Sacubitril and Valsartan: Difference between revisions
No edit summary |
No edit summary |
||
| (7 intermediate revisions by the same user not shown) | |||
| Line 7: | Line 7: | ||
|indication=of cardiovascular death and hospitalization for [[heart failure]] in patients with [[chronic heart failure]] ([[New york heart association functional classification|NYHA Class]] II-IV) and reduced [[ejection fraction]] | |indication=of cardiovascular death and hospitalization for [[heart failure]] in patients with [[chronic heart failure]] ([[New york heart association functional classification|NYHA Class]] II-IV) and reduced [[ejection fraction]] | ||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions=[[hypotension]], increased | |adverseReactions=[[hypotension]], increased [[serum potassium]], [[hyperkalemia]], and increased [[serum creatinine]] | ||
|blackBoxWarningTitle='''<span style="color:#FF0000;"></span>''' | |blackBoxWarningTitle='''<span style="color:#FF0000;"></span>''' | ||
FETAL TOXICITY | FETAL TOXICITY | ||
| Line 13: | Line 13: | ||
*When pregnancy is detected, discontinue sacubitril and valsartan as soon as possible | *When pregnancy is detected, discontinue sacubitril and valsartan as soon as possible | ||
*Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus | *Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus | ||
|fdaLIADAdult=Sacubitril and [[valsartan]] is indicated to reduce the risk of cardiovascular death and hospitalization for [[heart failure]] in patients with [[chronic heart failure]] ([[New york heart association functional classification|NYHA Class]] II-IV) and reduced ejection fraction. | |fdaLIADAdult=Sacubitril and [[valsartan]] is indicated to reduce the risk of cardiovascular death and hospitalization for [[heart failure]] in patients with [[chronic heart failure]] ([[New york heart association functional classification|NYHA Class]] II-IV) and reduced [[ejection fraction]]. | ||
'''Dosing Information''' | '''Dosing Information''' | ||
*Sacubitril and [[valsartan]] is contraindicated with concomitant use of an angiotensin-converting enzyme (ACE) inhibitor. If switching from an ACE inhibitor to sacubitril and [[valsartan]] allow a washout period of 36 hours between administration of the two drugs. | *Sacubitril and [[valsartan]] is contraindicated with concomitant use of an [[ACE inhibitor|angiotensin-converting enzyme (ACE) inhibitor]]. If switching from an [[ACE inhibitor]] to sacubitril and [[valsartan]], allow a washout period of 36 hours between administration of the two drugs. | ||
*The recommended starting dose of sacubitril and [[valsartan]] is 49/51 mg twice-daily. | *The recommended starting dose of sacubitril and [[valsartan]] is 49/51 mg twice-daily. | ||
*Double the dose of sacubitril and [[valsartan]] after 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | *Double the dose of sacubitril and [[valsartan]] after 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | ||
*Dose Adjustment for Patients Not Taking an ACE inhibitor or [[ARB]] or Previously Taking Low Doses of These Agents | *Dose Adjustment for Patients Not Taking an [[ACE inhibitor]] or [[ARB]] or Previously Taking Low Doses of These Agents | ||
**A starting dose of 24/26 mg twice-daily is recommended for patients not currently taking an ACE inhibitor or an [[angiotensin II receptor blocker]] (ARB) and for patients previously taking low doses of these agents. Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | **A starting dose of 24/26 mg twice-daily is recommended for patients not currently taking an [[ACE inhibitor]] or an [[angiotensin II receptor blocker]] (ARB) and for patients previously taking low doses of these agents. Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | ||
*Dose Adjustment for Severe Renal Impairment | *Dose Adjustment for Severe [[renal impairment|Renal Impairment]] | ||
**A starting dose of 24/26 mg twice-daily is recommended for patients with severe renal impairment (eGFR <30 mL/min/1.73 m2). Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | **A starting dose of 24/26 mg twice-daily is recommended for patients with severe [[renal impairment]] ([[glomerular filtration rate|eGFR]] <30 mL/min/1.73 m2). Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | ||
**No starting dose adjustment is needed for mild or moderate renal impairment. | **No starting dose adjustment is needed for mild or moderate [[renal impairment]]. | ||
*Dose Adjustment for Hepatic Impairment | *Dose Adjustment for [[hepatic impairment|Hepatic Impairment]] | ||
**A starting dose of 24/26 mg twice-daily is recommended for patients with moderate hepatic impairment (Child-Pugh B classification). Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | **A starting dose of 24/26 mg twice-daily is recommended for patients with moderate [[hepatic impairment]] ([[Child-Pugh]] B classification). Double the dose of sacubitril and [[valsartan]] every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient. | ||
**No starting dose adjustment is needed for mild hepatic impairment. | **No starting dose adjustment is needed for mild [[hepatic impairment]]. | ||
**Use in patients with severe hepatic impairment is not recommended. | **Use in patients with severe [[hepatic impairment]] is not recommended. | ||
|offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Sacubitril and [[Valsartan]] in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Sacubitril and [[Valsartan]] in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of Sacubitril and [[Valsartan]] in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of Sacubitril and [[Valsartan]] in adult patients. | ||
| Line 35: | Line 35: | ||
|contraindications=Sacubitril and [[valsartan]] is contraindicated: | |contraindications=Sacubitril and [[valsartan]] is contraindicated: | ||
*In patients with [[hypersensitivity]] to any component. | *In patients with [[hypersensitivity]] to any component. | ||
*In patients with a history of angioedema related to previous ACE inhibitor or [[ARB]] therapy. | *In patients with a history of [[angioedema]] related to previous [[ACE inhibitor]] or [[ARB]] therapy. | ||
*With concomitant use of ACE inhibitors. Do not administer within 36 hours of switching from or to an ACE inhibitor. | *With concomitant use of [[ACE inhibitor|ACE inhibitors]]. Do not administer within 36 hours of switching from or to an [[ACE inhibitor]]. | ||
*With concomitant use of [[aliskiren]] in patients with [[diabetes]]. | *With concomitant use of [[aliskiren]] in patients with [[diabetes]]. | ||
|warnings=*Fetal Toxicity | |warnings=*Fetal Toxicity | ||
**Sacubitril and [[valsartan]] can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. | **Sacubitril and [[valsartan]] can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the [[renin-angiotensin system]] during the second and third trimesters of pregnancy reduces fetal [[renal function]] and increases fetal and neonatal morbidity and death. | ||
**When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and [[valsartan]]. However, if there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system, and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus. | **When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and [[valsartan]]. However, if there is no appropriate alternative to therapy with drugs affecting the [[renin-angiotensin system]], and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus. | ||
*[[Angioedema]] | *[[Angioedema]] | ||
**Sacubitril and [[valsartan]] may cause angioedema. In the double-blind period of PARADIGM-HF, 0.5% of patients treated with sacubitril and [[valsartan]] and 0.2% of patients treated with enalapril had angioedema. | **Sacubitril and [[valsartan]] may cause [[angioedema]]. In the double-blind period of PARADIGM-HF, 0.5% of patients treated with sacubitril and [[valsartan]] and 0.2% of patients treated with [[enalapril]] had [[angioedema]]. | ||
**If angioedema occurs, discontinue sacubitril and [[valsartan]] immediately, provide appropriate therapy, and monitor for airway compromise. Sacubitril and [[valsartan]] must not be re-administered. In cases of confirmed angioedema where swelling has been confined to the face and lips, the condition has generally resolved without treatment, although antihistamines have been useful in relieving symptoms. | **If [[angioedema]] occurs, discontinue sacubitril and [[valsartan]] immediately, provide appropriate therapy, and monitor for airway compromise. Sacubitril and [[valsartan]] must not be re-administered. In cases of confirmed [[angioedema]] where [[swelling]] has been confined to the face and lips, the condition has generally resolved without treatment, although [[antihistamine|antihistamines]] have been useful in relieving symptoms. | ||
**Angioedema associated with laryngeal edema may be fatal. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, administer appropriate therapy, e.g., subcutaneous epinephrine/adrenaline solution 1:1000 (0.3 mL to 0.5 mL) and take measures necessary to ensure maintenance of a patent airway. | **[[Angioedema]] associated with [[laryngeal edema]] may be fatal. Where there is involvement of the [[tongue]], [[glottis]] or [[larynx]], likely to cause airway obstruction, administer appropriate therapy, e.g., [[subcutaneous]] [[Epinephrine (injection)|epinephrine/adrenaline]] solution 1:1000 (0.3 mL to 0.5 mL) and take measures necessary to ensure maintenance of a patent airway. | ||
**Sacubitril and [[valsartan]] has been associated with a higher rate of angioedema in Black than in non-Black patients. | **Sacubitril and [[valsartan]] has been associated with a higher rate of [[angioedema]] in Black than in non-Black patients. | ||
**Patients with a prior history of angioedema may be at increased risk of angioedema with sacubitril and [[valsartan]]. Sacubitril and [[valsartan]] should not be used in patients with a known history of angioedema related to previous ACE inhibitor or [[ARB]] therapy. | **Patients with a prior history of [[angioedema]] may be at increased risk of [[angioedema]] with sacubitril and [[valsartan]]. Sacubitril and [[valsartan]] should not be used in patients with a known history of [[angioedema]] related to previous [[ACE inhibitor]] or [[ARB]] therapy. | ||
*[[Hypotension]] | *[[Hypotension]] | ||
**Sacubitril and [[valsartan]] lowers blood pressure and may cause symptomatic hypotension. Patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics), are at greater risk. In the double-blind period of PARADIGM-HF, 18% of patients treated with sacubitril and [[valsartan]] and 12% of patients treated with enalapril reported hypotension as an adverse event, with hypotension reported as a serious adverse event in approximately 1.5% of patients in both treatment arms. | **Sacubitril and [[valsartan]] lowers [[blood pressure]] and may cause symptomatic [[hypotension]]. Patients with an activated [[renin-angiotensin system]], such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of [[diuretics]]), are at greater risk. In the double-blind period of PARADIGM-HF, 18% of patients treated with sacubitril and [[valsartan]] and 12% of patients treated with [[enalapril]] reported [[hypotension]] as an adverse event, with [[hypotension]] reported as a serious adverse event in approximately 1.5% of patients in both treatment arms. | ||
**Correct volume or salt depletion prior to administration of sacubitril and [[valsartan]] or start at a lower dose. If hypotension occurs, consider dose adjustment of diuretics, concomitant antihypertensive drugs, and treatment of other causes of hypotension (e.g., hypovolemia). If hypotension persists despite such measures, reduce the dosage or temporarily discontinue sacubitril and [[valsartan]]. Permanent discontinuation of therapy is usually not required. | **Correct volume or salt depletion prior to administration of sacubitril and [[valsartan]] or start at a lower dose. If [[hypotension]] occurs, consider dose adjustment of [[diuretics]], concomitant [[antihypertensive]] drugs, and treatment of other causes of [[hypotension]] (e.g., [[hypovolemia]]). If [[hypotension]] persists despite such measures, reduce the dosage or temporarily discontinue sacubitril and [[valsartan]]. Permanent discontinuation of therapy is usually not required. | ||
*Impaired Renal Function | *Impaired [[renal function|Renal Function]] | ||
**As a consequence of inhibiting the renin-angiotensin-aldosterone system (RAAS), decreases in renal function may be anticipated in susceptible individuals treated with sacubitril and [[valsartan]]. In the double-blind period of PARADIGM-HF, 5% of patients in both the sacubitril and [[valsartan]] and enalapril groups reported renal failure as an adverse event. | **As a consequence of inhibiting the [[renin-angiotensin-aldosterone system]] (RAAS), decreases in [[renal function]] may be anticipated in susceptible individuals treated with sacubitril and [[valsartan]]. In the double-blind period of PARADIGM-HF, 5% of patients in both the sacubitril and [[valsartan]] and [[enalapril]] groups reported [[renal failure]] as an adverse event. | ||
**In patients whose renal function depends upon the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe [[congestive heart failure]]), treatment with ACE inhibitors and angiotensin receptor antagonists has been associated with oliguria, progressive azotemia and, rarely, acute renal failure and death. | **In patients whose [[renal function]] depends upon the activity of the [[renin-angiotensin-aldosterone system]] (e.g., patients with severe [[congestive heart failure]]), treatment with [[ACE inhibitor|ACE inhibitors]] and [[Angiotensin II receptor antagonist|angiotensin receptor antagonists]] has been associated with [[oliguria]], progressive [[azotemia]] and, rarely, [[acute renal failure]] and death. | ||
**Closely monitor serum creatinine, and down-titrate or interrupt sacubitril and [[valsartan]] in patients who develop a clinically significant decrease in renal function. | **Closely monitor [[serum creatinine]], and down-titrate or interrupt sacubitril and [[valsartan]] in patients who develop a clinically significant decrease in [[renal function]]. | ||
**As with all drugs that affect the RAAS, sacubitril and [[valsartan]] may increase blood urea and serum creatinine levels in patients with bilateral or unilateral renal artery stenosis. In patients with renal artery stenosis, monitor renal function. | **As with all drugs that affect the [[RAAS]], sacubitril and [[valsartan]] may increase [[blood urea nitrogen|blood urea]] and [[serum creatinine]] levels in patients with bilateral or unilateral [[renal artery stenosis]]. In patients with [[renal artery stenosis]], monitor [[renal function]]. | ||
*[[Hyperkalemia]] | *[[Hyperkalemia]] | ||
