Thyroid cancer
|
Thyroid Cancer Main Page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Michael Maddaleni, B.S.; Ammu Susheela, M.D. [2]Seyedmahdi Pahlavani, M.D. [3] Sahar Memar Montazerin, M.D.[4]
Overview
Thyroid cancer refers to any of four kinds of tumors of the thyroid gland which include papillary, follicular, medullary and anaplastic tumors. Papillary and follicular tumors are the most common and are usually benign. Papillary and follicular tumors have a slow growth and may recur, but are generally not fatal in patients under 45 years of age. Medullary and anaplastic tumors are malignant. Medullary tumors have a good prognosis if the are restricted to the thyroid gland and a poorer prognosis if metastasis occurs. Anaplastic tumors are fast-growing and respond poorly to therapy. Thyroid nodules are diagnosed by ultrasound guided fine needle aspiration or frequently by thyroidectomy (surgical removal and subsequent histological examination). As the thyroid cancer can uptake iodine, radioactive iodine is commonly used for the treatment of thyroid carcinomas. However, radioactive iodine therapy is accompanied by thyroxine therapy to ensure TSH suppression.
Classification
Thyroid cancers can be classified according to their pathological characteristics. The following variants can be distinguished (distribution over various subtypes may show regional variation):
- Papillary thyroid cancer (75%, including mixed papillary/follicular)
- Follicular thyroid cancer (16%)
- Medullary thyroid cancer (5-7%)
- Anaplastic thyroid cancer (3%)
- Lymphoma (1%)
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Causes
- For more information on papillary thyroid cancer causes, click here.
- For more information on follicular thyroid cancer causes, click here.
- For more information on medullary thyroid cancer causes, click here.
- For more information on anaplastic thyroid cancer causes, click here.
- For more information on primary thyroid lymphoma causes, click here.
Differential diagnosis
Thyroid cancers should be differentiated from one another and from various other diseases:
