Sandbox: hyperthyroidism landing: Difference between revisions
Ahmed Younes (talk | contribs) |
Ahmed Younes (talk | contribs) No edit summary |
||
| Line 7: | Line 7: | ||
===Overview=== | ===Overview=== | ||
Hyperthyroidism is a disorder that the thyroid gland makes too much [[thyroid hormone]]. About 1 percent of the U.S. population has hyperthyroidism. Some diseases, such as [[Graves’ disease]], thyroid nodules and [[thyroiditis]], are associated with the cause of hyperthyroidism. Hyperthyroidism can affect your metabolism. Usual signs and symptoms include [[goiter]], increased appetite but [[weight loss]], [[palpitation]], [[hypertension]], increased sensitivity to heat and perspiration, [[nervousness]] and hand [[tremors]]. The Thyroid-Stimulating Hormone (TSH) test is a very sensitive and useful test to identify the disorder. Other examinations include the [[T3]] and [[T4]] test, radioactive iodine uptake test and thyroid scan. Treatment options of hyperthyroidism | Hyperthyroidism is a disorder that the thyroid gland makes too much [[thyroid hormone]]. About 1 percent of the U.S. population has hyperthyroidism. Some diseases, such as [[Graves’ disease]], thyroid nodules and [[thyroiditis]], are associated with the cause of hyperthyroidism. Hyperthyroidism can affect your metabolism. Usual signs and symptoms include [[goiter]], increased appetite but [[weight loss]], [[palpitation]], [[hypertension]], increased sensitivity to heat and perspiration, [[nervousness]] and hand [[tremors]]. The Thyroid-Stimulating Hormone (TSH) test is a very sensitive and useful test to identify the disorder. Other examinations include the [[T3]] and [[T4]] test, radioactive iodine uptake test and thyroid scan. Treatment options of hyperthyroidism depend on the cause, age, physical condition and the severity of symptoms. Usual treatment measures are medications, radioactive iodine and [[thyroidectomy]]. The common [[side effect]] of radioactive iodine and [[thyroidectomy]] is [[hypothyroidism]]. The patient will need to take thyroid hormone supplement to restore normal hormone levels. | ||
===What are the symptoms of Hyperthyroidism?=== | ===What are the symptoms of Hyperthyroidism?=== | ||
| Line 51: | Line 51: | ||
===Treatment options=== | ===Treatment options=== | ||
Usual treatment measures of hyperthyroidism include medications, radioactive iodine, and surgery. Treatment options | Usual treatment measures of hyperthyroidism include medications, radioactive iodine, and surgery. Treatment options depend on the cause, age, physical condition and the severity of symptoms. | ||
*Medications: Antithyroid medications, such as [[methimazole]] (Tapazole) and [[propylthiouracil]] (PTU), are used to block the production of thyroid hormone. Symptoms may begin to improve in 6 to 12 weeks and the whole treatment period may last for at least a year. [[Beta blockers]], for example [[propranolol]], may be used to relieve symptoms such as [[palpitation]], [[nervousness]],[[hypertension]], [[sweating]] and [[shaking]]. | *Medications: Antithyroid medications, such as [[methimazole]] (Tapazole) and [[propylthiouracil]] (PTU), are used to block the production of thyroid hormone. Symptoms may begin to improve in 6 to 12 weeks and the whole treatment period may last for at least a year. [[Beta blockers]], for example [[propranolol]], may be used to relieve symptoms such as [[palpitation]], [[nervousness]],[[hypertension]], [[sweating]] and [[shaking]]. | ||