**Through its actions on the RAAS, hyperkalemia may occur with sacubitril and [[valsartan]]. In the double-blind period of PARADIGM-HF, 12% of patients treated with sacubitril and [[valsartan]] and 14% of patients treated with enalapril reported hyperkalemia as an adverse event. | **Through its actions on the [[RAAS]], [[hyperkalemia]] may occur with sacubitril and [[valsartan]]. In the double-blind period of PARADIGM-HF, 12% of patients treated with sacubitril and [[valsartan]] and 14% of patients treated with [[enalapril]] reported [[hyperkalemia]] as an adverse event. | ||
**Monitor serum potassium periodically and treat appropriately, especially in patients with risk factors for hyperkalemia such as severe renal impairment, diabetes, hypoaldosteronism, or a high potassium diet. Dosage reduction or interruption of sacubitril and [[valsartan]] may be required. | **Monitor [[serum potassium]] periodically and treat appropriately, especially in patients with risk factors for [[hyperkalemia]] such as severe [[renal impairment]], [[diabetes]], [[hypoaldosteronism]], or a high [[potassium]] diet. Dosage reduction or interruption of sacubitril and [[valsartan]] may be required. | ||
|clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | ||
In the PARADIGM-HF trial, subjects were required to complete sequential enalapril and sacubitril and [[valsartan]] run-in periods of (median) 15 and 29 days, respectively, prior to entering the randomized double-blind period comparing sacubitril and [[valsartan]] and enalapril. During the enalapril run-in period, 1,102 patients (10.5%) were permanently discontinued from the study, 5.6% because of an adverse event, most commonly renal dysfunction (1.7%), hyperkalemia (1.7%) and hypotension (1.4%). During the sacubitril and [[valsartan]] run-in period, an additional 10.4% of patients permanently discontinued treatment, 5.9% because of an adverse event, most commonly renal dysfunction (1.8%), hypotension (1.7%) and hyperkalemia (1.3%). Because of this run-in design, the adverse reaction rates described below are lower than expected in practice. | In the PARADIGM-HF trial, subjects were required to complete sequential [[enalapril]] and sacubitril and [[valsartan]] run-in periods of (median) 15 and 29 days, respectively, prior to entering the randomized double-blind period comparing sacubitril and [[valsartan]] and [[enalapril]]. During the [[enalapril]] run-in period, 1,102 patients (10.5%) were permanently discontinued from the study, 5.6% because of an adverse event, most commonly [[renal dysfunction]] (1.7%), [[hyperkalemia]] (1.7%) and [[hypotension]] (1.4%). During the sacubitril and [[valsartan]] run-in period, an additional 10.4% of patients permanently discontinued treatment, 5.9% because of an adverse event, most commonly [[renal dysfunction]] (1.8%), [[hypotension]] (1.7%) and [[hyperkalemia]] (1.3%). Because of this run-in design, the adverse reaction rates described below are lower than expected in practice. | ||
In the double-blind period, safety was evaluated in 4,203 patients treated with sacubitril and [[valsartan]] and 4,229 treated with enalapril. In PARADIGM-HF, patients randomized to sacubitril and [[valsartan]] received treatment for up to 4.3 years, with a median duration of exposure of 24 months; 3,271 patients were treated for more than one year. Discontinuation of therapy because of an adverse event during the double-blind period occurred in 450 (10.7%) of sacubitril and [[valsartan]] treated patients and 516 (12.2%) of patients receiving enalapril. | In the double-blind period, safety was evaluated in 4,203 patients treated with sacubitril and [[valsartan]] and 4,229 treated with [[enalapril]]. In PARADIGM-HF, patients randomized to sacubitril and [[valsartan]] received treatment for up to 4.3 years, with a median duration of exposure of 24 months; 3,271 patients were treated for more than one year. Discontinuation of therapy because of an adverse event during the double-blind period occurred in 450 (10.7%) of sacubitril and [[valsartan]] treated patients and 516 (12.2%) of patients receiving [[enalapril]]. | ||
Adverse reactions occurring at an incidence of ≥5% in patients who were treated with sacubitril and [[valsartan]] in the double-blind period are shown in Table 1. | Adverse reactions occurring at an incidence of ≥5% in patients who were treated with sacubitril and [[valsartan]] in the double-blind period are shown in Table 1. | ||
| Line 68: | Line 68: | ||
[[File: Sacubitril and Valsartan T1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File: Sacubitril and Valsartan T1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
In the PARADIGM-HF trial, the incidence of angioedema was 0.1% in both the enalapril and sacubitril and [[valsartan]] run-in periods. In the double-blind period, the incidence of angioedema was higher in patients treated with sacubitril and [[valsartan]] than enalapril (0.5% and 0.2%, respectively). The incidence of angioedema in Black patients was 2.4% with sacubitril and [[valsartan]] and 0.5% with enalapril. | In the PARADIGM-HF trial, the incidence of [[angioedema]] was 0.1% in both the [[enalapril]] and sacubitril and [[valsartan]] run-in periods. In the double-blind period, the incidence of [[angioedema]] was higher in patients treated with sacubitril and [[valsartan]] than [[enalapril]] (0.5% and 0.2%, respectively). The incidence of [[angioedema]] in Black patients was 2.4% with sacubitril and [[valsartan]] and 0.5% with [[enalapril]]. | ||
Orthostasis was reported in 2.1% of patients treated with sacubitril and [[valsartan]] compared to 1.1% of patients treated with enalapril during the double-blind period of PARADIGM-HF. Falls were reported in 1.9% of patients treated with sacubitril and [[valsartan]] compared to 1.3% of patients treated with enalapril. | [[Orthostasis]] was reported in 2.1% of patients treated with sacubitril and [[valsartan]] compared to 1.1% of patients treated with [[enalapril]] during the double-blind period of PARADIGM-HF. Falls were reported in 1.9% of patients treated with sacubitril and [[valsartan]] compared to 1.3% of patients treated with [[enalapril]]. | ||
Laboratory Abnormalities: | Laboratory Abnormalities: | ||
*Hemoglobin and Hematocrit | *[[Hemoglobin]] and [[Hematocrit]] | ||
**Decreases in hemoglobin/hematocrit of >20% were observed in approximately 5% of both sacubitril and [[valsartan]]- and enalapril-treated patients in the double-blind period in PARADIGM-HF. | **Decreases in [[hemoglobin]]/[[hematocrit]] of >20% were observed in approximately 5% of both sacubitril and [[valsartan]]- and [[enalapril]]-treated patients in the double-blind period in PARADIGM-HF. | ||
*Serum Creatinine | *[[serum creatinine|Serum Creatinine]] | ||
**Increases in serum creatinine of >50% were observed in 1.4% of patients in the enalapril run-in period and 2.2% of patients in the sacubitril and [[valsartan]] run-in period. During the double-blind period, approximately 16% of both sacubitril and [[valsartan]]- and enalapril-treated patients had increases in serum creatinine of >50%. | **Increases in [[serum creatinine]] of >50% were observed in 1.4% of patients in the [[enalapril]] run-in period and 2.2% of patients in the sacubitril and [[valsartan]] run-in period. During the double-blind period, approximately 16% of both sacubitril and [[valsartan]]- and [[enalapril]]-treated patients had increases in [[serum creatinine]] of >50%. | ||
*Serum Potassium | *[[serum potassium|Serum Potassium]] | ||
**Potassium concentrations >5.5 mEq/L were observed in approximately 4% of patients in both the enalapril and sacubitril and [[valsartan]] run-in periods. During the double-blind period, approximately 16% of both sacubitril and [[valsartan]]- and enalapril-treated patients had potassium concentrations >5.5 mEq/L. | **[[Potassium]] concentrations >5.5 mEq/L were observed in approximately 4% of patients in both the [[enalapril]] and sacubitril and [[valsartan]] run-in periods. During the double-blind period, approximately 16% of both sacubitril and [[valsartan]]- and [[enalapril]]-treated patients had [[potassium]] concentrations >5.5 mEq/L. | ||
|drugInteractions=*Dual Blockade of the Renin-Angiotensin-Aldosterone System | |drugInteractions=*Dual Blockade of the [[renin-angiotensin-aldosterone system|Renin-Angiotensin-Aldosterone System]] | ||
**Concomitant use of sacubitril and [[valsartan]] with an ACE inhibitor is contraindicated because of the increased risk of angioedema. | **Concomitant use of sacubitril and [[valsartan]] with an [[ACE inhibitor]] is contraindicated because of the increased risk of [[angioedema]]. | ||
**Avoid use of sacubitril and [[valsartan]] with an [[ARB]], because sacubitril and [[valsartan]] contains the [[angiotensin II receptor blocker]] [[valsartan]]. | **Avoid use of sacubitril and [[valsartan]] with an [[ARB]], because sacubitril and [[valsartan]] contains the [[angiotensin II receptor blocker]] [[valsartan]]. | ||
**The concomitant use of sacubitril and [[valsartan]] with aliskiren is contraindicated in patients with diabetes. Avoid use with aliskiren in patients with renal impairment (eGFR <60 mL/min/1.73 m2). | **The concomitant use of sacubitril and [[valsartan]] with [[aliskiren]] is contraindicated in patients with [[diabetes]]. Avoid use with [[aliskiren]] in patients with [[renal impairment]] ([[glomerular filtration rate|eGFR]] <60 mL/min/1.73 m2). | ||
*Potassium-Sparing Diuretics | *[[potassium-sparing diuretic|Potassium-Sparing Diuretics]] | ||
**As with other drugs that block angiotensin II or its effects, concomitant use of potassium-sparing diuretics (e.g., spironolactone, triamterene, amiloride), potassium supplements, or salt substitutes containing potassium may lead to increases in serum potassium. | **As with other drugs that block [[angiotensin II]] or its effects, concomitant use of [[potassium-sparing diuretics]] (e.g., [[spironolactone]], [[triamterene]], [[amiloride]]), [[potassium]] supplements, or salt substitutes containing [[potassium]] may lead to increases in [[serum potassium]]. | ||
*Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors) | *[[NSAIDs|Nonsteroidal Anti-Inflammatory Drugs]] (NSAIDs) Including [[COX-2 inhibitor|Selective Cyclooxygenase-2 Inhibitors]] (COX-2 Inhibitors) | ||
**In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, concomitant use of NSAIDs, including COX-2 inhibitors, with sacubitril and [[valsartan]] may result in worsening of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically. | **In patients who are elderly, volume-depleted (including those on [[diuretic]] therapy), or with compromised [[renal function]], concomitant use of [[NSAIDs]], including [[COX-2 inhibitor|COX-2 inhibitors]], with sacubitril and [[valsartan]] may result in worsening of [[renal function]], including possible [[acute renal failure]]. These effects are usually reversible. Monitor [[renal function]] periodically. | ||
*[[Lithium]] | *[[Lithium]] | ||
**Increases in serum lithium concentrations and lithium toxicity have been reported during concomitant administration of lithium with angiotensin II receptor antagonists. Monitor serum lithium levels during concomitant use with sacubitril and [[valsartan]]. | **Increases in serum [[lithium]] concentrations and [[lithium]] toxicity have been reported during concomitant administration of [[lithium]] with [[angiotensin II receptor antagonists]]. Monitor serum [[lithium]] levels during concomitant use with sacubitril and [[valsartan]]. | ||
|useInPregnancyFDA=*Risk Summary | |useInPregnancyFDA=*Risk Summary | ||
**Sacubitril and [[valsartan]] can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. | **Sacubitril and [[valsartan]] can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the [[renin-angiotensin system]] during the second and third trimesters of pregnancy reduces fetal [[renal function]] and increases fetal and neonatal morbidity and death. | ||
**Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. In animal reproduction studies, sacubitril and [[valsartan]] treatment during organogenesis resulted in increased embryo-fetal lethality in rats and rabbits and teratogenicity in rabbits. | **Most epidemiologic studies examining fetal abnormalities after exposure to [[antihypertensive]] use in the first trimester have not distinguished drugs affecting the [[renin-angiotensin system]] from other [[antihypertensive]] agents. In animal reproduction studies, sacubitril and [[valsartan]] treatment during [[organogenesis]] resulted in increased embryo-fetal lethality in rats and rabbits and [[teratogenicity]] in rabbits. | ||
**When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and [[valsartan]]. However, if there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system, and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus. | **When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and [[valsartan]]. However, if there is no appropriate alternative to therapy with drugs affecting the [[renin-angiotensin system]], and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus. | ||
**The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. | **The estimated background risk of major [[birth defects]] and [[miscarriage]] for the indicated population is unknown. In the U.S. general population, the estimated background risk of major [[birth defects]] and [[miscarriage]] in clinically recognized pregnancies is 2-4% and 15-20%, respectively. | ||
*Clinical Considerations | *Clinical Considerations | ||
