Dz7bdr8I&hl=en&ei=mak7TPrNE4P6lwew3839BQ&sa=X&oi=book_result&ct=result&resnum=1&ved=0CBIQ6AEwAA#v=onepage&q&f=false | |||
|accessdate=12 July 2010}}</ref> In 1853, [[Antoine Jean Desormeaux]] of France examined the human bladder using a device he invented and called the ''[[Endoscopy|endoscope]]'' (this was the first time this term was applied to this practice).{{Citation needed|date=July 2010}} In 1868, [[Adolph Kussmaul]] of Germany performed the first [[esophagogastroduodenoscopy]] on a living human. The subject was a [[Sword swallowing|sword-swallower]], who swallowed a metal tube with a length of 47 centimeters and a diameter of 13 millimeters.{{Citation needed|date=July 2010}} In 1869, the German surgeon [[Friedrich Trendelenburg]] documented successful human [[tracheotomy]] for administration of [[General anaesthesia|general anesthesia]].{{Citation needed|date=July 2010}} In 1878, the Scottish surgeon [[William Macewen]] performed the first orotracheal intubation.{{Citation needed|date=July 2010}} In 1878, [[Maximilian Nitze]] and Josef Leiter invented the [[Cystoscopy|cystourethroscope]]{{Citation needed|date=July 2010}} and in 1881, [[Jan Mikulicz-Radecki]] created the first rigid gastroscope for practical applications.{{Citation needed|date=July 2010}} On 23 April 1895, [[Alfred Kirstein]] performed the first direct laryngoscopy in Berlin, Germany, using an esophagoscope he had modified for this purpose.<ref name=Hirsch1986>{{cite journal | |||
|author=N.P. Hirsch, G.B. Smith, and P.O. Hirsch | |||
|title=Alfred Kirstein: Pioneer of direct laryngoscopy | |||
|journal=Anaesthesia | |||
|volume=41 | |||
|issue=1 | |||
|pages=42-45 | |||
|date=January 1986 | |||
|doi=10.1111/j.1365-2044.1986.tb12702.x | |||
|url=http://www3.interscience.wiley.com/journal/119485967/abstract?CRETRY=1&SRETRY=0 | |||
|accessdate=10 July 2010}}</ref> | |||
===20th century=== | |||
The 20th century saw the transformation of endoscopy and tracheal intubation from a rarely employed procedure to one which has become essential to the practices of [[anesthesia]], [[Intensive-care medicine|critical care medicine]], [[emergency medicine]], [[gastroenterology]], [[pulmonology]], and [[surgery]]. During [[World War I]], Sir [[Ivan Magill]] and [[Robert Reynolds Macintosh|Robert Macintosh]] achieved significant advances in techniques for tracheal intubation.{{Citation needed|date=July 2010}} The Magill curve of an endotracheal tube and the Magill forceps for positioning the tube during nasotracheal intubation are named after Magill, while the most widely used curved laryngoscope blade is named after Macintosh. In 1932, [[Rudolf Schindler (doctor)|Rudolph Schindler]] of Germany introduced the first semi-flexible gastroscope.{{Citation needed|date=July 2010}} This device had numerous [[Lens (optics)|lenses]] positioned throughout the tube and a miniature light bulb at the distal tip. The tube of this device was 75 centimeters in length and 11 millimeters in diameter, and the distal portion was capable of a certain degree of flexion. Between 1945 and 1952, [[Optical engineering|optical engineers]] (notably [[Karl Storz]] of Germany, [[Harold Hopkins]] of England, and [[Mutsuo Sugiura]] of the Japanese [[Olympus Corporation]]) built upon this early work, leading to the development of the first [[gastrocamera]].{{Citation needed|date=July 2010}} In 1964, [[Fernando Alves Martins]] of Portugal applied [[optical fiber]] technology to one of these early gastrocameras to produce the first gastrocamera with a flexible [[fiberscope]].{{Citation needed|date=July 2010}} Initially used in esophagogastroduodenoscopy, newer devices were developed in the early 1970s for use in [[bronchoscopy]], [[rhinoscope|rhinoscopy]], and laryngoscopy. By the mid-1980s, the flexible fiberoptic bronchoscope had become an indispensable instrument within the pulmonology and anesthesia communities. | |||
== | ===21st century=== | ||
The [[Information Age|Digital Revolution]] has brought newer technology to the art and science of tracheal intubation. Several manufacturers have developed [[video laryngoscope]]s which employ [[Digital electronics|digital technology]] such as the [[CMOS]] [[active pixel sensor]] (CMOS APS) to generate a view of the glottis so that the trachea may be intubated. The Glidescope video laryngoscope is one example of such a device.{{Citation needed|date=July 2010}} | |||
==Indications== | |||
A definitive airway (orotracheal, nasotracheal, [[cricothyrotomy]], or tracheotomy) is indicated under any of the following circumstances: | |||
* [[Coma]]tose or [[Intoxication|intoxicated]] patients with a [[altered level of consciousness|depressed level of consciousness]] who are unable to protect their airways. This is commonly defined as those subjects with a [[Glasgow Coma Scale]] ≤ 8. In such cases, the throat muscles may lose their tone so that the [[hypopharynx]] becomes obstructed, impeding the free flow of air into the lungs. Furthermore, protective airway reflexes such as [[cough]]ing and [[swallowing]], which serve to protect the airways against [[Pulmonary aspiration|aspiration]] of [[secretion]]s and [[Foreign body|foreign bodies]], may be absent. With tracheal intubation, airway patency is restored and the lower airways can be protected from aspiration. | |||
* Requirement for mechanical ventilation, including [[cardiopulmonary resuscitation]] and general anesthesia. In such situations, spontaneous [[Ventilation (physiology)|ventilation]] may be decreased or absent due to the effect of [[injury]], [[disease]], [[anesthetic]] agents, [[opioid]]s, or [[neuromuscular-blocking drug]]s. To enable mechanical ventilation, an endotracheal tube is often used, although there are alternative devices such as the [[laryngeal mask airway]] or the [[Positive airway pressure|CPAP mask]]. | |||
* [[Apnea]] or [[hypoventilation]] (e.g., [[closed head injury]], intoxication or [[poisoning]], [[Spinal cord injury|cervical spine injury]], [[flail chest]]) | |||
* Persistent or recurrent airway obstruction | |||
* Impending or potential compromise of the airway (e.g., sustained [[Epileptic seizure|seizure activity]], [[Facial trauma|facial fractures]], expanding neck [[hematoma]], laryngeal or [[Tracheobronchial injury|tracheobronchial]] injury, airway burns, [[smoke inhalation|inhalation injury]]) | |||
* Inability to maintain [[Oxygenation (medical)|oxygenation]] using [[Simple face mask|face mask]] [[Oxygen therapy|oxygen supplementation]] (severe [[pneumonia]], [[acute respiratory distress syndrome]] (ARDS), near-[[drowning]], etc.) | |||
* Diagnostic or therapeutic manipulation of the airway (such as [[bronchoscopy]], [[Laser medicine|laser therapy]] or [[stent]]ing of the [[Bronchus|bronchi]]). | |||
==Equipment== | |||
===Laryngoscopes=== | |||