*Radioactive iodine: This kind of treatment may destroy the thyroid gland and stop the excess production of [[hormone]]s. During this period, the patient takes radioactive iodine by mouth. A common [[side effect]] is permanent hypothyroidism, which needs thyroid supplements. | *Radioactive iodine: This kind of treatment may destroy the thyroid gland and stop the excess production of [[hormone]]s. During this period, the patient takes radioactive iodine by mouth. A common [[side effect]] is permanent hypothyroidism, which needs thyroid supplements. | ||
| Line 105: | Line 105: | ||
*Metastatic follicular thyroid cancer | *Metastatic follicular thyroid cancer | ||
*[[Pituitary tumor]] | *[[Pituitary tumor]] | ||
*[[Struma | *[[Struma ovarii ]] | ||
*[[Teratoma]] | *[[Teratoma]] | ||
*[[Testicular cancer]] | *[[Testicular cancer]] | ||
| Line 149: | Line 149: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Endocrine''' | | '''Endocrine''' | ||
| bgcolor="Beige" | [[Anterior pituitary hyperhormonotrophic syndrome]], [[Autoimmune enteropathy]], [[Autoimmune thyroid disease]], [[Autonomous thyroid tissue ]] , [[Choriocarcinoma]], [[De quervain thyroiditis]], [[Excessive replacement therapy]], [[Exogenous thyroid hormone intake]], [[Factitious thyroiditis ]] , [[Graves' | | bgcolor="Beige" | [[Anterior pituitary hyperhormonotrophic syndrome]], [[Autoimmune enteropathy]], [[Autoimmune thyroid disease]], [[Autonomous thyroid tissue ]] , [[Choriocarcinoma]], [[De quervain thyroiditis]], [[Excessive replacement therapy]], [[Exogenous thyroid hormone intake]], [[Factitious thyroiditis ]] , [[Graves' disease ]] , [[Hashimoto's thyroiditis]], [[Jod-basedow thyrotoxicosis]], [[Metastatic follicular thyroid cancer]], [[Pituitary tumor]], [[Polyendocrinopathy]], [[Polyostotic fibrous dysplasia]], [[Postpartum thyroiditis]], [[Suppurative thyroiditis]], [[Thyroid adenoma]], [[Thyroid carcinoma]], [[Thyroid nodule]], [[Thyroid stimulating globulin]], [[Thyroid tumor]], [[Thyroiditis]], [[Thyrotropinoma]], [[Toxic adenoma]], [[Toxic multinodular goiter]], [[Toxic thyroid adenoma]], [[Tsh hypersecretion]], [[Tsh-mediated hyperthyroidism]], [[Tsh-producing pituitary adenoma]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 161: | Line 161: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Genetic''' | | '''Genetic''' | ||
| bgcolor="Beige" | [[Glutaricaciduria type 3]], [[Ipex | | bgcolor="Beige" | [[Glutaricaciduria type 3]], [[Ipex syndrome ]] , [[Mccune-albright syndrome ]] , [[Troell-junet syndrome]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 169: | Line 169: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Iatrogenic''' | | '''Iatrogenic''' | ||
| bgcolor="Beige" | [[Excessive replacement therapy]], [[Exogenous thyroid hormone intake]], [[Intentional suppressive therapy]], [[Iodine | | bgcolor="Beige" | [[Excessive replacement therapy]], [[Exogenous thyroid hormone intake]], [[Intentional suppressive therapy]], [[Iodine overuse ]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 193: | Line 193: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Oncologic''' | | '''Oncologic''' | ||
| bgcolor="Beige" | [[Adenocarcinoma]], [[Choriocarcinoma]], [[Metastatic follicular thyroid cancer]], [[Pituitary tumor]], [[Struma | | bgcolor="Beige" | [[Adenocarcinoma]], [[Choriocarcinoma]], [[Metastatic follicular thyroid cancer]], [[Pituitary tumor]], [[Struma ovarii ]] , [[Teratoma]], [[Testicular cancer]], [[Thyroid adenoma]], [[Thyroid carcinoma]], [[Thyroid nodule]], [[Thyroid tumor]], [[Thyrotropinoma]], [[Toxic adenoma]], [[Toxic thyroid adenoma]], [[Trophoblastic disease]], [[Tsh-producing pituitary adenoma]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 201: | Line 201: | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Overdose/Toxicity''' | | '''Overdose/Toxicity''' | ||
| bgcolor="Beige" | [[Iodine | | bgcolor="Beige" | [[Iodine overuse ]] | ||
|- | |- | ||
|- bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| Line 255: | Line 255: | ||