**Fetal/Neonatal Adverse Reactions | **Fetal/Neonatal Adverse Reactions | ||
***Oligohydramnios in pregnant women who use drugs affecting the renin-angiotensin system in the second and third trimesters of pregnancy can result in the following: reduced fetal renal function leading to anuria and renal failure, fetal lung hypoplasia, skeletal deformations, including skull hypoplasia, hypotension, and death. | ***[[Oligohydramnios]] in pregnant women who use drugs affecting the [[renin-angiotensin system]] in the second and third trimesters of pregnancy can result in the following: reduced fetal [[renal function]] leading to [[anuria]] and [[renal failure]], fetal lung [[hypoplasia]], skeletal deformations, including skull [[hypoplasia]], [[hypotension]], and death. | ||
***Perform serial ultrasound examinations to assess the intra-amniotic environment. Fetal testing may be appropriate, based on the week of gestation. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. If oligohydramnios is observed, consider alternative drug treatment. | ***Perform serial [[ultrasound]] examinations to assess the [[amniotic sac|intra-amniotic environment]]. Fetal testing may be appropriate, based on the week of gestation. Patients and physicians should be aware, however, that [[oligohydramnios]] may not appear until after the fetus has sustained irreversible injury. If [[oligohydramnios]] is observed, consider alternative drug treatment. | ||
***Closely observe neonates with histories of in utero exposure to sacubitril and [[valsartan]] for hypotension, oliguria, and hyperkalemia. In neonates with a history of in utero exposure to sacubitril and [[valsartan]], if oliguria or hypotension occurs, support blood pressure and renal perfusion. Exchange transfusions or dialysis may be required as a means of reversing hypotension and replacing renal function. | ***Closely observe neonates with histories of in utero exposure to sacubitril and [[valsartan]] for [[hypotension]], [[oliguria]], and [[hyperkalemia]]. In neonates with a history of in utero exposure to sacubitril and [[valsartan]], if [[oliguria]] or [[hypotension]] occurs, support [[blood pressure]] and renal [[perfusion]]. Exchange transfusions or [[dialysis]] may be required as a means of reversing [[hypotension]] and replacing [[renal function]]. | ||
*Data | *Data | ||
**Animal data | **Animal data | ||
***Sacubitril and [[valsartan]] treatment during organogenesis resulted in increased embryo-fetal lethality in rats at doses ≥ 49 mg sacubitril/51 mg [[valsartan]]/kg/day (≤ 0.14 [LBQ657, the active metabolite] and 1.5 [valsartan]-fold the maximum recommended human dose [MRHD] of 97/103 mg twice-daily on the basis of the area under the plasma drug concentration-time curve [AUC]) and rabbits at doses ≥ 5 mg sacubitril/5 mg [[valsartan]]/kg/day (4-fold and 0.06-fold the MRHD on the basis of [[valsartan]] and LBQ657 AUC, respectively). | ***Sacubitril and [[valsartan]] treatment during [[organogenesis]] resulted in increased embryo-fetal lethality in rats at doses ≥ 49 mg sacubitril/51 mg [[valsartan]]/kg/day (≤ 0.14 [LBQ657, the active [[metabolite]]] and 1.5 [valsartan]-fold the maximum recommended human dose [MRHD] of 97/103 mg twice-daily on the basis of the area under the [[AUC|plasma drug concentration-time curve]] [AUC]) and rabbits at doses ≥ 5 mg sacubitril/5 mg [[valsartan]]/kg/day (4-fold and 0.06-fold the MRHD on the basis of [[valsartan]] and LBQ657 [[AUC]], respectively). | ||
***Sacubitril and [[valsartan]] is teratogenic based on a low incidence of fetal hydrocephaly, associated with maternally toxic doses, which was observed in rabbits at an sacubitril and [[valsartan]] dose of ≥ 5 mg sacubitril/5 mg [[valsartan]]/kg/day. The adverse embryo-fetal effects of sacubitril and [[valsartan]] are attributed to the angiotensin receptor antagonist activity. | ***Sacubitril and [[valsartan]] is [[teratogenic]] based on a low incidence of fetal [[hydrocephaly]], associated with maternally toxic doses, which was observed in rabbits at an sacubitril and [[valsartan]] dose of ≥ 5 mg sacubitril/5 mg [[valsartan]]/kg/day. The adverse embryo-fetal effects of sacubitril and [[valsartan]] are attributed to the [[Angiotensin II receptor antagonist|angiotensin receptor antagonist]] activity. | ||
***Pre- and postnatal development studies in rats at sacubitril doses up to 750 mg/kg/day (4.5-fold the MRHD on the basis of LBQ657 AUC) and [[valsartan]] at doses up to 600 mg/kg/day (0.86-fold the MRHD on the basis of AUC) indicate that treatment with sacubitril and [[valsartan]] during organogenesis, gestation and lactation may affect pup development and survival. | ***Pre- and postnatal development studies in rats at sacubitril doses up to 750 mg/kg/day (4.5-fold the MRHD on the basis of LBQ657 [[AUC]]) and [[valsartan]] at doses up to 600 mg/kg/day (0.86-fold the MRHD on the basis of [[AUC]]) indicate that treatment with sacubitril and [[valsartan]] during [[organogenesis]], gestation and lactation may affect pup development and survival. | ||
|useInNursing=*Risk Summary | |useInNursing=*Risk Summary | ||
**There is no information regarding the presence of sacubitril/valsartan in human milk, the effects on the breastfed infant, or the effects on milk production. Sacubitril/valsartan is present in rat milk. Because of the potential for serious adverse reactions in breastfed infants from exposure to sacubitril/valsartan, advise a nursing woman that breastfeeding is not recommended during treatment with sacubitril and [[valsartan]]. | **There is no information regarding the presence of sacubitril/valsartan in human milk, the effects on the breastfed infant, or the effects on milk production. Sacubitril/valsartan is present in rat milk. Because of the potential for serious adverse reactions in breastfed infants from exposure to sacubitril/valsartan, advise a nursing woman that breastfeeding is not recommended during treatment with sacubitril and [[valsartan]]. | ||
| Line 110: | Line 110: | ||
|useInPed=Safety and effectiveness in pediatric patients have not been established. | |useInPed=Safety and effectiveness in pediatric patients have not been established. | ||
|useInGeri=No relevant pharmacokinetic differences have been observed in elderly (≥65 years) or very elderly (≥75 years) patients compared to the overall population. | |useInGeri=No relevant pharmacokinetic differences have been observed in elderly (≥65 years) or very elderly (≥75 years) patients compared to the overall population. | ||
|useInRenalImpair=No dose adjustment is required in patients with mild (eGFR 60 to 90 mL/min/1.73 m2) to moderate (eGFR 30 to 60 mL/min/1.73 m2) renal impairment. The recommended starting dose in patients with severe renal impairment (eGFR <30 mL/min/1.73 m2) is 24/26 mg twice daily. | |useInRenalImpair=No dose adjustment is required in patients with mild ([[glomerular filtration rate|eGFR]] 60 to 90 mL/min/1.73 m2) to moderate ([[glomerular filtration rate|eGFR]] 30 to 60 mL/min/1.73 m2) [[renal impairment]]. The recommended starting dose in patients with severe [[renal impairment]] ([[glomerular filtration rate|eGFR]] <30 mL/min/1.73 m2) is 24/26 mg twice daily. | ||
|useInHepaticImpair=No dose adjustment is required when administering sacubitril and [[valsartan]] to patients with mild hepatic impairment (Child-Pugh A classification). The recommended starting dose in patients with moderate hepatic impairment (Child-Pugh B classification) is 24/26 mg twice daily. The use of sacubitril and [[valsartan]] in patients with severe hepatic impairment (Child-Pugh C classification) is not recommended, as no studies have been conducted in these patients. | |useInHepaticImpair=No dose adjustment is required when administering sacubitril and [[valsartan]] to patients with mild [[hepatic impairment]] ([[Child-Pugh]] A classification). The recommended starting dose in patients with moderate [[hepatic impairment]] ([[Child-Pugh]] B classification) is 24/26 mg twice daily. The use of sacubitril and [[valsartan]] in patients with severe [[hepatic impairment]] ([[Child-Pugh]] C classification) is not recommended, as no studies have been conducted in these patients. | ||
|administration=Sacubitril and [[valsartan]] is contraindicated with concomitant use of an angiotensin-converting enzyme (ACE) inhibitor. If switching from an ACE inhibitor to sacubitril and [[valsartan]] allow a washout period of 36 hours between administration of the two drugs. | |administration=Sacubitril and [[valsartan]] is contraindicated with concomitant use of an [[ACE inhibitor|angiotensin-converting enzyme (ACE) inhibitor]]. If switching from an [[ACE inhibitor]] to sacubitril and [[valsartan]], allow a washout period of 36 hours between administration of the two drugs. | ||
|overdose=Limited data are available with regard to overdosage in human subjects with sacubitril and [[valsartan]]. In healthy volunteers, a single dose of sacubitril and [[valsartan]] 583 mg sacubitril/617 mg [[valsartan]], and multiple doses of 437 mg sacubitril/463 mg [[valsartan]] (14 days) have been studied and were well tolerated. | |overdose=Limited data are available with regard to overdosage in human subjects with sacubitril and [[valsartan]]. In healthy volunteers, a single dose of sacubitril and [[valsartan]] 583 mg sacubitril/617 mg [[valsartan]], and multiple doses of 437 mg sacubitril/463 mg [[valsartan]] (14 days) have been studied and were well tolerated. | ||
[[Hypotension]] is the most likely result of overdosage due to the blood pressure lowering effects of sacubitril and [[valsartan]]. Symptomatic treatment should be provided. | [[Hypotension]] is the most likely result of overdosage due to the [[blood pressure]] lowering effects of sacubitril and [[valsartan]]. Symptomatic treatment should be provided. | ||
Sacubitril and [[valsartan]] is unlikely to be removed by [[hemodialysis]] because of high protein binding. | Sacubitril and [[valsartan]] is unlikely to be removed by [[hemodialysis]] because of high protein binding. | ||
|drugBox=[[File:Sacubitril drugbox.JPG|thumb|none|400px]] | |drugBox=[[File:Sacubitril drugbox.JPG|thumb|none|400px]] | ||
[[File:Valsartan drugbox.JPG|thumb|none|400px]] | [[File:Valsartan drugbox.JPG|thumb|none|400px]] | ||
|mechAction=Sacubitril and [[valsartan]] contains a [[neprilysin]] inhibitor, sacubitril, and an angiotensin receptor blocker, [[valsartan]]. Sacubitril and [[valsartan]] inhibits [[neprilysin]] (neutral endopeptidase; NEP) via LBQ657, the active metabolite of the prodrug sacubitril, and blocks the angiotensin II type-1 (AT1) receptor via [[valsartan]]. The cardiovascular and renal effects of sacubitril and [[valsartan]] in [[heart failure]] patients are attributed to the increased levels of peptides that are degraded by [[neprilysin]], such as natriuretic peptides, by LBQ657, and the simultaneous inhibition of the effects of angiotensin II by valsartan. Valsartan inhibits the effects of angiotensin II by selectively blocking the AT1 receptor, and also inhibits angiotensin II-dependent aldosterone release. | |mechAction=Sacubitril and [[valsartan]] contains a [[neprilysin]] inhibitor, sacubitril, and an [[Angiotensin II receptor antagonist|angiotensin receptor blocker]], [[valsartan]]. Sacubitril and [[valsartan]] inhibits [[neprilysin]] (neutral endopeptidase; NEP) via LBQ657, the active [[metabolite]] of the prodrug sacubitril, and blocks the [[Angiotensin II receptor type 1|angiotensin II type-1 (AT1) receptor]] via [[valsartan]]. The cardiovascular and renal effects of sacubitril and [[valsartan]] in [[heart failure]] patients are attributed to the increased levels of [[peptides]] that are degraded by [[neprilysin]], such as [[natriuretic peptides]], by LBQ657, and the simultaneous inhibition of the effects of [[angiotensin II]] by valsartan. Valsartan inhibits the effects of [[angiotensin II]] by selectively blocking the [[Angiotensin II receptor type 1|AT1 receptor]], and also inhibits [[angiotensin II]]-dependent [[aldosterone]] release. | ||
|structure=Sacubitril and [[valsartan]] (sacubitril and [[valsartan]]) is a combination of a [[neprilysin]] inhibitor and an [[angiotensin II receptor blocker]]. | |structure=Sacubitril and [[valsartan]] (sacubitril and [[valsartan]]) is a combination of a [[neprilysin]] inhibitor and an [[angiotensin II receptor blocker]]. | ||
Sacubitril and [[valsartan]] contains a complex comprised of anionic forms of sacubitril and [[valsartan]], sodium cations, and water molecules in the molar ratio of 1:1:3:2.5, respectively. Following oral administration, the complex dissociates into sacubitril (which is further metabolized to LBQ657) and [[valsartan]]. The complex is chemically described as Octadecasodiumhexakis(4-{[(1S,3R)-1-([1,1´-biphenyl]-4-ylmethyl)-4-ethoxy-3-methyl-4-oxobutyl]amino}-4-oxobutanoate)hexakis(N-pentanoyl-N-{[2´-(1H-tetrazol-1-id-5-yl)[1,1´-biphenyl]-4-yl]methyl}-L-valinate)—water (1/15). | Sacubitril and [[valsartan]] contains a complex comprised of [[anionic]] forms of sacubitril and [[valsartan]], [[sodium]] [[cations]], and water molecules in the molar ratio of 1:1:3:2.5, respectively. Following oral administration, the complex dissociates into sacubitril (which is further metabolized to LBQ657) and [[valsartan]]. The complex is chemically described as Octadecasodiumhexakis(4-{[(1S,3R)-1-([1,1´-biphenyl]-4-ylmethyl)-4-ethoxy-3-methyl-4-oxobutyl]amino}-4-oxobutanoate)hexakis(N-pentanoyl-N-{[2´-(1H-tetrazol-1-id-5-yl)[1,1´-biphenyl]-4-yl]methyl}-L-valinate)—water (1/15). | ||
Its empirical formula (hemipentahydrate) is C48H55N6O8Na3 2.5 H2O. Its molecular mass is 957.99 and its schematic structural formula is: | Its empirical formula (hemipentahydrate) is C48H55N6O8Na3 2.5 H2O. Its molecular mass is 957.99 and its schematic structural formula is: | ||
[[File:Sacubitril and Valsartan structure.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Sacubitril and Valsartan structure.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
|PD=The pharmacodynamic effects of sacubitril and [[valsartan]] were evaluated after single and multiple dose administrations in healthy subjects and in patients with [[heart failure]], and are consistent with simultaneous [[neprilysin]] inhibition and renin-angiotensin system blockade. In a 7-day [[valsartan]]-controlled study in patients with reduced ejection fraction (HFrEF), administration of sacubitril and [[valsartan]] resulted in a significant non-sustained increase in natriuresis, increased urine cGMP, and decreased plasma MR-proANP and NT-proBNP compared to [[valsartan]]. | |PD=The pharmacodynamic effects of sacubitril and [[valsartan]] were evaluated after single and multiple dose administrations in healthy subjects and in patients with [[heart failure]], and are consistent with simultaneous [[neprilysin]] inhibition and [[renin-angiotensin system]] blockade. In a 7-day [[valsartan]]-controlled study in patients with reduced [[ejection fraction]] ([[HFrEF]]), administration of sacubitril and [[valsartan]] resulted in a significant non-sustained increase in [[urine|natriuresis]], increased [[urine]] [[cGMP]], and decreased plasma MR-proANP and NT-proBNP compared to [[valsartan]]. | ||