The vast majority of "noninvasive" tracheal intubations involve the use of a [[viewing instrument]] or "scope" of one type or another. Since its introduction by Kirstein in 1895, the most common device used for this purpose has been the conventional laryngoscope. Today, the typical conventional laryngoscope consists of a handle, usually containing batteries, and a set of interchangeable blades. Two basic styles of laryngoscope blade are commercially available: the straight blade and the curved blade. The [[Robert Reynolds Macintosh|Macintosh]] blade is the most widely used of the curved laryngoscope blades, while the Miller blade is the most popular style of straight blade. There are many other styles of straight and curved blades, with accessories such as mirrors for enlarging the field of view and even ports for the administration of [[oxygen]]. These specialty blades are primarily designed for use by [[Anesthesiologist|anesthetist]]s, most commonly in the [[Operating theater|operating room]]. | |||
== | Besides the conventional laryngoscopes, many devices have been developed as alternatives to direct laryngoscopy. These include a number of indirect [[Optical fiber|fiberoptic]] viewing laryngoscopes such as the [[fiberscope|flexible fiberoptic bronchoscope]], Bullard scope, UpsherScope,<ref name=>{{cite journal | ||
|author=Peter Fridrich, Michael Frass, Claus G. Krenn, Christian Weinstabl, Jonathan L. Benumof, and Peter Krafft | |||
|title=The UpsherScope in routine and difficult airway management: a randomized, controlled clinical trial | |||
|journal=Anesth Analg. | |||
|volume=85 | |||
|issue=6 | |||
|pages=1377-1381 | |||
|date=December 1997 | |||
|doi=10.1097/00000539-199712000-00036 | |||
|pmid=9390612 | |||
|url=http://www.anesthesia-analgesia.org/cgi/pmidlookup?view=long&pmid=9390612 | |||
|accessdate=17 July 2010}}</ref> and the WuScope. These devices are widely employed for tracheal intubation, especially in the setting of the difficult intubation (see below). Several types of video laryngoscopes are also currently available (e.g., Glidescope, McGrath laryngoscope, Daiken Medical Coopdech C-scope vlp-100, the Storz C-Mac, Pentax AWS and the Berci DCI). Other noninvasive devices which are commonly employed for tracheal intubation are the laryngeal mask airway (used as a guide for tracheal tube placement), the lighted stylet, and the AirTraq. Due to the widespread availability of such devices, the technique of blind digital intubation of the trachea is rarely practiced today, though it may still be useful in emergency situations under austere conditions such as natural or man-made [[disaster]]s. | |||
===Stylets=== | |||
A stylet is a [[Ductility|malleable]] metal [[wire]] which can be inserted into the endotracheal tube to make the tube conform better to the laryngopharyngeal anatomy of the specific individual, thus facilitating its insertion. It is commonly employed under circumstances of difficult laryngoscopy. The [[Eschmann stylet]] or ''[[Natural rubber|gum elastic]] bougie'' is a specialized type of stylet, which can also be used for difficult laryngoscopy or for removal and replacement of tracheal tubes without the need for laryngoscopy. | |||
== | ===Tracheal tubes=== | ||
[[File:Carlens.jpg|300px|thumb|right|A Carlens double-lumen [[endotracheal tube]], commonly used for [[thoracic surgery|thoracic surgical]] operations such as [[VATS lobectomy]].]] | |||
Most tracheal tubes today are constructed of [[polyvinyl chloride]], but specialty tubes constructed of [[silicone rubber]], [[Natural rubber|latex rubber]], or [[stainless steel]] are also widely available. Most tubes have an inflatable cuff to seal the trachea and [[Bronchus|bronchial tree]] against air leakage and [[Pulmonary aspiration|aspiration of gastric contents]], blood, secretions, and other fluids. Uncuffed tubes are also available, though their use is limited mostly to pediatric patients (in small children, the cricoid cartilage, the narrowest portion of the pediatric airway, often provides an adequate seal for mechanical ventilation). | |||
===Observational methods to confirm | The "armored endotracheal tube" is a cuffed, wire-reinforced, silicone rubber tube which is quite flexible but yet difficult to compress or kink. This can make it useful for situations in which the trachea is anticipated to remain intubated for a prolonged duration, or if the neck is to remain flexed during surgery. Polyvinyl chloride tubes are relatively stiff in comparison. Preformed tubes (such as the oral and nasal RAE tubes, named after the inventors Ring, Adair and Elwyn) are also widely available for special applications. These may also be constructed of polyvinyl chloride or wire-reinforced silicone rubber. Other tubes (such as the Bivona® Fome-Cuf® tube) are designed specifcally for use in laser surgery in and around the airway. Various types of double-lumen endotracheal tubes have been developed (Carlens, Robertshaw, etc.) for ventilating each lung independently—this is useful during pulmonary and other thoracic operations. | ||
===Observational methods to confirm tube placement=== | |||
*Direct visualization of the tube passing through the [[vocal cords]] | *Direct visualization of the tube passing through the [[vocal cords]] | ||
*Clear and equal bilateral [[breath sounds]] on auscultation of the chest | *Clear and equal bilateral [[breath sounds]] on auscultation of the chest | ||
*Absent sounds on auscultation of the [[epigastrium]] | *Absent sounds on auscultation of the [[epigastrium]] | ||
*Equal bilateral chest rise with [[ | *Equal bilateral chest rise with [[ventilation]] | ||
*Fogging of the tube | *Fogging of the tube | ||
*An absence of stomach contents in the tube | *An absence of stomach contents in the tube | ||
===Instruments to confirm | ===Instruments to confirm tube placement=== | ||
*Colorimetric end tidal | No single method for confirming tracheal tube placement has been shown to be 100% reliable. Accordingly, the use of multiple methods to confirm correct tube placement is now widely considered to be the [[standard of care]]. At least one of the methods utilized should be an instrument. Waveform '''[[capnography]]''' has emerged as the [[gold standard (test)|gold standard]] for the confirmation of correct tube placement and maintenance of the tube once it is in place. Other methods include: | ||
* [[Colorimetry|Colorimetric]] end tidal [[carbon dioxide]] detector | |||
*Self inflating esophageal bulb | * Self-inflating esophageal bulb | ||
*[[Pulse oximetry]] ( | * [[Pulse oximetry]] (important limitations include a significant delay in the decrease in [[oxygen saturation]], especially if subject has been pre-oxygenated) | ||
* Esophageal Detection Device<ref name=>{{cite web | |||
|author=Tim Wolfe, M.D. | |||
|date=May 1998 | |||
|url=http://www.wolfetory.com/education/eddab.html | |||
|title=The Esophageal Detector Device: Summary of the current articles in the literature | |||
|publisher=[http://www.wolfetory.com/ Wolfe Tory Medical, Inc.] | |||
|location=Salt Lake City, Utah | |||
|accessdate=17 July 2010}}</ref> | |||
== | ==Predicting ease of intubation== | ||
*Look externally (history of craniofacial traumas/previous surgery) | |||
*Evaluate 3,3,2 - three of the subject's fingers should be able to fit into his/her mouth when open, three fingers should comfortably fit between the chin and the throat, and two fingers in the thyromental distance (distance from thyroid cartilage to chin) | |||
*[[Mallampati score]] | |||
*Obstructions (stridorous breath sounds, wheezing, etc.) | |||
*Neck mobility (can subject tilt head back and then forward to touch chest) | |||
*Cormack-Lehane grading system (according to the percentage of glottic opening on laryngoscopy) | |||
== | ==Tracheal tube maintenance== | ||