*[[Factitious thyroiditis ]] | *[[Factitious thyroiditis ]] | ||
*[[Glutaricaciduria type 3]] | *[[Glutaricaciduria type 3]] | ||
*[[Graves' | *[[Graves' disease ]] | ||
*[[Hashimoto's thyroiditis]] | *[[Hashimoto's thyroiditis]] | ||
*[[Hashitoxicosis]] | *[[Hashitoxicosis]] | ||
| Line 262: | Line 262: | ||
*[[Immune dysregulation]] | *[[Immune dysregulation]] | ||
*[[Intentional suppressive therapy]] | *[[Intentional suppressive therapy]] | ||
*[[Iodine | *[[Iodine overuse ]] | ||
*[[Ipex | *[[Ipex syndrome ]] | ||
*[[Jod-basedow thyrotoxicosis]] | *[[Jod-basedow thyrotoxicosis]] | ||
*[[Levothyroxine and indinavir interaction]] | *[[Levothyroxine and indinavir interaction]] | ||
*[[Mccune-albright | *[[Mccune-albright syndrome ]] | ||
*[[Metastatic follicular thyroid cancer]] | *[[Metastatic follicular thyroid cancer]] | ||
*[[Nivolumab]] | *[[Nivolumab]] | ||
*[[Pituitary tumor]] | *[[Pituitary tumor]] | ||
*[[Poems | *[[Poems syndrome ]] | ||
*[[Polyendocrinopathy]] | *[[Polyendocrinopathy]] | ||
*[[Polyostotic fibrous dysplasia]] | *[[Polyostotic fibrous dysplasia]] | ||
| Line 277: | Line 277: | ||
*[[Pramipexole]] | *[[Pramipexole]] | ||
*[[Sorafenib]] | *[[Sorafenib]] | ||
*[[Struma | *[[Struma ovarii ]] | ||
*[[Suppurative thyroiditis]] | *[[Suppurative thyroiditis]] | ||
*[[Teratoma]] | *[[Teratoma]] | ||
| Line 325: | Line 325: | ||
*Hashitoxicosis | *Hashitoxicosis | ||
*Germ cell tumors (choriocarcinoma in males and testicular germ cell tumors) | *Germ cell tumors (choriocarcinoma in males and testicular germ cell tumors) | ||
*Pituitary TSH producing adenoma | *Pituitary TSH-producing adenoma | ||
===Low uptake=== | ===Low uptake=== | ||
*Subacute thyroiditis | *Subacute thyroiditis | ||
* | *Hyperthyroidism due to ectopic thyroid tissue | ||
==Pathophysiology== | ==Pathophysiology== | ||
Revision as of 14:55, 6 July 2017
Template:Hyperthyroidism landing Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Patient information
Overview
Hyperthyroidism is a disorder that the thyroid gland makes too much thyroid hormone. About 1 percent of the U.S. population has hyperthyroidism. Some diseases, such as Graves’ disease, thyroid nodules and thyroiditis, are associated with the cause of hyperthyroidism. Hyperthyroidism can affect your metabolism. Usual signs and symptoms include goiter, increased appetite but weight loss, palpitation, hypertension, increased sensitivity to heat and perspiration, nervousness and hand tremors. The Thyroid-Stimulating Hormone (TSH) test is a very sensitive and useful test to identify the disorder. Other examinations include the T3 and T4 test, radioactive iodine uptake test and thyroid scan. Treatment options of hyperthyroidism depend on the cause, age, physical condition and the severity of symptoms. Usual treatment measures are medications, radioactive iodine and thyroidectomy. The common side effect of radioactive iodine and thyroidectomy is hypothyroidism. The patient will need to take thyroid hormone supplement to restore normal hormone levels.
What are the symptoms of Hyperthyroidism?
Symptoms of hyperthyroidism vary from person to person. Usual signs include the following:
- Goiter
- Increased appetite, but weight loss
- Palpitation
- Hypertension
- Increased sensitivity to heat and perspiration
- Nervousness, anxiety or irritability, difficulty sleeping
- Hand tremors
- Fatigue, muscle weakness
- Changes in menstrual patterns (usually lighter flow, less frequent periods) in women
Other health problems may also cause these symptoms. Only a doctor can tell for sure. A person with any of these symptoms should tell the doctor so that the problems can be diagnosed and treated as early as possible.
Who is at highest risk?