In a 21-day study in HFrEF patients, sacubitril and [[valsartan]] significantly increased urine ANP and cGMP and plasma cGMP, and decreased plasma NT-proBNP, aldosterone and endothelin-1. Sacubitril and [[valsartan]] also blocked the AT1-receptor as evidenced by increased plasma renin activity and plasma renin concentrations. In PARADIGM-HF, sacubitril and [[valsartan]] decreased plasma NT-proBNP (not a [[neprilysin]] substrate) and increased plasma BNP (a [[neprilysin]] substrate) and urine cGMP compared with enalapril. | In a 21-day study in [[HFrEF]] patients, sacubitril and [[valsartan]] significantly increased [[urine]] ANP and [[cGMP]] and plasma [[cGMP]], and decreased plasma NT-proBNP, [[aldosterone]] and [[endothelin-1]]. Sacubitril and [[valsartan]] also blocked the [[Angiotensin II receptor type 1|AT1-receptor]] as evidenced by increased plasma [[renin]] activity and plasma [[renin]] concentrations. In PARADIGM-HF, sacubitril and [[valsartan]] decreased plasma NT-proBNP (not a [[neprilysin]] substrate) and increased plasma [[BNP]] (a [[neprilysin]] substrate) and [[urine]] [[cGMP]] compared with [[enalapril]]. | ||
QT Prolongation: In a thorough QTc clinical study in healthy male subjects, single doses of sacubitril and [[valsartan]] 194 mg sacubitril/206 mg [[valsartan]] and 583 mg sacubitril/617 mg [[valsartan]] had no effect on cardiac repolarization. | [[QT]] Prolongation: In a thorough [[QTc]] clinical study in healthy male subjects, single doses of sacubitril and [[valsartan]] 194 mg sacubitril/206 mg [[valsartan]] and 583 mg sacubitril/617 mg [[valsartan]] had no effect on cardiac [[repolarization]]. | ||
Amyloid-β: [[Neprilysin]] is one of multiple enzymes involved in the clearance of | [[Amyloid beta|Amyloid-β]]: [[Neprilysin]] is one of multiple enzymes involved in the clearance of [[Amyloid beta|Amyloid-β]] (Aβ) from the brain and [[cerebrospinal fluid]] (CSF). Administration of sacubitril and [[valsartan]] 194 mg sacubitril/206 mg [[valsartan]] once-daily for 2 weeks to healthy subjects was associated with an increase in [[cerebrospinal fluid|CSF]] [[Amyloid beta|Aβ1-38]] compared to placebo; there were no changes in concentrations of [[cerebrospinal fluid|CSF]] [[Amyloid beta|Aβ1-40]] or [[cerebrospinal fluid|CSF]] [[Amyloid beta|Aβ1-42]]. The clinical relevance of this finding is unknown. | ||
Blood Pressure: Addition of a 50 mg single dose of sildenafil to sacubitril and [[valsartan]] at steady state (194 mg sacubitril/206 mg [[valsartan]] mg once daily for 5 days) in patients with hypertension was associated with additional blood pressure (BP) reduction (~5/4 mmHg, systolic/diastolic BP) compared to administration of sacubitril and [[valsartan]] alone. | [[blood pressure|Blood Pressure]]: Addition of a 50 mg single dose of [[sildenafil]] to sacubitril and [[valsartan]] at steady state (194 mg sacubitril/206 mg [[valsartan]] mg once daily for 5 days) in patients with [[hypertension]] was associated with additional [[blood pressure]] (BP) reduction (~5/4 mmHg, systolic/diastolic BP) compared to administration of sacubitril and [[valsartan]] alone. | ||
Co-administration of sacubitril and [[valsartan]] did not significantly alter the BP effect of intravenous nitroglycerin. | Co-administration of sacubitril and [[valsartan]] did not significantly alter the BP effect of [[intravenous]] [[nitroglycerin]]. | ||
|PK='''Absorption''' | |PK='''Absorption''' | ||
Following oral administration, sacubitril and [[valsartan]] dissociates into sacubitril and [[valsartan]]. Sacubitril is further metabolized to LBQ657. The peak plasma concentrations of sacubitril, LBQ657, and [[valsartan]] are reached in 0.5 hours, 2 hours, and 1.5 hours, respectively. The oral absolute bioavailability of sacubitril is estimated to be ≥ 60%. The [[valsartan]] in sacubitril and [[valsartan]] is more bioavailable than the [[valsartan]] in other marketed tablet formulations; 26 mg, 51 mg, and 103 mg of [[valsartan]] in sacubitril and [[valsartan]] is equivalent to 40 mg, 80 mg, and 160 mg of [[valsartan]] in other marketed tablet formulations, respectively. | Following oral administration, sacubitril and [[valsartan]] dissociates into sacubitril and [[valsartan]]. Sacubitril is further metabolized to LBQ657. The peak plasma concentrations of sacubitril, LBQ657, and [[valsartan]] are reached in 0.5 hours, 2 hours, and 1.5 hours, respectively. The oral absolute bioavailability of sacubitril is estimated to be ≥ 60%. The [[valsartan]] in sacubitril and [[valsartan]] is more bioavailable than the [[valsartan]] in other marketed tablet formulations; 26 mg, 51 mg, and 103 mg of [[valsartan]] in sacubitril and [[valsartan]] is equivalent to 40 mg, 80 mg, and 160 mg of [[valsartan]] in other marketed tablet formulations, respectively. | ||
| Line 144: | Line 145: | ||
'''Distribution''' | '''Distribution''' | ||
Sacubitril, LBQ657 and [[valsartan]] are highly bound to plasma proteins (94% to 97%). Based on the comparison of plasma and CSF exposures, LBQ657 crosses the blood brain barrier to a limited extent (0.28%). The average apparent volumes of distribution of [[valsartan]] and sacubitril are 75 and 103 L, respectively. | |||
Sacubitril, LBQ657, and [[valsartan]] are highly bound to [[plasma proteins]] (94% to 97%). Based on the comparison of plasma and [[cerebrospinal fluid|CSF]] exposures, LBQ657 crosses the [[blood brain barrier]] to a limited extent (0.28%). The average apparent volumes of distribution of [[valsartan]] and sacubitril are 75 and 103 L, respectively. | |||
'''[[Metabolism]]''' | '''[[Metabolism]]''' | ||
Sacubitril is readily converted to LBQ657 by esterases; LBQ657 is not further metabolized to a significant extent. [[Valsartan]] is minimally metabolized; only about 20% of the dose is recovered as metabolites. A hydroxyl metabolite has been identified in plasma at low concentrations (< 10%). | |||
Sacubitril is readily converted to LBQ657 by [[esterase|esterases]]; LBQ657 is not further metabolized to a significant extent. [[Valsartan]] is minimally metabolized; only about 20% of the dose is recovered as [[metabolite|metabolites]]. A hydroxyl [[metabolite]] has been identified in plasma at low concentrations (< 10%). | |||
'''Elimination''' | '''Elimination''' | ||
Following oral administration, 52% to 68% of sacubitril (primarily as LBQ657) and ~13% of [[valsartan]] and its metabolites are excreted in urine; 37% to 48% of sacubitril (primarily as LBQ657), and 86% of [[valsartan]] and its metabolites are excreted in feces. Sacubitril, LBQ657, and [[valsartan]] are eliminated from plasma with a mean elimination half-life (T1/2) of approximately 1.4 hours, 11.5 hours, and 9.9 hours, respectively. | |||
Following oral administration, 52% to 68% of sacubitril (primarily as LBQ657) and ~13% of [[valsartan]] and its [[metabolite|metabolites]] are excreted in [[urine]]; 37% to 48% of sacubitril (primarily as LBQ657), and 86% of [[valsartan]] and its [[metabolite|metabolites]] are excreted in [[feces]]. Sacubitril, LBQ657, and [[valsartan]] are eliminated from plasma with a mean elimination half-life (T1/2) of approximately 1.4 hours, 11.5 hours, and 9.9 hours, respectively. | |||
'''Linearity/Nonlinearity''' | '''Linearity/Nonlinearity''' | ||
The pharmacokinetics of sacubitril, LBQ657, and [[valsartan]] were linear over an sacubitril and [[valsartan]] dose range of 24 mg sacubitril/26 mg [[valsartan]] to 194 mg sacubitril/206 mg [[valsartan]]. | The pharmacokinetics of sacubitril, LBQ657, and [[valsartan]] were linear over an sacubitril and [[valsartan]] dose range of 24 mg sacubitril/26 mg [[valsartan]] to 194 mg sacubitril/206 mg [[valsartan]]. | ||
'''Drug Interactions''' | '''Drug Interactions''' | ||
Effect of co-administered drugs on sacubitril and [[valsartan]]: | Effect of co-administered drugs on sacubitril and [[valsartan]]: | ||
Because CYP450 enzyme-mediated metabolism of sacubitril and [[valsartan]] is minimal, coadministration with drugs that impact CYP450 enzymes is not expected to affect the pharmacokinetics of sacubitril and [[valsartan]]. Dedicated drug interaction studies demonstrated that coadministration of furosemide, warfarin, digoxin, carvedilol, a combination of levonorgestrel/ethinyl estradiol, amlodipine, omeprazole, hydrochlorothiazide (HCTZ), metformin, atorvastatin, and sildenafil, did not alter the systemic exposure to sacubitril, LBQ657 or [[valsartan]]. | Because [[CYP450]] enzyme-mediated [[metabolism]] of sacubitril and [[valsartan]] is minimal, coadministration with drugs that impact [[CYP450]] enzymes is not expected to affect the pharmacokinetics of sacubitril and [[valsartan]]. Dedicated drug interaction studies demonstrated that coadministration of [[furosemide]], [[warfarin]], [[digoxin]], [[carvedilol]], a combination of [[levonorgestrel]]/[[ethinyl estradiol]], [[amlodipine]], [[omeprazole]], [[hydrochlorothiazide]] (HCTZ), [[metformin]], [[atorvastatin]], and [[sildenafil]], did not alter the systemic exposure to sacubitril, LBQ657 or [[valsartan]]. | ||
Effect of sacubitril and [[valsartan]] on co-administered drugs: | Effect of sacubitril and [[valsartan]] on co-administered drugs: | ||
| Line 164: | Line 170: | ||
'''Specific Populations''' | '''Specific Populations''' | ||
Effect of specific populations on the pharmacokinetics of LBQ657 and [[valsartan]] are shown in Figure 2. | Effect of specific populations on the pharmacokinetics of LBQ657 and [[valsartan]] are shown in Figure 2. | ||
[[File:Sacubitril and Valsartan F2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Sacubitril and Valsartan F2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
|nonClinToxic=''' | |nonClinToxic='''[[Carcinogenesis]], [[Mutagenesis]], Impairment of [[Fertility]]''' | ||
Impairment of Fertility: | [[Carcinogenesis]] and [[Mutagenesis]]: | ||
Sacubitril and [[valsartan]] did not show any effects on fertility in rats up to a dose of 73 mg sacubitril/77 mg [[valsartan]]/kg/day (≤1.0-fold and ≤ 0.18-fold the MRHD on the basis of the AUCs of [[valsartan]] and LBQ657, respectively). | [[Carcinogenicity]] studies conducted in mice and rats with sacubitril and [[valsartan]] did not identify any [[carcinogenic]] potential for sacubitril and [[valsartan]]. The LBQ657 [[Cmax]] at the high dose (HD) of 1200 mg/kg/day in male and female mice was, respectively, 14 and 16 times that in humans at the MRHD. The LBQ657 [[Cmax]] in male and female rats at the HD of 400 mg/kg/day was, respectively, 1.7 and 3.5 times that at the MRHD. The doses of [[valsartan]] studied (high dose of 160 and 200 mg/kg/day in mice and rats, respectively) were about 4 and 10 times, respectively, the MRHD on a mg/m2 basis. | ||
Mutagenicity and clastogenicity studies conducted with sacubitril and [[valsartan]], sacubitril, and [[valsartan]] did not reveal any effects at either the gene or [[chromosome]] level. | |||
Impairment of [[Fertility]]: | |||
Sacubitril and [[valsartan]] did not show any effects on [[fertility]] in rats up to a dose of 73 mg sacubitril/77 mg [[valsartan]]/kg/day (≤1.0-fold and ≤ 0.18-fold the MRHD on the basis of the [[AUC|AUCs]] of [[valsartan]] and LBQ657, respectively). | |||
'''Animal Toxicology and/or Pharmacology''' | '''Animal Toxicology and/or Pharmacology''' | ||
The effects of sacubitril and [[valsartan]] on | |||
The effects of sacubitril and [[valsartan]] on [[Amyloid beta|Amyloid-β]] concentrations in [[cerebrospinal fluid|CSF]] and brain tissue were assessed in young (2 to 4 years old) cynomolgus monkeys treated with sacubitril and [[valsartan]] (24 mg sacubitril/26 mg [[valsartan]]/kg/day) for 2 weeks. In this study, sacubitril and [[valsartan]] affected [[cerebrospinal fluid|CSF]] [[Amyloid beta|Amyloid-β]] clearance, increasing [[cerebrospinal fluid|CSF]] [[Amyloid beta|Amyloid-β]] 1-40, 1-42, and 1-38 levels in [[cerebrospinal fluid|CSF]]; there was no corresponding increase in [[Amyloid beta|Amyloid-β]] levels in the brain. In addition, in a toxicology study in cynomolgus monkeys treated with sacubitril and [[valsartan]] at 146 mg sacubitril/154 mg [[valsartan]]/kg/day for 39-weeks, there was no [[Amyloid beta|Amyloid-β]] accumulation in the brain. | |||
|clinicalStudies=Dosing in clinical trials was based on the total amount of both components of sacubitril and [[valsartan]], i.e., 24/26 mg, 49/51 mg and 97/103 mg were referred to as 50 mg, 100 mg, and 200 mg, respectively. | |clinicalStudies=Dosing in clinical trials was based on the total amount of both components of sacubitril and [[valsartan]], i.e., 24/26 mg, 49/51 mg and 97/103 mg were referred to as 50 mg, 100 mg, and 200 mg, respectively. | ||
'''PARADIGM-HF''' | '''PARADIGM-HF''' | ||
The primary objective of PARADIGM-HF was to determine whether sacubitril and [[valsartan]], a combination of sacubitril and a RAS inhibitor (valsartan), was superior to a RAS inhibitor (enalapril) alone in reducing the risk of the combined endpoint of cardiovascular (CV) death or hospitalization for [[heart failure]] (HF). | PARADIGM-HF was a multinational, randomized, double-blind trial comparing sacubitril and [[valsartan]] and [[enalapril]] in 8,442 adult patients with symptomatic [[chronic heart failure]] ([[New york heart association functional classification|NYHA Class]] II–IV) and [[systolic dysfunction]] ([[left ventricular ejection fraction]] ≤ 40%). Patients had to have been on an [[ACE inhibitor]] or [[ARB]] for at least four weeks and on maximally tolerated doses of [[beta blocker|beta-blockers]]. Patients with a [[systolic blood pressure]] of < 100 mmHg at screening were excluded. | ||
The primary objective of PARADIGM-HF was to determine whether sacubitril and [[valsartan]], a combination of sacubitril and a RAS inhibitor ([[valsartan]]), was superior to a RAS inhibitor ([[enalapril]]) alone in reducing the risk of the combined endpoint of cardiovascular (CV) death or hospitalization for [[heart failure]] (HF). | |||