The tube is secured in place with tape or an endotracheal tube holder. A cervical collar is sometimes used to prevent motion of the airway. Tube placement should be confirmed after each physical move of the patient and after any unexplained change in his/her clinical status. Continuous pulse oximetry and continuous waveform capnography are often used to monitor the tube's correct placement. | |||
== | The cuff pressure must be monitored carefully in order to avoid complications from over-inflation, which can include [[tracheomalacia]], [[tracheoesophageal fistula]], or even frank rupture of the trachea. Many of the complications of over-inflated cuffs can be traced to excessive cuff pressure causing ischemia of the tracheal mucosa.<ref name=>{{cite journal | ||
|author=Papiya Sengupta, Daniel I Sessler, Paul Maglinger, Spencer Wells, Alicia Vogt, Jaleel Durrani, and Anupama Wadhwa | |||
|title=Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure | |||
|journal=BMC Anesthesiology | |||
|volume=4 | |||
|issue=1 | |||
|pages=8 | |||
|date=2004 | |||
|doi=10.1186/1471-2253-4-8 | |||
|pmid=15569386 | |||
|PMCID=PMC535565 | |||
|url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC535565/?tool=pmcentrez | |||
|accessdate=17 July 2010}}</ref> | |||
An excessive leak can sometimes be corrected through the placement of a larger (0.5 mm larger in internal diameter) endotracheal tube, and in difficult-to-ventilate pediatric patients children it is often necessary to use cuffed tubes to allow for high pressure ventilation if the leak is too great to overcome with the ventilator.<ref name=>{{cite journal | |||
|author=Sheridan RL | |||
|title=Uncuffed endotracheal tubes should not be used in seriously burned children | |||
|journal=Pediatr Crit Care Med | |||
|volume=7 | |||
|issue=3 | |||
|pages=258-259 | |||
|date=May 2006 | |||
|doi=10.1097/01.PCC.0000216681.71594.04 | |||
|pmid=16575345 | |||
|url=http://journals.lww.com/pccmjournal/Abstract/2006/05000/Uncuffed_endotracheal_tubes_should_not_be_used_in.13.aspx | |||
|accessdate=17 July 2010}}</ref> | |||
==Special situations== | |||
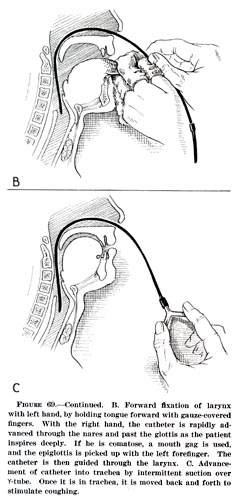
[[Image:Chapter5figure69b-nasotracheal intubation.jpg|thumb|right|200px|Nasal intubation]] | |||
== | ===Emergency intubation=== | ||
Personnel experienced in direct laryngoscopy are not always immediately available in certain settings that require emergency tracheal intubation. For this reason, specialized devices have been designed to act as bridges to a definitive airway. Such devices include the laryngeal mask airway, cuffed oropharyngeal airway, and the [[Combitube]].<ref name=Foley2000>{{cite journal | |||
|author=Foley LJ, Ochroch EA | |||
|title=Bridges to establish an emergency airway and alternate intubating techniques | |||
|journal=Critical Care Clinics | |||
|volume=16 | |||
|issue=3 | |||
|pages=429-444 | |||
|date=July 2000 | |||
|doi=10.1016/S0749-0704%2805%2970121-4 | |||
|pmid=10941582 | |||
|url=http://www.ncbi.nlm.nih.gov/pubmed/10941582 | |||
|accessdate=16 July 2010}}</ref> Other devices such as rigid stylets, the lightwand (a blind technique) and indirect fiberoptic rigid stylets, such as the Bullard scope, Upsher scope, and the WuScope can also be used as alternatives to direct laryngoscopy. Each of these devices have its own unique set of benefits and drawbacks, and none of them is effective under all circumstances. | |||
[[ | ===Difficult intubation=== | ||
Many individuals have unusual airway anatomy, such as those who have limited range of motion of the [[Cervical vertebrae|cervical spine]] or [[temporomandibular joint]], or who have oropharyngeal [[tumor]]s, [[hematoma]]s, [[angioedema]], [[Micrognathism|micrognathia]], [[Retrognathism|retrognathia]], or excess [[adipose tissue]] of the face and neck. Using conventional laryngoscopic techniques, intubation of the trachea can be difficult in such people. Use of the flexible fiberoptic bronchoscope and similar devices has become among the preferred techniques in the management of such cases. Among the drawbacks of these devices are their high cost of purchase, maintenance and repair.<ref name=>{{cite journal | |||
|author=Kirkpatrick MB, Smith JR, Hoffman PJ, Middleton RM III | |||
|title=Bronchoscope damage and repair costs: results of a regional postal survey | |||
|journal=Respir Care | |||
|volume=37 | |||
|issue=11 | |||
|pages=1256-1259 | |||
|date=November 1992 | |||
|doi= | |||
|pmid=10145745 | |||
|url=http://www.ncbi.nlm.nih.gov/pubmed/10145745 | |||
|accessdate=17 July 2010}}</ref><ref name=>{{cite journal | |||
|author=Ales Rozman, Stefan Duh, Marija Petrinec-Primozic, Nadja Triller | |||
|title=Flexible Bronchoscope Damage and Repair Costs in a Bronchoscopy Teaching Unit | |||
|journal=Respiration | |||
|volume=77 | |||
|issue=3 | |||
|pages=325-330 | |||
|date=2009 | |||
|doi=10.1159/000188788 | |||
|pmid= | |||
|url=http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowPDF&ArtikelNr=188788&Ausgabe=246377&ProduktNr=224278&filename=188788.pdf | |||
|accessdate=17 July 2010}}</ref> Another drawback is that intubation with one of these devices can take considerably longer than that achieved using conventional laryngoscopy; this limits their use somewhat in urgent and emergent situations. | |||
Another | ===Rapid-sequence intubation=== | ||
Rapid-sequence intubation (RSI) refers to the method of sedation and paralysis prior to tracheal intubation. This technique is quicker than the process normally used to induce a state of general anesthesia. One important difference between RSI and routine tracheal intubation is that the practitoner does not ventilate the lungs after administration of a rapid-acting neuromuscular blocking agent. Another key feature of RSI is the application of manual pressure to the [[cricoid cartilage]] (this is referred to as the [[Sellick maneuver]]) prior to instrumentation of the airway and intubation of the trachea. | |||
RSI involves pre-oxygenating the patient with a tightly-fitting oxygen mask, followed by the sequential administration of pre-determined doses of a hypnotic drug and a rapid-acting neuromuscular blocker. Hypnotics used include thiopental, propofol and etomidate. Neuromuscular-blocking drugs used include suxamethonium (sometimes with a defasciculating dose of vecuronium) and rocuronium.[1] Other drugs may be used in a "modified" RSI. When performing endotracheal intubation, there are several adjunct medications available. No adjunctive medications, when given for their respective indications, have been proven to improve outcomes.[2] Opioids such as alfentanil or fentanyl may be given to attenuate the responses to the intubation process (tachycardia and raised intracranial pressure). This is supposed to have advantages in patients with ischemic heart disease and those with intra-cerebral hemorrhage (e.g. after traumatic head injury or stroke). Lidocaine is also theorized to blunt a rise in intracranial pressure during laryngoscopy, although this remains controversial and its use varies greatly. Atropine may be used to prevent a reflex bradycardia from vagal stimulation during laryngoscopy, especially in young children and infants. | |||