- Graves’ disease
- Thyroid nodules
- Thyroiditis
- Too much iodine ingestion
- Over-medicating with synthetic thyroid hormone
Diagnosis
- Thyroid-Stimulating Hormone (TSH) test: This is a very sensitive and useful test and usually used as the first test to identify the disorder. The TSH test is based on the feedback between TSH and thyroid hormone. Patients with hyperthyroidism may show a lower reading than normal people.
- T3 and T4 test: This test may show the levels of T3 and T4 in your blood. In patients with hyperthyroidism, the levels of one or both of these hormones in your blood will be higher than normal.
- Thyroid-stimulating immunoglobulin (TSI) test: This test may help diagnose Graves' disease, which has this kind of antibody.
- Radioactive iodine uptake test: This test can detect the iodine uptake function of your thyroid gland and help diagnose the cause of hyperthyroidism. For example, low levels of iodine uptake might be a sign of thyroiditis, whereas high levels could indicate Graves’ disease.
- Thyroid scan: This test may also help diagnose the cause of hyperthyroidism by providing images of nodules and other possible thyroid irregularities.
Other diseases with similar symptoms:
- Autonomic nerve dysfunction
- Coronary artery disease
- Goiter
- Schizophrenia
- Thyroid cancer
When to seek urgent medical care?
Call your health care provider if symptoms of hyperthyroidism develop. If you experience either of the following symptoms, seeking urgent medical care as soon as possible:
- Palpitation
- Severe hypertension
Treatment options
Usual treatment measures of hyperthyroidism include medications, radioactive iodine, and surgery. Treatment options depend on the cause, age, physical condition and the severity of symptoms.
- Medications: Antithyroid medications, such as methimazole (Tapazole) and propylthiouracil (PTU), are used to block the production of thyroid hormone. Symptoms may begin to improve in 6 to 12 weeks and the whole treatment period may last for at least a year. Beta blockers, for example propranolol, may be used to relieve symptoms such as palpitation, nervousness,hypertension, sweating and shaking.
- Radioactive iodine: This kind of treatment may destroy the thyroid gland and stop the excess production of hormones. During this period, the patient takes radioactive iodine by mouth. A common side effect is permanent hypothyroidism, which needs thyroid supplements.
- Surgery: Thyroidectomy is another type of treatment option. The possible side effect after surgery is hypothyroidism. Patients need to take thyroid hormone supplements to restore normal hormone levels.
Contraindicated medications
Patients diagnosed with hyperthyroidism should avoid using the following medications:
- Levothyroxine
- Phentermine
If you have been diagnosed with hyperthyroidism, consult your physician before starting or stopping any of these medications.
Where to find medical care for Hyperthyroidism?
Directions to Hospitals Treating Hyperthyroidism
Prevention
- For hyperthyroidism caused by too much iodine ingestion, the method of prevention is decreasing iodine ingestion and a regular check of thyroid hormone levels in the blood.
- For hyperthyroidism caused by over-medicating with synthetic thyroid hormone, giving the appropriate dose to patients and a regular check of thyroid hormone levels in the blood may be important.
What to expect (Outlook/Prognosis)?
Many cases of hyperthyroidism are generally treatable. Prognosis depends on whether or not the patient has severe complications.
Possible Complications
Sources
- http://www.endocrine.niddk.nih.gov/pubs/Hyperthyroidism/
- http://www.nlm.nih.gov/medlineplus/ency/article/000356.htm
Causes
Major causes in humans are:
Other causes of hyperthyroxinemia (high blood levels of thyroid hormones) are not to be confused with true hyperthyroidism and include subacute and other forms of thyroiditis (inflammation) and struma ovarii (a teratoma). Thyrotoxicosis (symptoms caused by hyperthyroxinemia) can occur in both hyperthyroidism and thyroiditis. When it causes acutely increased metabolism, it is sometimes called "thyroid storm", a life-threatening event characterized by tachycardia, hypertension, and fever.
Excess thyroid hormone from pills can also cause hyperthyroidism. Amiodarone, a heart medication, can sometimes cause hyperthyroidism. Hamburger toxicosis is a condition that occurs sporadically and is associated with ground beef contaminated with thyroid hormone.
Postpartum thyroiditis occurs in about 7% of women during the year after they give birth. PPT typically has several phases, the first of which is hyperthyroidism. Many times, the hyperthyroidism corrects itself within weeks or months without any treatment necessary.