After discontinuing their existing ACE inhibitor or [[ARB]] therapy, patients entered sequential single-blind run-in periods during which they received enalapril 10 mg twice-daily, followed by sacubitril and [[valsartan]] 100 mg twice-daily, increasing to 200 mg twice daily. Patients who successfully completed the sequential run-in periods were randomized to receive either sacubitril and [[valsartan]] 200 mg (N=4,209) twice-daily or enalapril 10 mg (N=4,233) twice-daily. The primary endpoint was the first event in the composite of CV death or hospitalization for HF. The median follow-up duration was 27 months and patients were treated for up to 4.3 years. | After discontinuing their existing [[ACE inhibitor]] or [[ARB]] therapy, patients entered sequential single-blind run-in periods during which they received [[enalapril]] 10 mg twice-daily, followed by sacubitril and [[valsartan]] 100 mg twice-daily, increasing to 200 mg twice daily. Patients who successfully completed the sequential run-in periods were randomized to receive either sacubitril and [[valsartan]] 200 mg (N=4,209) twice-daily or [[enalapril]] 10 mg (N=4,233) twice-daily. The primary endpoint was the first event in the composite of CV death or hospitalization for [[heart failure|HF]]. The median follow-up duration was 27 months and patients were treated for up to 4.3 years. | ||
The population was 66% Caucasian, 18% Asian, and 5% Black; the mean age was 64 years and 78% were male. At randomization, 70% of patients were [[New york heart association functional classification|NYHA Class]] II, 24% were [[New york heart association functional classification|NYHA Class]] III, and 0.7% were [[New york heart association functional classification|NYHA Class]] IV. The mean left ventricular ejection fraction was 29%. The underlying cause of [[heart failure]] was coronary artery disease in 60% of patients; 71% had a history of hypertension, 43% had a history of myocardial infarction, 37% had an eGFR < 60 mL/min/1.73m2, and 35% had diabetes mellitus. Most patients were taking beta-blockers (94%), mineralocorticoid antagonists (58%), and diuretics (82%). Few patients had an implantable cardioverter-defibrillator (ICD) or cardiac resynchronization therapy-defibrillator (CRT-D) (15%). | The population was 66% Caucasian, 18% Asian, and 5% Black; the mean age was 64 years and 78% were male. At randomization, 70% of patients were [[New york heart association functional classification|NYHA Class]] II, 24% were [[New york heart association functional classification|NYHA Class]] III, and 0.7% were [[New york heart association functional classification|NYHA Class]] IV. The mean [[left ventricular ejection fraction]] was 29%. The underlying cause of [[heart failure]] was [[coronary artery disease]] in 60% of patients; 71% had a history of [[hypertension]], 43% had a history of [[myocardial infarction]], 37% had an [[glomerular filtration rate|eGFR]] < 60 mL/min/1.73m2, and 35% had [[diabetes mellitus]]. Most patients were taking [[beta blocker|beta-blockers]] (94%), [[mineralocorticoid]] antagonists (58%), and [[diuretics]] (82%). Few patients had an [[implantable cardioverter-defibrillator]] (ICD) or cardiac resynchronization therapy-defibrillator (CRT-D) (15%). | ||
PARADIGM-HF demonstrated that sacubitril and [[valsartan]], a combination of sacubitril and a RAS inhibitor (valsartan), was superior to a RAS inhibitor (enalapril), in reducing the risk of the combined endpoint of cardiovascular death or hospitalization for [[heart failure]], based on a time-to-event analysis (hazard ratio [HR]: 0.80, 95% confidence interval [CI], 0.73, 0.87, p <0.0001). The treatment effect reflected a reduction in both cardiovascular death and [[heart failure]] hospitalization; see Table 2 and Figure 3. Sudden death accounted for 45% of cardiovascular deaths, followed by pump failure, which accounted for 26%. | PARADIGM-HF demonstrated that sacubitril and [[valsartan]], a combination of sacubitril and a RAS inhibitor ([[valsartan]]), was superior to a RAS inhibitor ([[enalapril]]), in reducing the risk of the combined endpoint of cardiovascular death or hospitalization for [[heart failure]], based on a time-to-event analysis (hazard ratio [HR]: 0.80, 95% confidence interval [CI], 0.73, 0.87, p <0.0001). The treatment effect reflected a reduction in both cardiovascular death and [[heart failure]] hospitalization; see Table 2 and Figure 3. Sudden death accounted for 45% of cardiovascular deaths, followed by pump failure, which accounted for 26%. | ||
Sacubitril and [[valsartan]] also improved overall survival (HR 0.84; 95% CI [0.76, 0.93], p = 0.0009) (Table 2). This finding was driven entirely by a lower incidence of cardiovascular mortality on sacubitril and [[valsartan]]. | Sacubitril and [[valsartan]] also improved overall survival (HR 0.84; 95% CI [0.76, 0.93], p = 0.0009) (Table 2). This finding was driven entirely by a lower incidence of cardiovascular mortality on sacubitril and [[valsartan]]. | ||
| Line 204: | Line 214: | ||
[[File:Sacubitril and Valsartan ingredients2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Sacubitril and Valsartan ingredients2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
[[File:Sacubitril and Valsartan ingredients3.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Sacubitril and Valsartan ingredients3.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
[[File:Sacubitril and Valsartan label1. | [[File:Sacubitril and Valsartan label1.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
[[File:Sacubitril and Valsartan label2. | [[File:Sacubitril and Valsartan label2.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
[[File:Sacubitril and Valsartan label3. | [[File:Sacubitril and Valsartan label3.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
|fdaPatientInfo=Advise patients to read the FDA-approved patient labeling (Patient Information). | |fdaPatientInfo=Advise patients to read the FDA-approved patient labeling (Patient Information). | ||
Pregnancy: Advise female patients of childbearing age about the consequences of exposure to sacubitril and [[valsartan]] during pregnancy. Discuss treatment options with women planning to become pregnant. Ask patients to report pregnancies to their physicians as soon as possible. | Pregnancy: Advise female patients of childbearing age about the consequences of exposure to sacubitril and [[valsartan]] during pregnancy. Discuss treatment options with women planning to become pregnant. Ask patients to report pregnancies to their physicians as soon as possible. | ||
Angioedema: Advise patients to discontinue use of their previous ACE inhibitor or [[ARB]]. Advise patients to allow a 36 hour wash-out period if switching from or to an ACE inhibitor. | [[Angioedema]]: Advise patients to discontinue use of their previous [[ACE inhibitor]] or [[ARB]]. Advise patients to allow a 36 hour wash-out period if switching from or to an [[ACE inhibitor]]. | ||
|alcohol=Alcohol-Sacubitril and [[Valsartan]] interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Sacubitril and [[Valsartan]] interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
|brandNames=ENTRESTO | |brandNames=ENTRESTO | ||
}} | }} | ||
Latest revision as of 15:54, 25 July 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Allison Tu [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
|
Overview
Sacubitril and Valsartan is a combination of a neprilysin inhibitor and an angiotensin II receptor blocker that is FDA approved for the prevention of of cardiovascular death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II-IV) and reduced ejection fraction. There is a Black Box Warning for this drug as shown here. Common adverse reactions include hypotension, increased serum potassium, hyperkalemia, and increased serum creatinine.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Sacubitril and valsartan is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II-IV) and reduced ejection fraction.
Dosing Information
- Sacubitril and valsartan is contraindicated with concomitant use of an angiotensin-converting enzyme (ACE) inhibitor. If switching from an ACE inhibitor to sacubitril and valsartan, allow a washout period of 36 hours between administration of the two drugs.
- The recommended starting dose of sacubitril and valsartan is 49/51 mg twice-daily.
- Double the dose of sacubitril and valsartan after 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient.
- Dose Adjustment for Patients Not Taking an ACE inhibitor or ARB or Previously Taking Low Doses of These Agents
- A starting dose of 24/26 mg twice-daily is recommended for patients not currently taking an ACE inhibitor or an angiotensin II receptor blocker (ARB) and for patients previously taking low doses of these agents. Double the dose of sacubitril and valsartan every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient.
- Dose Adjustment for Severe Renal Impairment
- A starting dose of 24/26 mg twice-daily is recommended for patients with severe renal impairment (eGFR <30 mL/min/1.73 m2). Double the dose of sacubitril and valsartan every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient.
- No starting dose adjustment is needed for mild or moderate renal impairment.
- Dose Adjustment for Hepatic Impairment
- A starting dose of 24/26 mg twice-daily is recommended for patients with moderate hepatic impairment (Child-Pugh B classification). Double the dose of sacubitril and valsartan every 2 to 4 weeks to the target maintenance dose of 97/103 mg twice daily, as tolerated by the patient.
- No starting dose adjustment is needed for mild hepatic impairment.
- Use in patients with severe hepatic impairment is not recommended.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sacubitril and Valsartan in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sacubitril and Valsartan in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Sacubitril and Valsartan FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sacubitril and Valsartan in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sacubitril and Valsartan in pediatric patients.
Contraindications
Sacubitril and valsartan is contraindicated:
- In patients with hypersensitivity to any component.
- In patients with a history of angioedema related to previous ACE inhibitor or ARB therapy.
- With concomitant use of ACE inhibitors. Do not administer within 36 hours of switching from or to an ACE inhibitor.
- With concomitant use of aliskiren in patients with diabetes.
Warnings
|
FETAL TOXICITY
See full prescribing information for complete Boxed Warning.
|
- Fetal Toxicity
- Sacubitril and valsartan can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death.
- When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and valsartan. However, if there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system, and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus.
- Angioedema
- Sacubitril and valsartan may cause angioedema. In the double-blind period of PARADIGM-HF, 0.5% of patients treated with sacubitril and valsartan and 0.2% of patients treated with enalapril had angioedema.
- If angioedema occurs, discontinue sacubitril and valsartan immediately, provide appropriate therapy, and monitor for airway compromise. Sacubitril and valsartan must not be re-administered. In cases of confirmed angioedema where swelling has been confined to the face and lips, the condition has generally resolved without treatment, although antihistamines have been useful in relieving symptoms.
- Angioedema associated with laryngeal edema may be fatal. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, administer appropriate therapy, e.g., subcutaneous epinephrine/adrenaline solution 1:1000 (0.3 mL to 0.5 mL) and take measures necessary to ensure maintenance of a patent airway.
- Sacubitril and valsartan has been associated with a higher rate of angioedema in Black than in non-Black patients.
- Patients with a prior history of angioedema may be at increased risk of angioedema with sacubitril and valsartan. Sacubitril and valsartan should not be used in patients with a known history of angioedema related to previous ACE inhibitor or ARB therapy.
- Hypotension
- Sacubitril and valsartan lowers blood pressure and may cause symptomatic hypotension. Patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics), are at greater risk. In the double-blind period of PARADIGM-HF, 18% of patients treated with sacubitril and valsartan and 12% of patients treated with enalapril reported hypotension as an adverse event, with hypotension reported as a serious adverse event in approximately 1.5% of patients in both treatment arms.
- Correct volume or salt depletion prior to administration of sacubitril and valsartan or start at a lower dose. If hypotension occurs, consider dose adjustment of diuretics, concomitant antihypertensive drugs, and treatment of other causes of hypotension (e.g., hypovolemia). If hypotension persists despite such measures, reduce the dosage or temporarily discontinue sacubitril and valsartan. Permanent discontinuation of therapy is usually not required.
- Impaired Renal Function
- As a consequence of inhibiting the renin-angiotensin-aldosterone system (RAAS), decreases in renal function may be anticipated in susceptible individuals treated with sacubitril and valsartan. In the double-blind period of PARADIGM-HF, 5% of patients in both the sacubitril and valsartan and enalapril groups reported renal failure as an adverse event.
- In patients whose renal function depends upon the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with ACE inhibitors and angiotensin receptor antagonists has been associated with oliguria, progressive azotemia and, rarely, acute renal failure and death.
- Closely monitor serum creatinine, and down-titrate or interrupt sacubitril and valsartan in patients who develop a clinically significant decrease in renal function.
- As with all drugs that affect the RAAS, sacubitril and valsartan may increase blood urea and serum creatinine levels in patients with bilateral or unilateral renal artery stenosis. In patients with renal artery stenosis, monitor renal function.
- Hyperkalemia
- Through its actions on the RAAS, hyperkalemia may occur with sacubitril and valsartan. In the double-blind period of PARADIGM-HF, 12% of patients treated with sacubitril and valsartan and 14% of patients treated with enalapril reported hyperkalemia as an adverse event.