This procedure is usually performed by an anesthesiologist or CRNAs (certified registered nurse anesthetists) in surgery, by respiratory therapists in multiple settings, and by medical personnel in the emergency department. It may also be performed in the prehospital setting[1] by persons trained to the EMT-Intermediate or paramedic level, including flight medics and flight nurses. | |||
Another alternative is intubation of the awake patient under [[local anesthesia]] using a flexible endoscope or by other means (e.g., using a video laryngoscope). This technique is preferred if difficulties are anticipated, as it allows the patient to breathe spontaneously throughout the procedure, thus ensuring ventilation and oxygenation even in the event of a failed intubation. | |||
* | Some alternatives to intubation are | ||
* | *Tracheotomy - a surgical technique, typically for patients who require long-term respiratory support | ||
*Cricothyrotomy - an emergency technique used when intubation is unsuccessful and tracheotomy is not an option. | |||
Because the life of a patient can depend on the success of an intubation, it is important to assess possible obstacles beforehand. | |||
The ease of intubation is difficult to predict. One score to assess anatomical difficulties is the [[Mallampati score]],<ref name=>{{cite journal | |||
|author=S. Rao Mallampati, Stephen P. Gatt, Laverne D. Gugino, Sukumar P. Desai, Barbara Waraksa, Dubravka Freiberger, Philip L. Liu | |||
|title=A clinical sign to predict difficult tracheal intubation: a prospective study | |||
|journal=Canadian Journal of Anesthesia | |||
|volume=32 | |||
|issue=4 | |||
|pages=429-434 | |||
|date=July 1985 | |||
|doi=10.1007/BF03011357 | |||
|pmid=4027773 | |||
|url=http://www.springerlink.com/content/ep65t25471146547/fulltext.pdf | |||
|accessdate=17 July 2010}}</ref> which is determined by looking at the [[anatomy]] of the [[mouth]] and based on the visibility of the base of [[uvula]], [[Fauces (anatomy)|faucial pillar]]s and the [[soft palate]]. It should however be noted that no single score or combination of scores can be trusted to detect all patients who are difficult to intubate. Therefore, persons performing intubation must be familiar with alternative techniques of securing the airways. | |||
===Pediatric patients=== | |||
Most of the general principles of anesthesia can be applied to children, but there are some significant anatomical and physiological differences between children and adults that can cause problems, especially in neonates and children weighing less than 15 kg. For infants and young children, oral intubation is easier than nasal. Nasal route carries risk of dislodgement of adenoid tissue and epistaxis, but advantages include good fixation of tube. Because of good fixation, nasal route is preferable to oral route in children undergoing intensive care and requiring prolonged intubation. The position of the tube is checked by auscultation (equal air entry on each side and, in long-term intubation, by chest X-ray). Because the airway of a child is narrow, a small amount of oedema can produce severe obstruction. Edema can easily be caused by forcing in a tracheal tube that is too tight. (If length of the tube is suspected to be large, immediate changing it to the smaller size is suggestible.) | |||
= | The appropriate length for the endotracheal tube can be estimated by doubling the distance from the corner of the child's mouth to the ear canal. The tip of the tube should be at midtrachea, between the clavicles on an AP chest X-ray. The correct diameter of the tube is that which results in a small leak at a pressure of about 25 cm of water. The appropriate inner diameter for the endotracheal tube is roughly the same diameter as the child's little finger. For normally nourished children 2 years of age and older, the internal diameter of the tube can be calculated using the following formula: | ||
*Internal diameter of tube (mm) = (patient's age in years + 16) / 4 | |||
For neonates, 3 mm internal diameter is accepted while for premature infants 2.5 mm internal diameter is more appropriate. | |||
''' | ==Complications== | ||
Tracheal intubation is potentially a very dangerous invasive procedure that requires a great deal of clinical experience to master.<ref name=>{{cite journal | |||
|author=von Goedecke A, Herff H, Paal P, Dörges V, Wenzel V | |||
|title=Field airway management disasters | |||
|journal=Anesth Analg | |||
|volume=104 | |||
|issue=3 | |||
|pages=481-483 | |||
|date=March 2007 | |||
|doi=10.1213/01.ane.0000255964.86086.63 | |||
|pmid=17312190 | |||
|url=http://www.anesthesiaandanalgesia.net/content/104/3/481.full | |||
|accessdate=17 July 2010}}</ref> When performed improperly (e.g., unrecognized esophageal intubation), the associated complications may rapidly lead to the patient's death.<ref name=>{{cite book | |||
|author=Mazur, Glen | |||
|title=ACLS: Principles And Practice | |||
|editor=Richard O. Cummins | |||
|chapter= | |||
|publisher=[[American Heart Association]] | |||
|location=[[Dallas]], [[Texas]] | |||
|edition= | |||
|date=January 2004 | |||
|pages=135-180 | |||
|isbn=978-0874933413 | |||
|url= | |||
|accessdate=17 July 2010}}</ref> Consequently, in recent editions of its ''Guidelines for Cardiopulmonary Resuscitation'' the [[American Heart Association]] has de-emphasized the role of tracheal intubation in advanced airway maintenance, in favor of more basic techniques like bag-valve-mask ventilation.<ref>{{cite journal |chapter=Part 7.1: Adjuncts for Airway Control and Ventilation |title=2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care |journal=Circulation |volume=112 |issue=24 Suppl |pages=IV51–7 |year=2005 |month=Dec |pmid=16314375 |doi=10.1161/CIRCULATIONAHA.105.166550 |url=http://circ.ahajournals.org/cgi/content/full/112/24_suppl/IV-51 |author1=ECC Committee, Subcommittees and Task Forces of the American Heart Association}}</ref> Despite these concerns, tracheal intubation is still considered the definitive technique for airway management, as it allows the most reliable means of oxygenation and ventilation, while providing the highest level of protection against vomitus and regurgitation. | |||
( | Although the conventional laryngoscope has proven effective across a wide variety of settings and patients, its use and misuse can result in serious complications (e.g., trauma to oropharyngeal and [[dental trauma|dental]] structures). Newer technologies such as flexible fiberoptic laryngoscopy have fared better in reducing the incidence of such complications, though the most common cause of intubation trauma remains a lack of skill on the part of the laryngoscopist. | ||
==See also== | |||
* [[Bronchoscopy]] | |||
* [[Cricothyrotomy]] | |||
* [[Jet ventilation]] | |||
* [[Mechanical ventilation]] | |||
* [[Positive end-expiratory pressure]] | |||
* [[Positive pressure ventilation]] | |||
* [[Tracheobronchial injury]] | |||
* [[Tracheotomy]] | |||
==References== | |||
{{reflist}} | |||
== | |||
=== | ==Bibliography== | ||
*{{cite journal |author=Adnet F, Borron SW, Racine SX, ''et al.'' |title=The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation |journal=Anesthesiology |volume=87 |issue=6 |pages=1290–7 |year=1997 |month=Dec |pmid=9416711 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0003-3022&volume=87&issue=6&spage=1290 |doi=10.1097/00000542-199712000-00005}} | |||