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | Microscopic Appearance |
|---|---|---|---|---|---|---|---|---|---|
| Papillary Thyroid Cancer[1][2][3] |
|
|
|
|
|
|
|
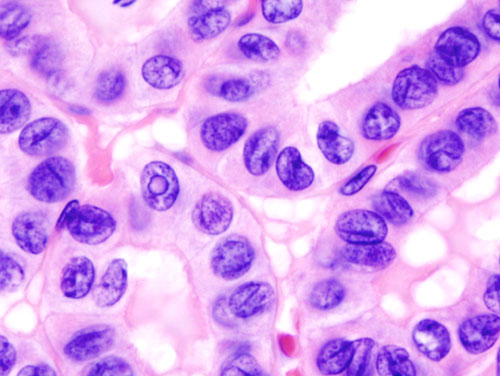 | |
| Follicular Thyroid Cancer[2][3][4] |
|
|
|
|
|
|
|
|
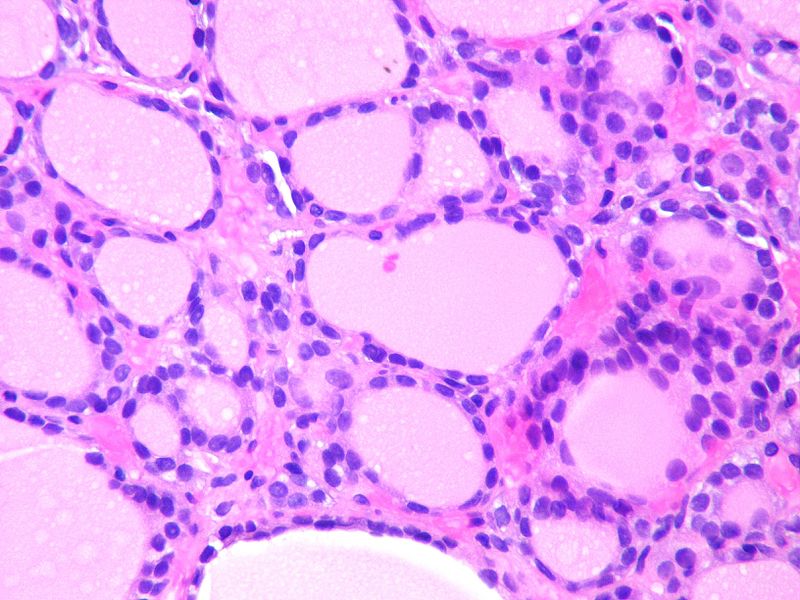 |
| Medullary Thyroid Cancer[5][6][7][3] |
|
|
|
|
|
|
|
 | |
| Anaplastic Thyroid Cancer[8][9][10] |
|
|
|
|
|
|
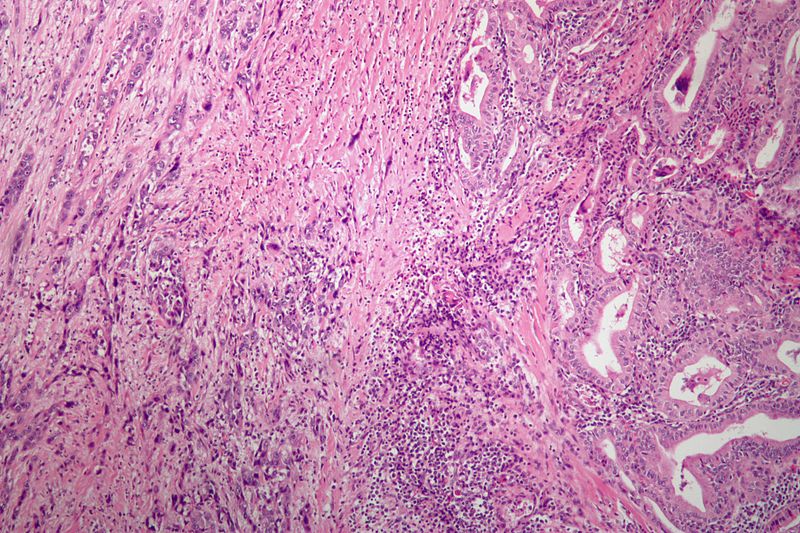 | ||
| Follicular Adenoma[11] |
|
|
|
|
|
|
 | ||
| Multinodular Goiter[12] |
|
|
|
|
|
|
|
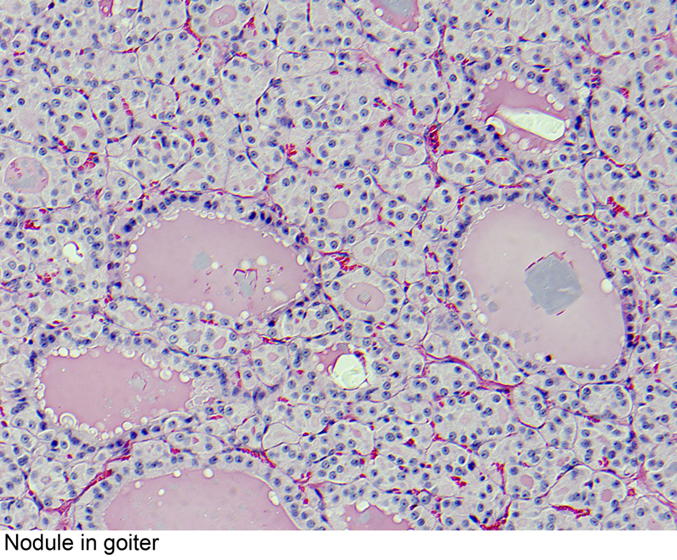 | |
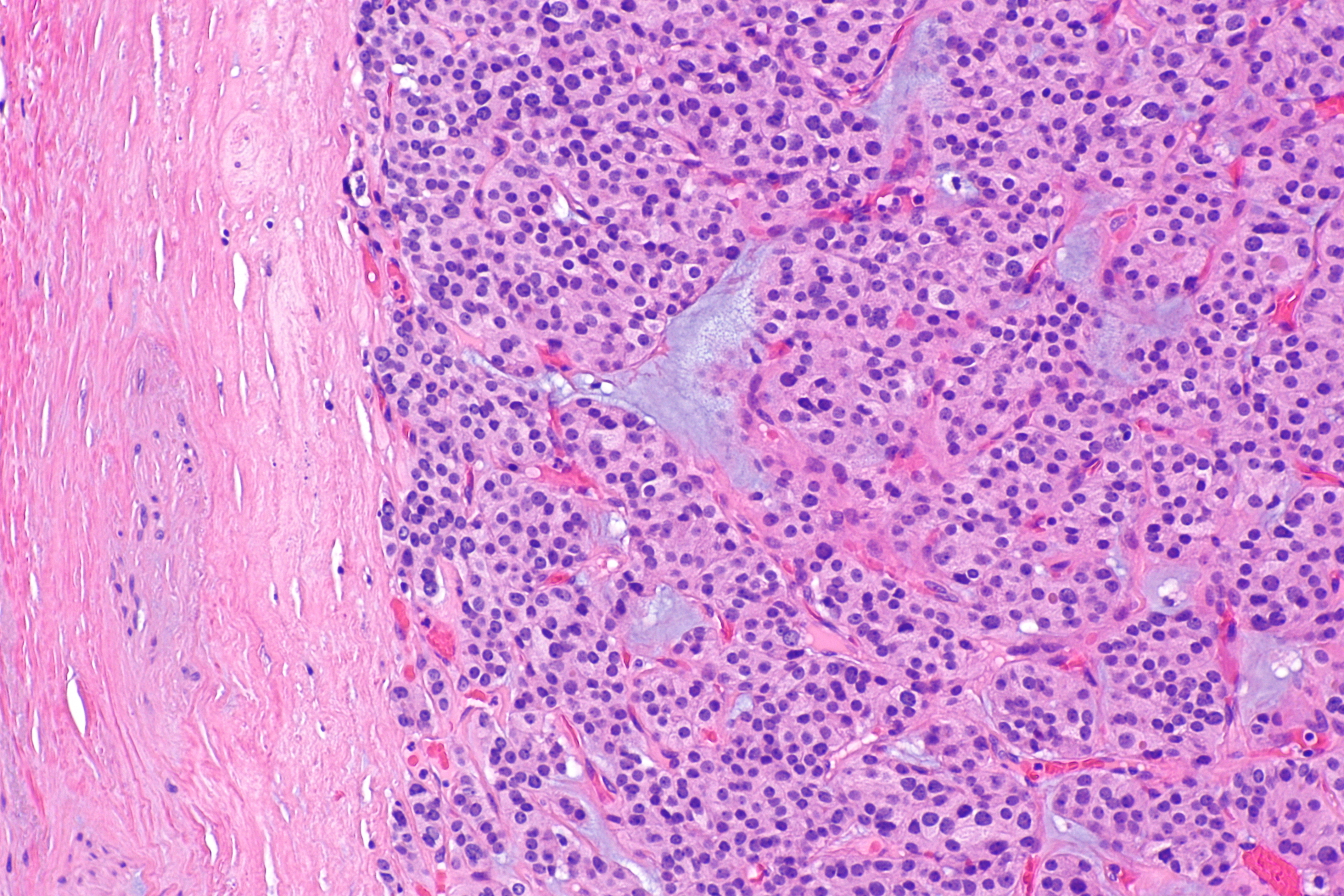
| Thyroid Lymphoma[13] |
|
|
|
|
|
|
|
|
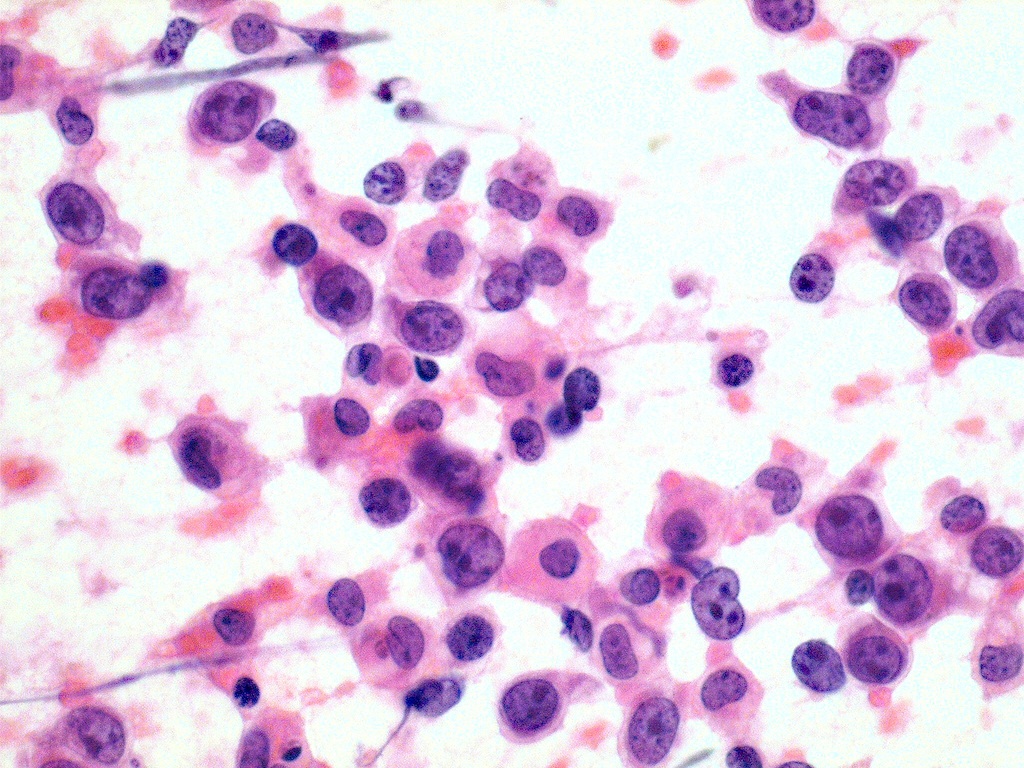 |
References
- ↑ Fagin, James A.; Mitsiades, Nicholas (2008). "Molecular pathology of thyroid cancer: diagnostic and clinical implications". Best Practice & Research Clinical Endocrinology & Metabolism. 22 (6): 955–969. doi:10.1016/j.beem.2008.09.017. ISSN 1521-690X.