- Monitor serum potassium periodically and treat appropriately, especially in patients with risk factors for hyperkalemia such as severe renal impairment, diabetes, hypoaldosteronism, or a high potassium diet. Dosage reduction or interruption of sacubitril and valsartan may be required.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In the PARADIGM-HF trial, subjects were required to complete sequential enalapril and sacubitril and valsartan run-in periods of (median) 15 and 29 days, respectively, prior to entering the randomized double-blind period comparing sacubitril and valsartan and enalapril. During the enalapril run-in period, 1,102 patients (10.5%) were permanently discontinued from the study, 5.6% because of an adverse event, most commonly renal dysfunction (1.7%), hyperkalemia (1.7%) and hypotension (1.4%). During the sacubitril and valsartan run-in period, an additional 10.4% of patients permanently discontinued treatment, 5.9% because of an adverse event, most commonly renal dysfunction (1.8%), hypotension (1.7%) and hyperkalemia (1.3%). Because of this run-in design, the adverse reaction rates described below are lower than expected in practice.
In the double-blind period, safety was evaluated in 4,203 patients treated with sacubitril and valsartan and 4,229 treated with enalapril. In PARADIGM-HF, patients randomized to sacubitril and valsartan received treatment for up to 4.3 years, with a median duration of exposure of 24 months; 3,271 patients were treated for more than one year. Discontinuation of therapy because of an adverse event during the double-blind period occurred in 450 (10.7%) of sacubitril and valsartan treated patients and 516 (12.2%) of patients receiving enalapril.
Adverse reactions occurring at an incidence of ≥5% in patients who were treated with sacubitril and valsartan in the double-blind period are shown in Table 1.
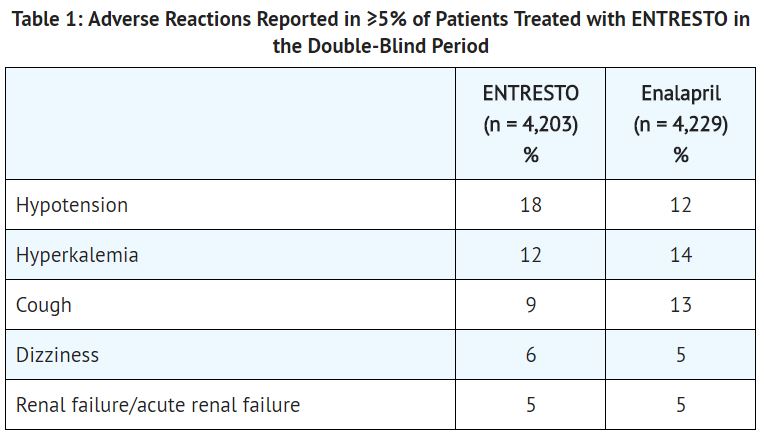
In the PARADIGM-HF trial, the incidence of angioedema was 0.1% in both the enalapril and sacubitril and valsartan run-in periods. In the double-blind period, the incidence of angioedema was higher in patients treated with sacubitril and valsartan than enalapril (0.5% and 0.2%, respectively). The incidence of angioedema in Black patients was 2.4% with sacubitril and valsartan and 0.5% with enalapril.
Orthostasis was reported in 2.1% of patients treated with sacubitril and valsartan compared to 1.1% of patients treated with enalapril during the double-blind period of PARADIGM-HF. Falls were reported in 1.9% of patients treated with sacubitril and valsartan compared to 1.3% of patients treated with enalapril.
Laboratory Abnormalities:
- Hemoglobin and Hematocrit
- Decreases in hemoglobin/hematocrit of >20% were observed in approximately 5% of both sacubitril and valsartan- and enalapril-treated patients in the double-blind period in PARADIGM-HF.
- Serum Creatinine
- Increases in serum creatinine of >50% were observed in 1.4% of patients in the enalapril run-in period and 2.2% of patients in the sacubitril and valsartan run-in period. During the double-blind period, approximately 16% of both sacubitril and valsartan- and enalapril-treated patients had increases in serum creatinine of >50%.
- Serum Potassium
- Potassium concentrations >5.5 mEq/L were observed in approximately 4% of patients in both the enalapril and sacubitril and valsartan run-in periods. During the double-blind period, approximately 16% of both sacubitril and valsartan- and enalapril-treated patients had potassium concentrations >5.5 mEq/L.
Postmarketing Experience
There is limited information regarding Sacubitril and Valsartan Postmarketing Experience in the drug label.
Drug Interactions
- Dual Blockade of the Renin-Angiotensin-Aldosterone System
- Concomitant use of sacubitril and valsartan with an ACE inhibitor is contraindicated because of the increased risk of angioedema.
- Avoid use of sacubitril and valsartan with an ARB, because sacubitril and valsartan contains the angiotensin II receptor blocker valsartan.
- The concomitant use of sacubitril and valsartan with aliskiren is contraindicated in patients with diabetes. Avoid use with aliskiren in patients with renal impairment (eGFR <60 mL/min/1.73 m2).
- Potassium-Sparing Diuretics
- As with other drugs that block angiotensin II or its effects, concomitant use of potassium-sparing diuretics (e.g., spironolactone, triamterene, amiloride), potassium supplements, or salt substitutes containing potassium may lead to increases in serum potassium.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors)
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, concomitant use of NSAIDs, including COX-2 inhibitors, with sacubitril and valsartan may result in worsening of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically.
- Lithium
Use in Specific Populations
Pregnancy
- Risk Summary
- Sacubitril and valsartan can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death.
- Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. In animal reproduction studies, sacubitril and valsartan treatment during organogenesis resulted in increased embryo-fetal lethality in rats and rabbits and teratogenicity in rabbits.
- When pregnancy is detected, consider alternative drug treatment and discontinue sacubitril and valsartan. However, if there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system, and if the drug is considered lifesaving for the mother, advise a pregnant woman of the potential risk to the fetus.
- The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
- Clinical Considerations
- Fetal/Neonatal Adverse Reactions
- Oligohydramnios in pregnant women who use drugs affecting the renin-angiotensin system in the second and third trimesters of pregnancy can result in the following: reduced fetal renal function leading to anuria and renal failure, fetal lung hypoplasia, skeletal deformations, including skull hypoplasia, hypotension, and death.
- Perform serial ultrasound examinations to assess the intra-amniotic environment. Fetal testing may be appropriate, based on the week of gestation. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. If oligohydramnios is observed, consider alternative drug treatment.
- Closely observe neonates with histories of in utero exposure to sacubitril and valsartan for hypotension, oliguria, and hyperkalemia. In neonates with a history of in utero exposure to sacubitril and valsartan, if oliguria or hypotension occurs, support blood pressure and renal perfusion. Exchange transfusions or dialysis may be required as a means of reversing hypotension and replacing renal function.
- Fetal/Neonatal Adverse Reactions
- Data
- Animal data
- Sacubitril and valsartan treatment during organogenesis resulted in increased embryo-fetal lethality in rats at doses ≥ 49 mg sacubitril/51 mg valsartan/kg/day (≤ 0.14 [LBQ657, the active metabolite] and 1.5 [valsartan]-fold the maximum recommended human dose [MRHD] of 97/103 mg twice-daily on the basis of the area under the plasma drug concentration-time curve [AUC]) and rabbits at doses ≥ 5 mg sacubitril/5 mg valsartan/kg/day (4-fold and 0.06-fold the MRHD on the basis of valsartan and LBQ657 AUC, respectively).
- Sacubitril and valsartan is teratogenic based on a low incidence of fetal hydrocephaly, associated with maternally toxic doses, which was observed in rabbits at an sacubitril and valsartan dose of ≥ 5 mg sacubitril/5 mg valsartan/kg/day. The adverse embryo-fetal effects of sacubitril and valsartan are attributed to the angiotensin receptor antagonist activity.
- Pre- and postnatal development studies in rats at sacubitril doses up to 750 mg/kg/day (4.5-fold the MRHD on the basis of LBQ657 AUC) and valsartan at doses up to 600 mg/kg/day (0.86-fold the MRHD on the basis of AUC) indicate that treatment with sacubitril and valsartan during organogenesis, gestation and lactation may affect pup development and survival.
- Animal data
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sacubitril and Valsartan in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Sacubitril and Valsartan during labor and delivery.
Nursing Mothers
- Risk Summary
- There is no information regarding the presence of sacubitril/valsartan in human milk, the effects on the breastfed infant, or the effects on milk production. Sacubitril/valsartan is present in rat milk. Because of the potential for serious adverse reactions in breastfed infants from exposure to sacubitril/valsartan, advise a nursing woman that breastfeeding is not recommended during treatment with sacubitril and valsartan.
- Data
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
No relevant pharmacokinetic differences have been observed in elderly (≥65 years) or very elderly (≥75 years) patients compared to the overall population.
Gender
There is no FDA guidance on the use of Sacubitril and Valsartan with respect to specific gender populations.
Race
There is no FDA guidance on the use of Sacubitril and Valsartan with respect to specific racial populations.
Renal Impairment
No dose adjustment is required in patients with mild (eGFR 60 to 90 mL/min/1.73 m2) to moderate (eGFR 30 to 60 mL/min/1.73 m2) renal impairment. The recommended starting dose in patients with severe renal impairment (eGFR <30 mL/min/1.73 m2) is 24/26 mg twice daily.
Hepatic Impairment
No dose adjustment is required when administering sacubitril and valsartan to patients with mild hepatic impairment (Child-Pugh A classification). The recommended starting dose in patients with moderate hepatic impairment (Child-Pugh B classification) is 24/26 mg twice daily. The use of sacubitril and valsartan in patients with severe hepatic impairment (Child-Pugh C classification) is not recommended, as no studies have been conducted in these patients.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Sacubitril and Valsartan in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Sacubitril and Valsartan in patients who are immunocompromised.
Administration and Monitoring
Administration
Sacubitril and valsartan is contraindicated with concomitant use of an angiotensin-converting enzyme (ACE) inhibitor. If switching from an ACE inhibitor to sacubitril and valsartan, allow a washout period of 36 hours between administration of the two drugs.
Monitoring
There is limited information regarding Sacubitril and Valsartan Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Sacubitril and Valsartan and IV administrations.
Overdosage
Limited data are available with regard to overdosage in human subjects with sacubitril and valsartan. In healthy volunteers, a single dose of sacubitril and valsartan 583 mg sacubitril/617 mg valsartan, and multiple doses of 437 mg sacubitril/463 mg valsartan (14 days) have been studied and were well tolerated.
Hypotension is the most likely result of overdosage due to the blood pressure lowering effects of sacubitril and valsartan. Symptomatic treatment should be provided.
Sacubitril and valsartan is unlikely to be removed by hemodialysis because of high protein binding.
Pharmacology
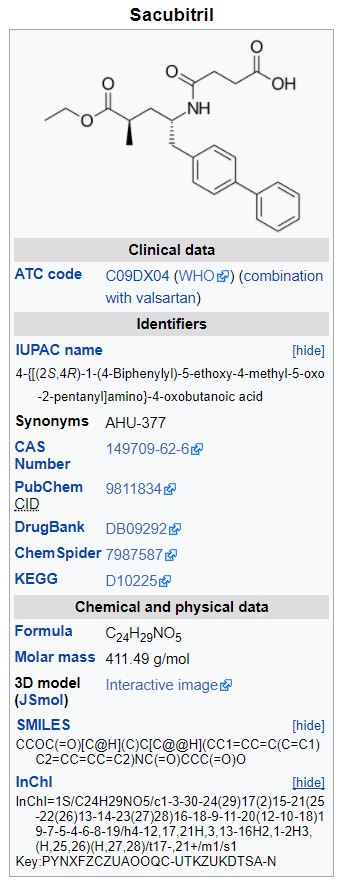
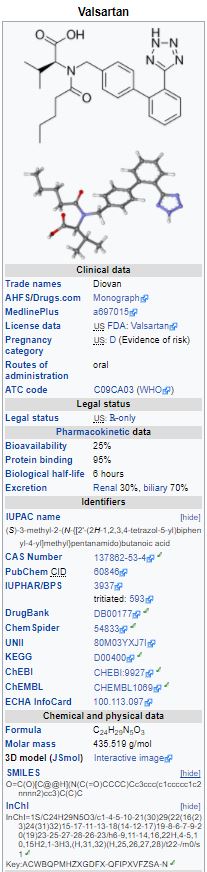
Mechanism of Action
Sacubitril and valsartan contains a neprilysin inhibitor, sacubitril, and an angiotensin receptor blocker, valsartan. Sacubitril and valsartan inhibits neprilysin (neutral endopeptidase; NEP) via LBQ657, the active metabolite of the prodrug sacubitril, and blocks the angiotensin II type-1 (AT1) receptor via valsartan. The cardiovascular and renal effects of sacubitril and valsartan in heart failure patients are attributed to the increased levels of peptides that are degraded by neprilysin, such as natriuretic peptides, by LBQ657, and the simultaneous inhibition of the effects of angiotensin II by valsartan. Valsartan inhibits the effects of angiotensin II by selectively blocking the AT1 receptor, and also inhibits angiotensin II-dependent aldosterone release.
Structure
Sacubitril and valsartan (sacubitril and valsartan) is a combination of a neprilysin inhibitor and an angiotensin II receptor blocker.
Sacubitril and valsartan contains a complex comprised of anionic forms of sacubitril and valsartan, sodium cations, and water molecules in the molar ratio of 1:1:3:2.5, respectively. Following oral administration, the complex dissociates into sacubitril (which is further metabolized to LBQ657) and valsartan. The complex is chemically described as Octadecasodiumhexakis(4-{[(1S,3R)-1-([1,1´-biphenyl]-4-ylmethyl)-4-ethoxy-3-methyl-4-oxobutyl]amino}-4-oxobutanoate)hexakis(N-pentanoyl-N-{[2´-(1H-tetrazol-1-id-5-yl)[1,1´-biphenyl]-4-yl]methyl}-L-valinate)—water (1/15).