The | *{{cite book |author=Ovassapian A |chapter=Conduct of anesthesia |editor=Shields TW |title=General thoracic surgery |publisher=Williams & Wilkins |location=Baltimore |year=1994 |pages=307–23 |isbn=0-683-07716-3 }} | ||
*{{cite journal |author=de Menezes Lyra R |title=Glottis simulator |journal=Anesth. Analg. |volume=88 |issue=6 |pages=1422–3 |year=1999 |month=Jun |pmid=10357358 |url=http://www.anesthesia-analgesia.org/cgi/pmidlookup?view=long&pmid=10357358 |doi=10.1097/00000539-199906000-00044}} | |||
=== | *{{cite journal |author=Smith NT |title=Simulation in anesthesia: the merits of large simulators versus small simulators |journal=Curr Opin Anaesthesiol |volume=13 |issue=6 |pages=659–65 |year=2000 |month=Dec |pmid=17016372 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0952-7907&volume=13&issue=6&spage=659 |doi=10.1097/00001503-200012000-00009}} | ||
* {{cite journal |author=Kabrhel C, Thomsen TW, Setnik GS, Walls RM |title=Videos in clinical medicine. Orotracheal intubation |journal=N Engl J Med. |volume=356 |issue=17 |pages=e15 |year=2007 |pmid=17460222 |doi=10.1056/NEJMvcm063574}} | |||
=== | |||
==== | |||
==== | |||
== | |||
==External links== | ==External links== | ||
* [http://airwaycam.com/video-library.html Videos of direct laryngoscopy recorded with the Airway Cam (TM) imaging system, a head mounted camera system that captures the perspective of the operator.] | |||
* [http://vam.anest.ufl.edu/airwaydevice/index.html Airway devices for intubation] | * [http://vam.anest.ufl.edu/airwaydevice/index.html Airway devices for intubation] | ||
{{Emergency medicine}} | {{Emergency medicine}} | ||
{{ | {{Intensive care medicine}} | ||
{{Respiratory system surgeries and other procedures}} | |||
[[Category:Anesthesia]] | |||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category: | [[Category:Emergency medical procedures]] | ||
[[Category:First aid]] | |||
[[Category:Intensive care medicine]] | |||
[[Category:Medical equipment]] | |||
[[Category:Oral and maxillofacial surgery]] | |||
[[Category:Otolaryngology]] | |||
[[Category:Pulmonology]] | [[Category:Pulmonology]] | ||
[[Category: | [[Category:Surgery]] | ||
[[ar:تنبيب (طب)]] | |||
[[ | [[cs:Intubace]] | ||
[[de:Tracheal intubation]] | |||
[[es:Intubación]] | |||
[[fr:Intubation trachéale]] | [[fr:Intubation trachéale]] | ||
[[he:צנרור]] | [[it:Intubazione]] | ||
[[he:צנרור קנה]] | |||
[[hu:Intubálás]] | |||
[[nl:Intubatie]] | [[nl:Intubatie]] | ||
[[ja:気管挿管]] | [[ja:気管挿管]] | ||
[[no:Intubasjon]] | [[no:Intubasjon]] | ||
[[pl:Intubacja]] | [[pl:Intubacja]] | ||
[[pt:Intubação | [[pt:Intubação traqueal]] | ||
[[ru:Интубация трахеи]] | |||
[[fi:Intubaatio]] | [[fi:Intubaatio]] | ||
[[sv:Intubation]] | [[sv:Intubation]] | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Revision as of 05:19, 18 July 2010

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch. Template:Interventions infobox Tracheal intubation (often simply referred to as intubation) is the placement of a flexible plastic tube into the trachea to protect the airway and provide a means of mechanical ventilation. The most common route for tracheal intubation is orotracheal where, with the assistance of a laryngoscope, an endotracheal tube is passed through the oropharynx, glottis, and larynx into the trachea. A bulb is then inflated near the distal tip of the tube to help secure it in place and protect the airway from blood, gastric contents and other secretions. Another route for tracheal intubation is nasotracheal, where an endotracheal tube is passed through the nasopharynx, glottis, and larynx into the trachea. Removal of the tube is referred to as extubation of the trachea.
History
Pre-19th century
The first known description of tracheal intubation was given in the 1020s by Avicenna in The Canon of Medicine in order to facilitate breathing.[1] The next known report on tracheal intubation and subsequent artificial respiration of animals was in 1543, when Andreas Vesalius pointed out that the technique could be life-saving.[citation needed] This report remained unnoticed for more than 250 years.
19th century
In 1805, Philip Bozzini used a device he invented and called the lichtleiter (or light-guiding instrument) to examine the human urinary bladder, rectum and pharynx.[citation needed] The practice of gastric endoscopy in humans was pioneered by U.S. Army surgeon William Beaumont in 1822 with the cooperation of his patient Alexis St. Martin, a victim of an accidental gunshot wound to the stomach.[2] In 1853, Antoine Jean Desormeaux of France examined the human bladder using a device he invented and called the endoscope (this was the first time this term was applied to this practice).[citation needed] In 1868, Adolph Kussmaul of Germany performed the first esophagogastroduodenoscopy on a living human. The subject was a sword-swallower, who swallowed a metal tube with a length of 47 centimeters and a diameter of 13 millimeters.[citation needed] In 1869, the German surgeon Friedrich Trendelenburg documented successful human tracheotomy for administration of general anesthesia.[citation needed] In 1878, the Scottish surgeon William Macewen performed the first orotracheal intubation.[citation needed] In 1878, Maximilian Nitze and Josef Leiter invented the cystourethroscope[citation needed] and in 1881, Jan Mikulicz-Radecki created the first rigid gastroscope for practical applications.[citation needed] On 23 April 1895, Alfred Kirstein performed the first direct laryngoscopy in Berlin, Germany, using an esophagoscope he had modified for this purpose.[3]
20th century
The 20th century saw the transformation of endoscopy and tracheal intubation from a rarely employed procedure to one which has become essential to the practices of anesthesia, critical care medicine, emergency medicine, gastroenterology, pulmonology, and surgery. During World War I, Sir Ivan Magill and Robert Macintosh achieved significant advances in techniques for tracheal intubation.[citation needed] The Magill curve of an endotracheal tube and the Magill forceps for positioning the tube during nasotracheal intubation are named after Magill, while the most widely used curved laryngoscope blade is named after Macintosh. In 1932, Rudolph Schindler of Germany introduced the first semi-flexible gastroscope.[citation needed] This device had numerous lenses positioned throughout the tube and a miniature light bulb at the distal tip. The tube of this device was 75 centimeters in length and 11 millimeters in diameter, and the distal portion was capable of a certain degree of flexion. Between 1945 and 1952, optical engineers (notably Karl Storz of Germany, Harold Hopkins of England, and Mutsuo Sugiura of the Japanese Olympus Corporation) built upon this early work, leading to the development of the first gastrocamera.[citation needed] In 1964, Fernando Alves Martins of Portugal applied optical fiber technology to one of these early gastrocameras to produce the first gastrocamera with a flexible fiberscope.[citation needed] Initially used in esophagogastroduodenoscopy, newer devices were developed in the early 1970s for use in bronchoscopy, rhinoscopy, and laryngoscopy. By the mid-1980s, the flexible fiberoptic bronchoscope had become an indispensable instrument within the pulmonology and anesthesia communities.