- ↑ 2.0 2.1 Schlumberger, Martin Jean (1998). "Papillary and Follicular Thyroid Carcinoma". New England Journal of Medicine. 338 (5): 297–306. doi:10.1056/NEJM199801293380506. ISSN 0028-4793.
- ↑ 3.0 3.1 3.2 Sipos JA (December 2009). "Advances in ultrasound for the diagnosis and management of thyroid cancer". Thyroid. 19 (12): 1363–72. doi:10.1089/thy.2009.1608. PMID 20001718.
- ↑ Pettersson B, Adami HO, Wilander E, Coleman MP (April 1991). "Trends in thyroid cancer incidence in Sweden, 1958-1981, by histopathologic type". Int. J. Cancer. 48 (1): 28–33. doi:10.1002/ijc.2910480106. PMID 2019455.
- ↑ Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E (January 1984). "Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma". Cancer. 53 (2): 278–85. doi:10.1002/1097-0142(19840115)53:2<278::aid-cncr2820530216>3.0.co;2-z. PMID 6690009.
- ↑ Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH (March 2000). "Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems". Cancer. 88 (5): 1139–48. doi:10.1002/(sici)1097-0142(20000301)88:5<1139::aid-cncr26>3.0.co;2-z. PMID 10699905.
- ↑ Hofstra, Robert M. W.; Landsvater, Rudy M.; Ceccherini, Isabella; Stulp, Rein P.; Stelwagen, Tineke; Luo, Yin; Pasini, Barbara; Hoppener, Jo W. M.; van Amstel, Hans Kristian Ploos; Romeo, Giovanni; Lips, Cornells J. M.; Buys, Charles H. C. M. (1994). "A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma". Nature. 367 (6461): 375–376. doi:10.1038/367375a0. ISSN 0028-0836.
- ↑ Nagaiah G, Hossain A, Mooney CJ, Parmentier J, Remick SC (2011). "Anaplastic thyroid cancer: a review of epidemiology, pathogenesis, and treatment". J Oncol. 2011: 542358. doi:10.1155/2011/542358. PMC 3136148. PMID 21772843.
- ↑ Chang TC, Liaw KY, Kuo SH, Chang CC, Chen FW (June 1989). "Anaplastic thyroid carcinoma: review of 24 cases, with emphasis on cytodiagnosis and leukocytosis". Taiwan Yi Xue Hui Za Zhi. 88 (6): 551–6. PMID 2794956.
- ↑ Venkatesh YS, Ordonez NG, Schultz PN, Hickey RC, Goepfert H, Samaan NA (July 1990). "Anaplastic carcinoma of the thyroid. A clinicopathologic study of 121 cases". Cancer. 66 (2): 321–30. doi:10.1002/1097-0142(19900715)66:2<321::aid-cncr2820660221>3.0.co;2-a. PMID 1695118.
- ↑ Mathur, Aarti; Olson, Matthew T.; Zeiger, Martha A. (2014). "Follicular Lesions of the Thyroid". Surgical Clinics of North America. 94 (3): 499–513. doi:10.1016/j.suc.2014.02.005. ISSN 0039-6109.
- ↑ Bronshteĭn ME, Makarov AD, Artemova AM, Bazarova EN, Kozlov GI (1994). "[Morphology of the thyroid tissue in multinodular euthyroid goiter]". Probl Endokrinol (Mosk) (in Russian). 40 (2): 36–9. PMID 8197088.
- ↑ Pedersen RK, Pedersen NT (January 1996). "Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study". Histopathology. 28 (1): 25–32. PMID 8838117.
- ↑ Hyjek E, Isaacson PG (November 1988). "Primary B cell lymphoma of the thyroid and its relationship to Hashimoto's thyroiditis". Hum. Pathol. 19 (11): 1315–26. doi:10.1016/s0046-8177(88)80287-9. PMID 3141260.
- ↑ Tupchong L, Hughes F, Harmer CL (October 1986). "Primary lymphoma of the thyroid: clinical features, prognostic factors, and results of treatment". Int. J. Radiat. Oncol. Biol. Phys. 12 (10): 1813–21. doi:10.1016/0360-3016(86)90324-x. PMID 3759532.
- ↑ Ota H, Ito Y, Matsuzuka F, Kuma S, Fukata S, Morita S, Kobayashi K, Nakamura Y, Kakudo K, Amino N, Miyauchi A (October 2006). "Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid". Thyroid. 16 (10): 983–7. doi:10.1089/thy.2006.16.983. PMID 17042683.