Its empirical formula (hemipentahydrate) is C48H55N6O8Na3 2.5 H2O. Its molecular mass is 957.99 and its schematic structural formula is:
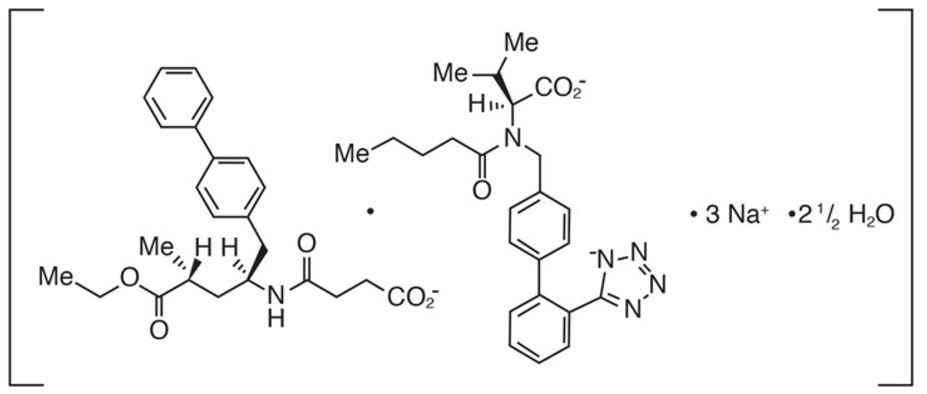
Pharmacodynamics
The pharmacodynamic effects of sacubitril and valsartan were evaluated after single and multiple dose administrations in healthy subjects and in patients with heart failure, and are consistent with simultaneous neprilysin inhibition and renin-angiotensin system blockade. In a 7-day valsartan-controlled study in patients with reduced ejection fraction (HFrEF), administration of sacubitril and valsartan resulted in a significant non-sustained increase in natriuresis, increased urine cGMP, and decreased plasma MR-proANP and NT-proBNP compared to valsartan.
In a 21-day study in HFrEF patients, sacubitril and valsartan significantly increased urine ANP and cGMP and plasma cGMP, and decreased plasma NT-proBNP, aldosterone and endothelin-1. Sacubitril and valsartan also blocked the AT1-receptor as evidenced by increased plasma renin activity and plasma renin concentrations. In PARADIGM-HF, sacubitril and valsartan decreased plasma NT-proBNP (not a neprilysin substrate) and increased plasma BNP (a neprilysin substrate) and urine cGMP compared with enalapril.
QT Prolongation: In a thorough QTc clinical study in healthy male subjects, single doses of sacubitril and valsartan 194 mg sacubitril/206 mg valsartan and 583 mg sacubitril/617 mg valsartan had no effect on cardiac repolarization.
Amyloid-β: Neprilysin is one of multiple enzymes involved in the clearance of Amyloid-β (Aβ) from the brain and cerebrospinal fluid (CSF). Administration of sacubitril and valsartan 194 mg sacubitril/206 mg valsartan once-daily for 2 weeks to healthy subjects was associated with an increase in CSF Aβ1-38 compared to placebo; there were no changes in concentrations of CSF Aβ1-40 or CSF Aβ1-42. The clinical relevance of this finding is unknown.
Blood Pressure: Addition of a 50 mg single dose of sildenafil to sacubitril and valsartan at steady state (194 mg sacubitril/206 mg valsartan mg once daily for 5 days) in patients with hypertension was associated with additional blood pressure (BP) reduction (~5/4 mmHg, systolic/diastolic BP) compared to administration of sacubitril and valsartan alone.
Co-administration of sacubitril and valsartan did not significantly alter the BP effect of intravenous nitroglycerin.
Pharmacokinetics
Absorption
Following oral administration, sacubitril and valsartan dissociates into sacubitril and valsartan. Sacubitril is further metabolized to LBQ657. The peak plasma concentrations of sacubitril, LBQ657, and valsartan are reached in 0.5 hours, 2 hours, and 1.5 hours, respectively. The oral absolute bioavailability of sacubitril is estimated to be ≥ 60%. The valsartan in sacubitril and valsartan is more bioavailable than the valsartan in other marketed tablet formulations; 26 mg, 51 mg, and 103 mg of valsartan in sacubitril and valsartan is equivalent to 40 mg, 80 mg, and 160 mg of valsartan in other marketed tablet formulations, respectively.
Following twice-daily dosing of sacubitril and valsartan, steady state levels of sacubitril, LBQ657, and valsartan are reached in 3 days. At steady state, sacubitril and valsartan do not accumulate significantly, whereas LBQ657 accumulates by 1.6-fold. Sacubitril and valsartan administration with food has no clinically significant effect on the systemic exposures of sacubitril, LBQ657, or valsartan. Although there is a decrease in exposure to valsartan when sacubitril and valsartan is administered with food, this decrease is not accompanied by a clinically significant reduction in the therapeutic effect. Sacubitril and valsartan can therefore be administered with or without food.
Distribution
Sacubitril, LBQ657, and valsartan are highly bound to plasma proteins (94% to 97%). Based on the comparison of plasma and CSF exposures, LBQ657 crosses the blood brain barrier to a limited extent (0.28%). The average apparent volumes of distribution of valsartan and sacubitril are 75 and 103 L, respectively.
Sacubitril is readily converted to LBQ657 by esterases; LBQ657 is not further metabolized to a significant extent. Valsartan is minimally metabolized; only about 20% of the dose is recovered as metabolites. A hydroxyl metabolite has been identified in plasma at low concentrations (< 10%).
Elimination
Following oral administration, 52% to 68% of sacubitril (primarily as LBQ657) and ~13% of valsartan and its metabolites are excreted in urine; 37% to 48% of sacubitril (primarily as LBQ657), and 86% of valsartan and its metabolites are excreted in feces. Sacubitril, LBQ657, and valsartan are eliminated from plasma with a mean elimination half-life (T1/2) of approximately 1.4 hours, 11.5 hours, and 9.9 hours, respectively.
Linearity/Nonlinearity
The pharmacokinetics of sacubitril, LBQ657, and valsartan were linear over an sacubitril and valsartan dose range of 24 mg sacubitril/26 mg valsartan to 194 mg sacubitril/206 mg valsartan.
Drug Interactions
Effect of co-administered drugs on sacubitril and valsartan: Because CYP450 enzyme-mediated metabolism of sacubitril and valsartan is minimal, coadministration with drugs that impact CYP450 enzymes is not expected to affect the pharmacokinetics of sacubitril and valsartan. Dedicated drug interaction studies demonstrated that coadministration of furosemide, warfarin, digoxin, carvedilol, a combination of levonorgestrel/ethinyl estradiol, amlodipine, omeprazole, hydrochlorothiazide (HCTZ), metformin, atorvastatin, and sildenafil, did not alter the systemic exposure to sacubitril, LBQ657 or valsartan.
Effect of sacubitril and valsartan on co-administered drugs: In vitro data indicate that sacubitril inhibits OATP1B1 and OATP1B3 transporters. The effects of sacubitril and valsartan on the pharmacokinetics of coadministered drugs are summarized in Figure 1.
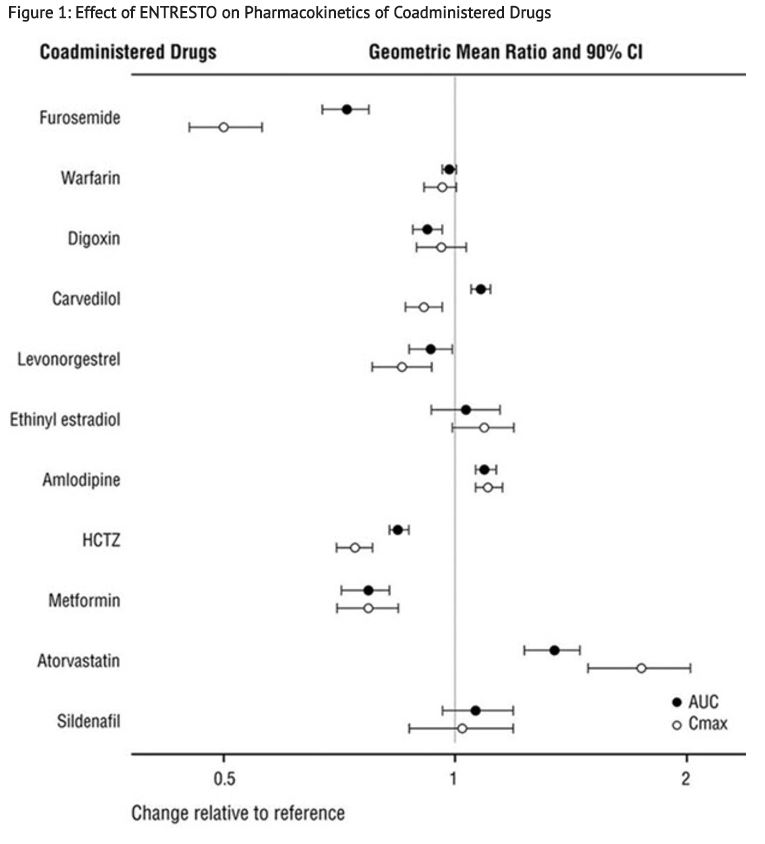
Specific Populations
Effect of specific populations on the pharmacokinetics of LBQ657 and valsartan are shown in Figure 2.
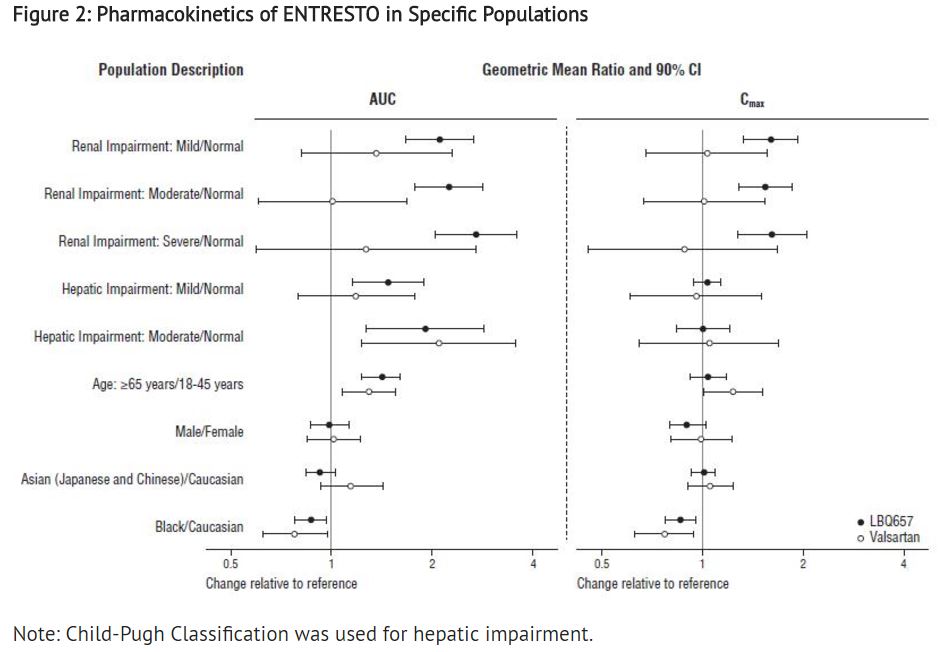
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis: Carcinogenicity studies conducted in mice and rats with sacubitril and valsartan did not identify any carcinogenic potential for sacubitril and valsartan. The LBQ657 Cmax at the high dose (HD) of 1200 mg/kg/day in male and female mice was, respectively, 14 and 16 times that in humans at the MRHD. The LBQ657 Cmax in male and female rats at the HD of 400 mg/kg/day was, respectively, 1.7 and 3.5 times that at the MRHD. The doses of valsartan studied (high dose of 160 and 200 mg/kg/day in mice and rats, respectively) were about 4 and 10 times, respectively, the MRHD on a mg/m2 basis. Mutagenicity and clastogenicity studies conducted with sacubitril and valsartan, sacubitril, and valsartan did not reveal any effects at either the gene or chromosome level.
Impairment of Fertility: Sacubitril and valsartan did not show any effects on fertility in rats up to a dose of 73 mg sacubitril/77 mg valsartan/kg/day (≤1.0-fold and ≤ 0.18-fold the MRHD on the basis of the AUCs of valsartan and LBQ657, respectively).
Animal Toxicology and/or Pharmacology
The effects of sacubitril and valsartan on Amyloid-β concentrations in CSF and brain tissue were assessed in young (2 to 4 years old) cynomolgus monkeys treated with sacubitril and valsartan (24 mg sacubitril/26 mg valsartan/kg/day) for 2 weeks. In this study, sacubitril and valsartan affected CSF Amyloid-β clearance, increasing CSF Amyloid-β 1-40, 1-42, and 1-38 levels in CSF; there was no corresponding increase in Amyloid-β levels in the brain. In addition, in a toxicology study in cynomolgus monkeys treated with sacubitril and valsartan at 146 mg sacubitril/154 mg valsartan/kg/day for 39-weeks, there was no Amyloid-β accumulation in the brain.
Clinical Studies
Dosing in clinical trials was based on the total amount of both components of sacubitril and valsartan, i.e., 24/26 mg, 49/51 mg and 97/103 mg were referred to as 50 mg, 100 mg, and 200 mg, respectively.
PARADIGM-HF
PARADIGM-HF was a multinational, randomized, double-blind trial comparing sacubitril and valsartan and enalapril in 8,442 adult patients with symptomatic chronic heart failure (NYHA Class II–IV) and systolic dysfunction (left ventricular ejection fraction ≤ 40%). Patients had to have been on an ACE inhibitor or ARB for at least four weeks and on maximally tolerated doses of beta-blockers. Patients with a systolic blood pressure of < 100 mmHg at screening were excluded.