21st century
The Digital Revolution has brought newer technology to the art and science of tracheal intubation. Several manufacturers have developed video laryngoscopes which employ digital technology such as the CMOS active pixel sensor (CMOS APS) to generate a view of the glottis so that the trachea may be intubated. The Glidescope video laryngoscope is one example of such a device.[citation needed]
Indications
A definitive airway (orotracheal, nasotracheal, cricothyrotomy, or tracheotomy) is indicated under any of the following circumstances:
- Comatose or intoxicated patients with a depressed level of consciousness who are unable to protect their airways. This is commonly defined as those subjects with a Glasgow Coma Scale ≤ 8. In such cases, the throat muscles may lose their tone so that the hypopharynx becomes obstructed, impeding the free flow of air into the lungs. Furthermore, protective airway reflexes such as coughing and swallowing, which serve to protect the airways against aspiration of secretions and foreign bodies, may be absent. With tracheal intubation, airway patency is restored and the lower airways can be protected from aspiration.
- Requirement for mechanical ventilation, including cardiopulmonary resuscitation and general anesthesia. In such situations, spontaneous ventilation may be decreased or absent due to the effect of injury, disease, anesthetic agents, opioids, or neuromuscular-blocking drugs. To enable mechanical ventilation, an endotracheal tube is often used, although there are alternative devices such as the laryngeal mask airway or the CPAP mask.
- Apnea or hypoventilation (e.g., closed head injury, intoxication or poisoning, cervical spine injury, flail chest)
- Persistent or recurrent airway obstruction
- Impending or potential compromise of the airway (e.g., sustained seizure activity, facial fractures, expanding neck hematoma, laryngeal or tracheobronchial injury, airway burns, inhalation injury)
- Inability to maintain oxygenation using face mask oxygen supplementation (severe pneumonia, acute respiratory distress syndrome (ARDS), near-drowning, etc.)
- Diagnostic or therapeutic manipulation of the airway (such as bronchoscopy, laser therapy or stenting of the bronchi).
Equipment
Laryngoscopes
The vast majority of "noninvasive" tracheal intubations involve the use of a viewing instrument or "scope" of one type or another. Since its introduction by Kirstein in 1895, the most common device used for this purpose has been the conventional laryngoscope. Today, the typical conventional laryngoscope consists of a handle, usually containing batteries, and a set of interchangeable blades. Two basic styles of laryngoscope blade are commercially available: the straight blade and the curved blade. The Macintosh blade is the most widely used of the curved laryngoscope blades, while the Miller blade is the most popular style of straight blade. There are many other styles of straight and curved blades, with accessories such as mirrors for enlarging the field of view and even ports for the administration of oxygen. These specialty blades are primarily designed for use by anesthetists, most commonly in the operating room.
Besides the conventional laryngoscopes, many devices have been developed as alternatives to direct laryngoscopy. These include a number of indirect fiberoptic viewing laryngoscopes such as the flexible fiberoptic bronchoscope, Bullard scope, UpsherScope,[4] and the WuScope. These devices are widely employed for tracheal intubation, especially in the setting of the difficult intubation (see below). Several types of video laryngoscopes are also currently available (e.g., Glidescope, McGrath laryngoscope, Daiken Medical Coopdech C-scope vlp-100, the Storz C-Mac, Pentax AWS and the Berci DCI). Other noninvasive devices which are commonly employed for tracheal intubation are the laryngeal mask airway (used as a guide for tracheal tube placement), the lighted stylet, and the AirTraq. Due to the widespread availability of such devices, the technique of blind digital intubation of the trachea is rarely practiced today, though it may still be useful in emergency situations under austere conditions such as natural or man-made disasters.
Stylets
A stylet is a malleable metal wire which can be inserted into the endotracheal tube to make the tube conform better to the laryngopharyngeal anatomy of the specific individual, thus facilitating its insertion. It is commonly employed under circumstances of difficult laryngoscopy. The Eschmann stylet or gum elastic bougie is a specialized type of stylet, which can also be used for difficult laryngoscopy or for removal and replacement of tracheal tubes without the need for laryngoscopy.
Tracheal tubes
Most tracheal tubes today are constructed of polyvinyl chloride, but specialty tubes constructed of silicone rubber, latex rubber, or stainless steel are also widely available. Most tubes have an inflatable cuff to seal the trachea and bronchial tree against air leakage and aspiration of gastric contents, blood, secretions, and other fluids. Uncuffed tubes are also available, though their use is limited mostly to pediatric patients (in small children, the cricoid cartilage, the narrowest portion of the pediatric airway, often provides an adequate seal for mechanical ventilation).
The "armored endotracheal tube" is a cuffed, wire-reinforced, silicone rubber tube which is quite flexible but yet difficult to compress or kink. This can make it useful for situations in which the trachea is anticipated to remain intubated for a prolonged duration, or if the neck is to remain flexed during surgery. Polyvinyl chloride tubes are relatively stiff in comparison. Preformed tubes (such as the oral and nasal RAE tubes, named after the inventors Ring, Adair and Elwyn) are also widely available for special applications. These may also be constructed of polyvinyl chloride or wire-reinforced silicone rubber. Other tubes (such as the Bivona® Fome-Cuf® tube) are designed specifcally for use in laser surgery in and around the airway. Various types of double-lumen endotracheal tubes have been developed (Carlens, Robertshaw, etc.) for ventilating each lung independently—this is useful during pulmonary and other thoracic operations.
Observational methods to confirm tube placement
- Direct visualization of the tube passing through the vocal cords
- Clear and equal bilateral breath sounds on auscultation of the chest
- Absent sounds on auscultation of the epigastrium
- Equal bilateral chest rise with ventilation
- Fogging of the tube
- An absence of stomach contents in the tube
Instruments to confirm tube placement
No single method for confirming tracheal tube placement has been shown to be 100% reliable. Accordingly, the use of multiple methods to confirm correct tube placement is now widely considered to be the standard of care. At least one of the methods utilized should be an instrument. Waveform capnography has emerged as the gold standard for the confirmation of correct tube placement and maintenance of the tube once it is in place. Other methods include:
- Colorimetric end tidal carbon dioxide detector
- Self-inflating esophageal bulb
- Pulse oximetry (important limitations include a significant delay in the decrease in oxygen saturation, especially if subject has been pre-oxygenated)
- Esophageal Detection Device[5]
Predicting ease of intubation
- Look externally (history of craniofacial traumas/previous surgery)
- Evaluate 3,3,2 - three of the subject's fingers should be able to fit into his/her mouth when open, three fingers should comfortably fit between the chin and the throat, and two fingers in the thyromental distance (distance from thyroid cartilage to chin)
- Mallampati score
- Obstructions (stridorous breath sounds, wheezing, etc.)