Life Threatening Causes
- Adenocarcinoma
- Choriocarcinoma
- Metastatic follicular thyroid cancer
- Pituitary tumor
- Struma ovarii
- Teratoma
- Testicular cancer
- Thyroid adenoma
- Thyroid carcinoma
- Thyroid nodule
- Thyroid tumor
- Thyrotropinoma
- Toxic adenoma
- Toxic thyroid adenoma
- Trophoblastic disease
- Tsh-producing pituitary adenoma
Common Causes
Causes by Organ System
Causes in Alphabetical Order
Calssification
Classification
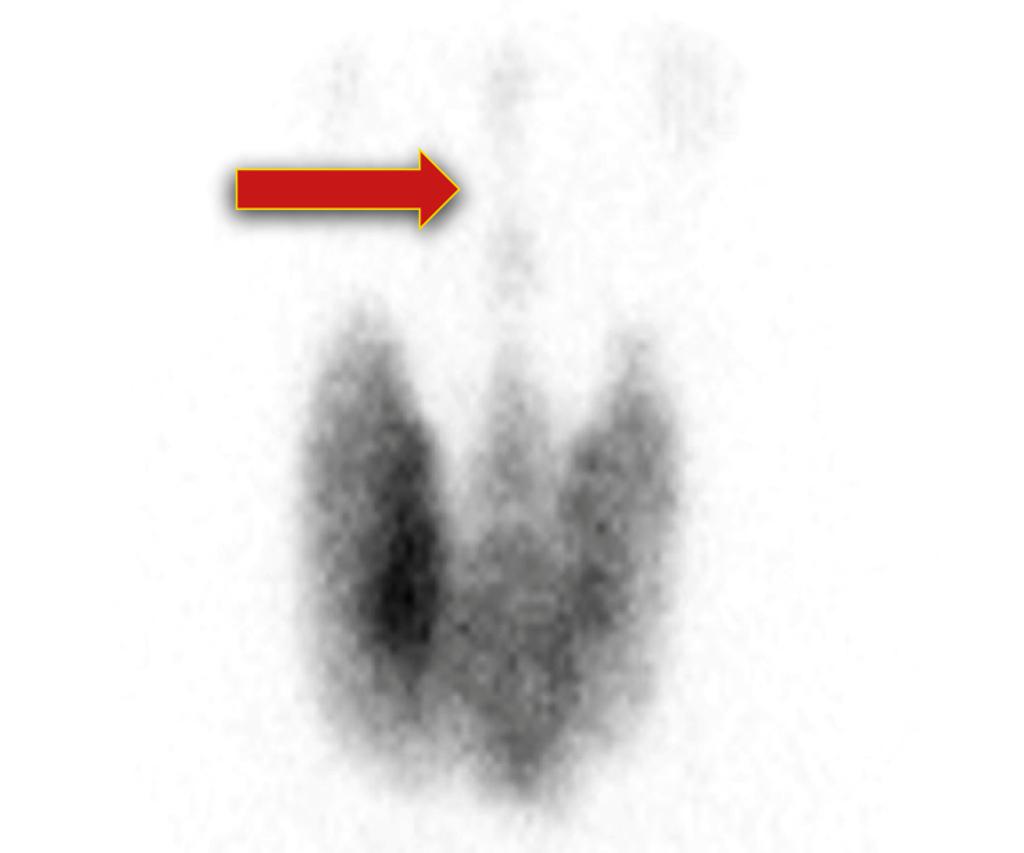
Hyperthyroidism can be classified according to the results of iodine uptake test into:
High iodine uptake
- Grave’s disease
- Toxic multinodular goiter
- Toxic thyroid adenoma
High or normal uptake:
![Normal thyroid scan - Myohan at en.wikipedia [CC BY 3.0 (http://creativecommons.org/licenses/by/3.0)], via Wikimedia Commons](/images/e/e0/Thyroid_scan.jpg) |
- Iodine caused hyperthyroidism
- Hashitoxicosis
- Germ cell tumors (choriocarcinoma in males and testicular germ cell tumors)
- Pituitary TSH-producing adenoma
Low uptake
- Subacute thyroiditis
- Hyperthyroidism due to ectopic thyroid tissue