The primary objective of PARADIGM-HF was to determine whether sacubitril and valsartan, a combination of sacubitril and a RAS inhibitor (valsartan), was superior to a RAS inhibitor (enalapril) alone in reducing the risk of the combined endpoint of cardiovascular (CV) death or hospitalization for heart failure (HF).
After discontinuing their existing ACE inhibitor or ARB therapy, patients entered sequential single-blind run-in periods during which they received enalapril 10 mg twice-daily, followed by sacubitril and valsartan 100 mg twice-daily, increasing to 200 mg twice daily. Patients who successfully completed the sequential run-in periods were randomized to receive either sacubitril and valsartan 200 mg (N=4,209) twice-daily or enalapril 10 mg (N=4,233) twice-daily. The primary endpoint was the first event in the composite of CV death or hospitalization for HF. The median follow-up duration was 27 months and patients were treated for up to 4.3 years.
The population was 66% Caucasian, 18% Asian, and 5% Black; the mean age was 64 years and 78% were male. At randomization, 70% of patients were NYHA Class II, 24% were NYHA Class III, and 0.7% were NYHA Class IV. The mean left ventricular ejection fraction was 29%. The underlying cause of heart failure was coronary artery disease in 60% of patients; 71% had a history of hypertension, 43% had a history of myocardial infarction, 37% had an eGFR < 60 mL/min/1.73m2, and 35% had diabetes mellitus. Most patients were taking beta-blockers (94%), mineralocorticoid antagonists (58%), and diuretics (82%). Few patients had an implantable cardioverter-defibrillator (ICD) or cardiac resynchronization therapy-defibrillator (CRT-D) (15%).
PARADIGM-HF demonstrated that sacubitril and valsartan, a combination of sacubitril and a RAS inhibitor (valsartan), was superior to a RAS inhibitor (enalapril), in reducing the risk of the combined endpoint of cardiovascular death or hospitalization for heart failure, based on a time-to-event analysis (hazard ratio [HR]: 0.80, 95% confidence interval [CI], 0.73, 0.87, p <0.0001). The treatment effect reflected a reduction in both cardiovascular death and heart failure hospitalization; see Table 2 and Figure 3. Sudden death accounted for 45% of cardiovascular deaths, followed by pump failure, which accounted for 26%.
Sacubitril and valsartan also improved overall survival (HR 0.84; 95% CI [0.76, 0.93], p = 0.0009) (Table 2). This finding was driven entirely by a lower incidence of cardiovascular mortality on sacubitril and valsartan.
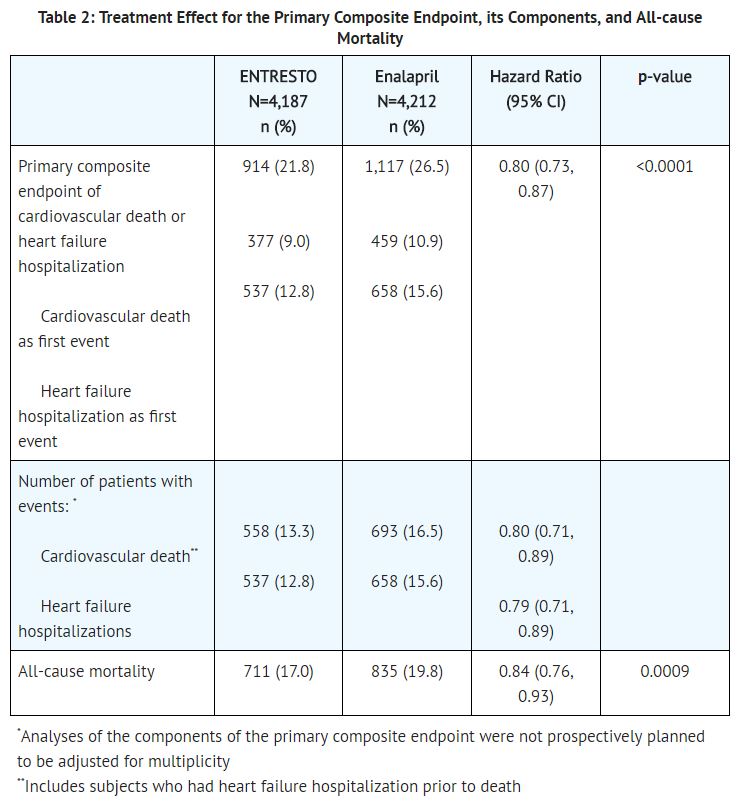
The Kaplan-Meier curves presented below (Figure 3) show time to first occurrence of the primary composite endpoint (3A), and time to occurrence of cardiovascular death at any time (3B) and first heart failure hospitalization (3C).
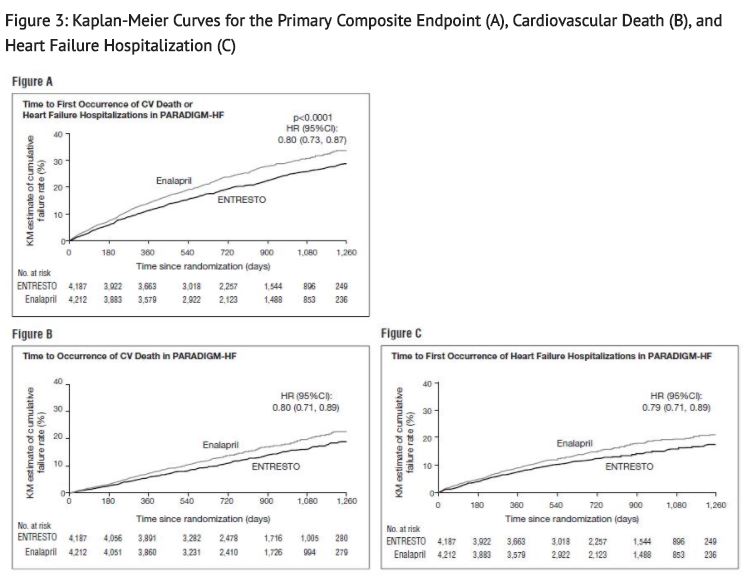
A wide range of demographic characteristics, baseline disease characteristics, and baseline concomitant medications were examined for their influence on outcomes. The results of the primary composite endpoint were consistent across the subgroups examined (Figure 4).
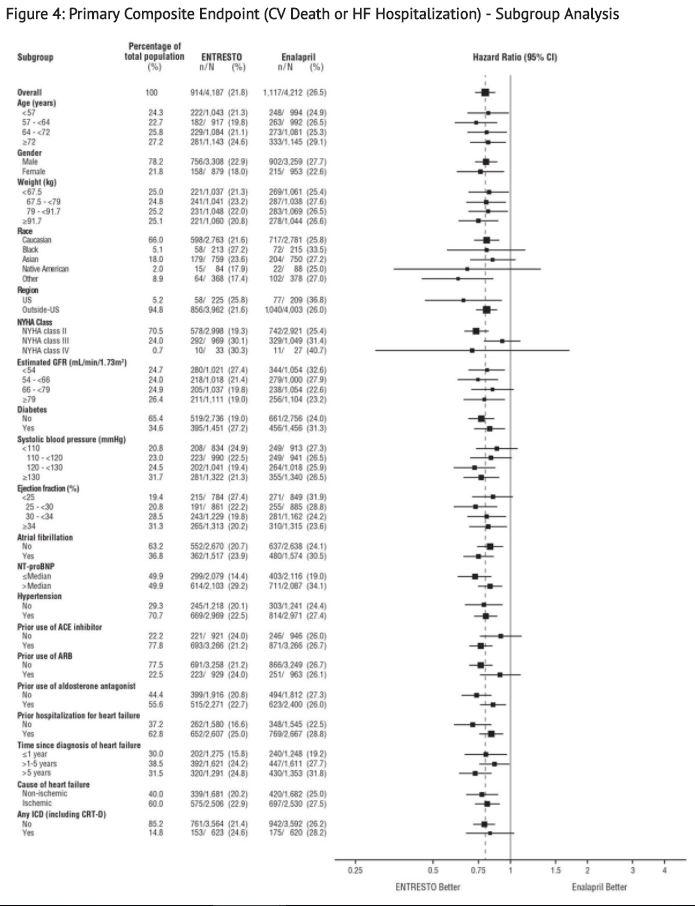
Note: The figure above presents effects in various subgroups, all of which are baseline characteristics. The 95% confidence limits that are shown do not take into account the number of comparisons made, and may not reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
How Supplied
Sacubitril and valsartan is available as unscored, ovaloid, biconvex, film-coated tablets, containing 24 mg of sacubitril and 26 mg of valsartan; 49 mg of sacubitril and 51 mg of valsartan; and 97 mg of sacubitril and 103 mg of valsartan. All strengths are packaged in bottles and unit dose blister packages (10 strips of 10 tablets) as described below.
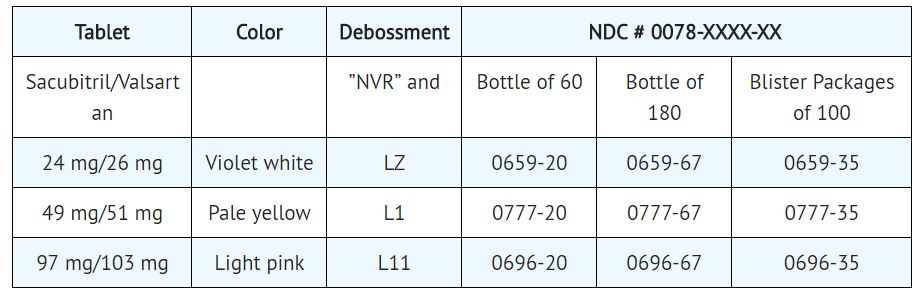
Storage
Store at 25°C (77°F) with excursions between 15°C and 30°C (59°F and 86°F) permitted. Protect from moisture.
Images
Drug Images
{{#ask: Page Name::Sacubitril and Valsartan |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
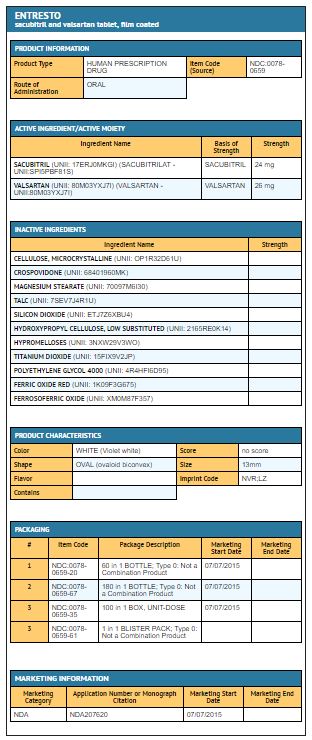
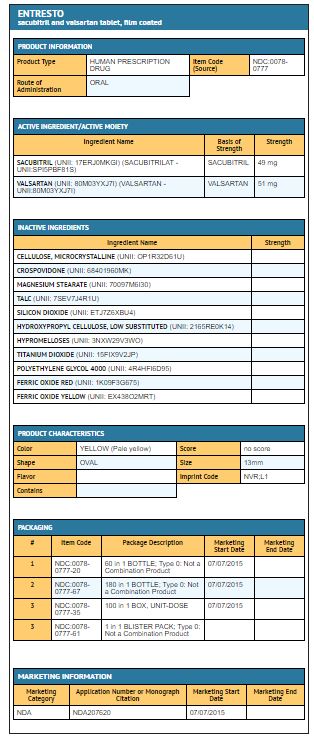
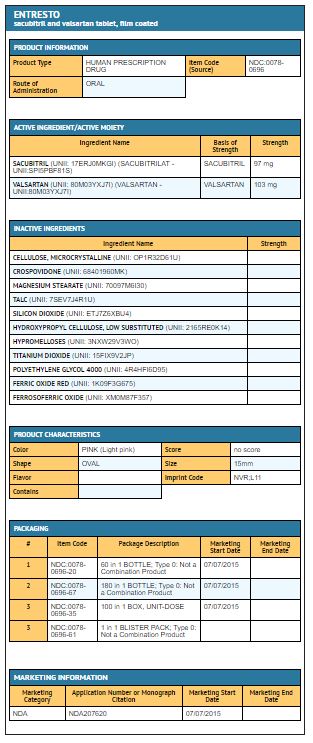
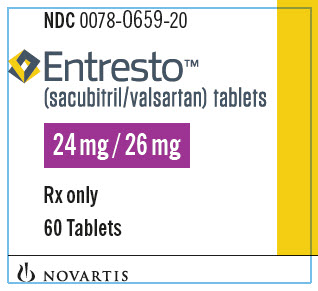
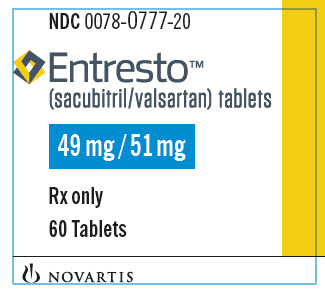
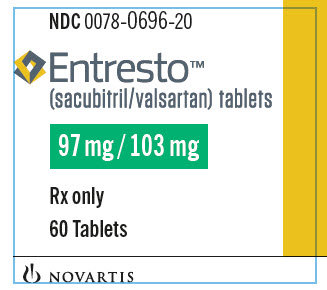
{{#ask: Label Page::Sacubitril and Valsartan |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise patients to read the FDA-approved patient labeling (Patient Information).
Pregnancy: Advise female patients of childbearing age about the consequences of exposure to sacubitril and valsartan during pregnancy. Discuss treatment options with women planning to become pregnant. Ask patients to report pregnancies to their physicians as soon as possible.
Angioedema: Advise patients to discontinue use of their previous ACE inhibitor or ARB. Advise patients to allow a 36 hour wash-out period if switching from or to an ACE inhibitor.
Precautions with Alcohol
Alcohol-Sacubitril and Valsartan interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
ENTRESTO
Look-Alike Drug Names
There is limited information regarding Sacubitril and Valsartan Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.