- Neck mobility (can subject tilt head back and then forward to touch chest)
- Cormack-Lehane grading system (according to the percentage of glottic opening on laryngoscopy)
Tracheal tube maintenance
The tube is secured in place with tape or an endotracheal tube holder. A cervical collar is sometimes used to prevent motion of the airway. Tube placement should be confirmed after each physical move of the patient and after any unexplained change in his/her clinical status. Continuous pulse oximetry and continuous waveform capnography are often used to monitor the tube's correct placement.
The cuff pressure must be monitored carefully in order to avoid complications from over-inflation, which can include tracheomalacia, tracheoesophageal fistula, or even frank rupture of the trachea. Many of the complications of over-inflated cuffs can be traced to excessive cuff pressure causing ischemia of the tracheal mucosa.[6]
An excessive leak can sometimes be corrected through the placement of a larger (0.5 mm larger in internal diameter) endotracheal tube, and in difficult-to-ventilate pediatric patients children it is often necessary to use cuffed tubes to allow for high pressure ventilation if the leak is too great to overcome with the ventilator.[7]
Special situations
Emergency intubation
Personnel experienced in direct laryngoscopy are not always immediately available in certain settings that require emergency tracheal intubation. For this reason, specialized devices have been designed to act as bridges to a definitive airway. Such devices include the laryngeal mask airway, cuffed oropharyngeal airway, and the Combitube.[8] Other devices such as rigid stylets, the lightwand (a blind technique) and indirect fiberoptic rigid stylets, such as the Bullard scope, Upsher scope, and the WuScope can also be used as alternatives to direct laryngoscopy. Each of these devices have its own unique set of benefits and drawbacks, and none of them is effective under all circumstances.
Difficult intubation
Many individuals have unusual airway anatomy, such as those who have limited range of motion of the cervical spine or temporomandibular joint, or who have oropharyngeal tumors, hematomas, angioedema, micrognathia, retrognathia, or excess adipose tissue of the face and neck. Using conventional laryngoscopic techniques, intubation of the trachea can be difficult in such people. Use of the flexible fiberoptic bronchoscope and similar devices has become among the preferred techniques in the management of such cases. Among the drawbacks of these devices are their high cost of purchase, maintenance and repair.[9][10] Another drawback is that intubation with one of these devices can take considerably longer than that achieved using conventional laryngoscopy; this limits their use somewhat in urgent and emergent situations.
Rapid-sequence intubation
Rapid-sequence intubation (RSI) refers to the method of sedation and paralysis prior to tracheal intubation. This technique is quicker than the process normally used to induce a state of general anesthesia. One important difference between RSI and routine tracheal intubation is that the practitoner does not ventilate the lungs after administration of a rapid-acting neuromuscular blocking agent. Another key feature of RSI is the application of manual pressure to the cricoid cartilage (this is referred to as the Sellick maneuver) prior to instrumentation of the airway and intubation of the trachea.
RSI involves pre-oxygenating the patient with a tightly-fitting oxygen mask, followed by the sequential administration of pre-determined doses of a hypnotic drug and a rapid-acting neuromuscular blocker. Hypnotics used include thiopental, propofol and etomidate. Neuromuscular-blocking drugs used include suxamethonium (sometimes with a defasciculating dose of vecuronium) and rocuronium.[1] Other drugs may be used in a "modified" RSI. When performing endotracheal intubation, there are several adjunct medications available. No adjunctive medications, when given for their respective indications, have been proven to improve outcomes.[2] Opioids such as alfentanil or fentanyl may be given to attenuate the responses to the intubation process (tachycardia and raised intracranial pressure). This is supposed to have advantages in patients with ischemic heart disease and those with intra-cerebral hemorrhage (e.g. after traumatic head injury or stroke). Lidocaine is also theorized to blunt a rise in intracranial pressure during laryngoscopy, although this remains controversial and its use varies greatly. Atropine may be used to prevent a reflex bradycardia from vagal stimulation during laryngoscopy, especially in young children and infants.
This procedure is usually performed by an anesthesiologist or CRNAs (certified registered nurse anesthetists) in surgery, by respiratory therapists in multiple settings, and by medical personnel in the emergency department. It may also be performed in the prehospital setting[1] by persons trained to the EMT-Intermediate or paramedic level, including flight medics and flight nurses.
Another alternative is intubation of the awake patient under local anesthesia using a flexible endoscope or by other means (e.g., using a video laryngoscope). This technique is preferred if difficulties are anticipated, as it allows the patient to breathe spontaneously throughout the procedure, thus ensuring ventilation and oxygenation even in the event of a failed intubation.
Some alternatives to intubation are
- Tracheotomy - a surgical technique, typically for patients who require long-term respiratory support
- Cricothyrotomy - an emergency technique used when intubation is unsuccessful and tracheotomy is not an option.
Because the life of a patient can depend on the success of an intubation, it is important to assess possible obstacles beforehand. The ease of intubation is difficult to predict. One score to assess anatomical difficulties is the Mallampati score,[11] which is determined by looking at the anatomy of the mouth and based on the visibility of the base of uvula, faucial pillars and the soft palate. It should however be noted that no single score or combination of scores can be trusted to detect all patients who are difficult to intubate. Therefore, persons performing intubation must be familiar with alternative techniques of securing the airways.
Pediatric patients
Most of the general principles of anesthesia can be applied to children, but there are some significant anatomical and physiological differences between children and adults that can cause problems, especially in neonates and children weighing less than 15 kg. For infants and young children, oral intubation is easier than nasal. Nasal route carries risk of dislodgement of adenoid tissue and epistaxis, but advantages include good fixation of tube. Because of good fixation, nasal route is preferable to oral route in children undergoing intensive care and requiring prolonged intubation. The position of the tube is checked by auscultation (equal air entry on each side and, in long-term intubation, by chest X-ray). Because the airway of a child is narrow, a small amount of oedema can produce severe obstruction. Edema can easily be caused by forcing in a tracheal tube that is too tight. (If length of the tube is suspected to be large, immediate changing it to the smaller size is suggestible.)
The appropriate length for the endotracheal tube can be estimated by doubling the distance from the corner of the child's mouth to the ear canal. The tip of the tube should be at midtrachea, between the clavicles on an AP chest X-ray. The correct diameter of the tube is that which results in a small leak at a pressure of about 25 cm of water. The appropriate inner diameter for the endotracheal tube is roughly the same diameter as the child's little finger. For normally nourished children 2 years of age and older, the internal diameter of the tube can be calculated using the following formula:
- Internal diameter of tube (mm) = (patient's age in years + 16) / 4
For neonates, 3 mm internal diameter is accepted while for premature infants 2.5 mm internal diameter is more appropriate.
Complications
Tracheal intubation is potentially a very dangerous invasive procedure that requires a great deal of clinical experience to master.[12] When performed improperly (e.g., unrecognized esophageal intubation), the associated complications may rapidly lead to the patient's death.[13] Consequently, in recent editions of its Guidelines for Cardiopulmonary Resuscitation the American Heart Association has de-emphasized the role of tracheal intubation in advanced airway maintenance, in favor of more basic techniques like bag-valve-mask ventilation.[14] Despite these concerns, tracheal intubation is still considered the definitive technique for airway management, as it allows the most reliable means of oxygenation and ventilation, while providing the highest level of protection against vomitus and regurgitation.
Although the conventional laryngoscope has proven effective across a wide variety of settings and patients, its use and misuse can result in serious complications (e.g., trauma to oropharyngeal and dental structures). Newer technologies such as flexible fiberoptic laryngoscopy have fared better in reducing the incidence of such complications, though the most common cause of intubation trauma remains a lack of skill on the part of the laryngoscopist.
See also
- Bronchoscopy
- Cricothyrotomy
- Jet ventilation
- Mechanical ventilation
- Positive end-expiratory pressure
- Positive pressure ventilation
- Tracheobronchial injury
- Tracheotomy
References
- ↑ Patricia Skinner (2008). "Unani-tibbi". In Laurie J. Fundukian. The Gale Encyclopedia of Alternative Medicine (3rd ed.). Farmington Hills, Michigan: Gale Cengage. ISBN 9781414448725. Retrieved 17 July 2010. External link in
|publisher=(help) - ↑ William Beaumont and Andrew Combe (1838). Experiments and observations on the gastric juice, and the physiology of digestion. Edinburgh: MacLachlan & Stewart. p. 319. Retrieved 12 July 2010.
- ↑ N.P. Hirsch, G.B. Smith, and P.O. Hirsch (January 1986). "Alfred Kirstein: Pioneer of direct laryngoscopy". Anaesthesia. 41 (1): 42–45. doi:10.1111/j.1365-2044.1986.tb12702.x. Retrieved 10 July 2010.
- ↑ Peter Fridrich, Michael Frass, Claus G. Krenn, Christian Weinstabl, Jonathan L. Benumof, and Peter Krafft (December 1997). "The UpsherScope in routine and difficult airway management: a randomized, controlled clinical trial". Anesth Analg. 85 (6): 1377–1381. doi:10.1097/00000539-199712000-00036. PMID 9390612. Retrieved 17 July 2010.
- ↑ Tim Wolfe, M.D. (May 1998). "The Esophageal Detector Device: Summary of the current articles in the literature". Salt Lake City, Utah: Wolfe Tory Medical, Inc. Retrieved 17 July 2010. External link in
|publisher=(help) - ↑ Papiya Sengupta, Daniel I Sessler, Paul Maglinger, Spencer Wells, Alicia Vogt, Jaleel Durrani, and Anupama Wadhwa (2004). "Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure". BMC Anesthesiology. 4 (1): 8. doi:10.1186/1471-2253-4-8. PMID 15569386. Retrieved 17 July 2010. Unknown parameter
|PMCID=ignored (|pmc=suggested) (help) - ↑ Sheridan RL (May 2006). "Uncuffed endotracheal tubes should not be used in seriously burned children". Pediatr Crit Care Med. 7 (3): 258–259. doi:10.1097/01.PCC.0000216681.71594.04. PMID 16575345. Retrieved 17 July 2010.
- ↑ Foley LJ, Ochroch EA (July 2000). "Bridges to establish an emergency airway and alternate intubating techniques". Critical Care Clinics. 16 (3): 429–444. doi:10.1016/S0749-0704%2805%2970121-4. PMID 10941582. Retrieved 16 July 2010.
- ↑ Kirkpatrick MB, Smith JR, Hoffman PJ, Middleton RM III (November 1992). "Bronchoscope damage and repair costs: results of a regional postal survey". Respir Care. 37 (11): 1256–1259. PMID 10145745. Retrieved 17 July 2010.
- ↑ Ales Rozman, Stefan Duh, Marija Petrinec-Primozic, Nadja Triller (2009). "Flexible Bronchoscope Damage and Repair Costs in a Bronchoscopy Teaching Unit" (PDF). Respiration. 77 (3): 325–330. doi:10.1159/000188788. Retrieved 17 July 2010.
- ↑ S. Rao Mallampati, Stephen P. Gatt, Laverne D. Gugino, Sukumar P. Desai, Barbara Waraksa, Dubravka Freiberger, Philip L. Liu (July 1985). "A clinical sign to predict difficult tracheal intubation: a prospective study" (PDF). Canadian Journal of Anesthesia. 32 (4): 429–434. doi:10.1007/BF03011357. PMID 4027773. Retrieved 17 July 2010.
- ↑ von Goedecke A, Herff H, Paal P, Dörges V, Wenzel V (March 2007). "Field airway management disasters". Anesth Analg. 104 (3): 481–483. doi:10.1213/01.ane.0000255964.86086.63. PMID 17312190. Retrieved 17 July 2010.
- ↑ Mazur, Glen (January 2004). Richard O. Cummins, ed. ACLS: Principles And Practice. Dallas, Texas: American Heart Association. pp. 135–180. ISBN 978-0874933413.
|access-date=requires|url=(help) - ↑ ECC Committee, Subcommittees and Task Forces of the American Heart Association (2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 112 (24 Suppl): IV51–7. doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375. Unknown parameter
|month=ignored (help);|chapter=ignored (help)
Bibliography
- Adnet F, Borron SW, Racine SX; et al. (1997). "The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation". Anesthesiology. 87 (6): 1290–7. doi:10.1097/00000542-199712000-00005. PMID 9416711. Unknown parameter
|month=ignored (help) - Ovassapian A (1994). "Conduct of anesthesia". In Shields TW. General thoracic surgery. Baltimore: Williams & Wilkins. pp. 307–23. ISBN 0-683-07716-3.
- de Menezes Lyra R (1999). "Glottis simulator". Anesth. Analg. 88 (6): 1422–3. doi:10.1097/00000539-199906000-00044. PMID 10357358. Unknown parameter
|month=ignored (help) - Smith NT (2000). "Simulation in anesthesia: the merits of large simulators versus small simulators". Curr Opin Anaesthesiol. 13 (6): 659–65. doi:10.1097/00001503-200012000-00009. PMID 17016372. Unknown parameter
|month=ignored (help) - Kabrhel C, Thomsen TW, Setnik GS, Walls RM (2007). "Videos in clinical medicine. Orotracheal intubation". N Engl J Med. 356 (17): e15. doi:10.1056/NEJMvcm063574. PMID 17460222.
External links
- Videos of direct laryngoscopy recorded with the Airway Cam (TM) imaging system, a head mounted camera system that captures the perspective of the operator.
- Airway devices for intubation
Template:Respiratory system surgeries and other procedures
ar:تنبيب (طب) cs:Intubace de:Tracheal intubation it:Intubazione he:צנרור קנה hu:Intubálás nl:Intubatie no:Intubasjon fi:Intubaatio sv:Intubation
- CS1 errors: external links
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- Pages using citations with accessdate and no URL
- CS1 errors: chapter ignored
- Pages using duplicate arguments in template calls
- All articles with unsourced statements
- Articles with unsourced statements from July 2010
- Articles with invalid date parameter in template
- Pages with broken file links
- CS1 maint: Explicit use of et al.
- Anesthesia
- Emergency medicine
- Emergency medical procedures
- First aid
- Intensive care medicine
- Medical equipment
- Oral and maxillofacial surgery
- Otolaryngology
- Pulmonology
- Surgery