Angiotensin II receptor antagonist
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Angiotensin II receptor antagonists, also known as angiotensin receptor blockers (ARBs), AT1-receptor antagonists or sartans, are a group of pharmaceuticals which modulate the renin-angiotensin-aldosterone system. Their main use is in hypertension (high blood pressure), diabetic nephropathy (kidney damage due to diabetes) and congestive heart failure.
Mode of action
These substances are AT1-receptor antagonists – that is, they block the activation of angiotensin II AT1 receptors. Blockade of AT1 receptors directly causes vasodilation, reduces secretion of vasopressin, reduces production and secretion of aldosterone, amongst other actions – the combined effect of which is reduction of blood pressure.
The specific efficacy of each ARB within this class is made up of a combination of three pharmacodynamic and pharmacokinetic parameters. These areas are: 1) Pressor inhibition (at trough or the 24th hour) this clinically important measurement relates to the amount of blockade or inhibition of the BP raising effect of angiotension II. The rates as listed in the US FDA Package Inserts for inhibition of this effect at the 24th hour for the ARBs are as follows: (all doses listed in PI are included)
- Valsartan 80mg 30%
- Telmisartan 80mg 40%
- Losartan 100mg 25- 40%
- Irbesartan 150mg 40%
- Irbesartan 300mg 60%
- Olmesartan 20mg 61%
- Olmesartan 40mg 74%
2) AT1 affinity, AT1 affinity vs AT2 is the second meaningful area out of three that make up the efficacy of an individual ARB. The specific AT1 affinity relates to how specificially attracted the medicine is for the correct receptor, the US FDA Package Insert rates for AT1 affinity are as follows:
- Losartan 1000 fold
- Telmisartan 3000 fold
- Irbesartan 8500 fold
- Olmesartan 12500 fold
- Valsartan 20000 fold
3) The third area that completes the overall efficacy picture of an ARB is half life. Half life is an indicator of how many hours it takes for half the medicine to still be effective. The rates from the US FDA Package Inserts are as follows:
- Valsartan 6
- Losartan 6- 9
- Irbesartan 11- 15
- Olmesartan 13
- Telmisartan 24
Based on the above data for the three key PD/ PK areas that indicate efficacy it is important to see that you need a combination of all three at an effective level.
Uses
Angiotensin II receptor antagonists are primarily used for the treatment of hypertension where the patient is intolerant of ACE inhibitor therapy. They do not inhibit the breakdown of bradykinin or other kinins, and are thus only rarely associated with the persistent dry cough and/or angioedema that limit ACE inhibitor therapy. More recently, they have been used for the treatment of heart failure in patients intolerant of ACE inhibitor therapy, particularly candesartan. Irbesartan and losartan have trial data showing benefit in hypertensive patients with type II diabetes, and may delay the progression of diabetic nephropathy. Candesartan is used experimentally in preventive treatment of migraine.[1] Another angiotensin II receptor antagonist, olmesartan, is an important part of the Marshall Protocol, invented by American biomedical researcher Trevor Marshall.
The angiotensin II receptor blockers have differing potencies in relation to blood pressure control, with statistically differing blood pressure effects at the maximal doses.[2] When used in clinical practice, the particular agent used may vary based on the degree of blood pressure response required. one
Adverse effects
This class of drugs is usually well-tolerated, with common adverse drug reactions (ADRs) including: dizziness, headache, and/or hyperkalemia. Infrequent ADRs associated with therapy include: first dose orthostatic hypotension, rash, diarrhea, dyspepsia, abnormal liver function, muscle cramp, myalgia, back pain, insomnia, decreased haemoglobin levels, renal impairment, pharyngitis, and/or nasal congestion. (Rossi, 2006)
While one of the main rationales for the use of this class is the avoidance of dry cough and/or angioedema associated with ACE inhibitor therapy, they may still rarely occur. Additionally, there is also a small risk of cross-reactivity in patients who have experienced angioedema with ACE inhibitor therapy. (Rossi, 2006)
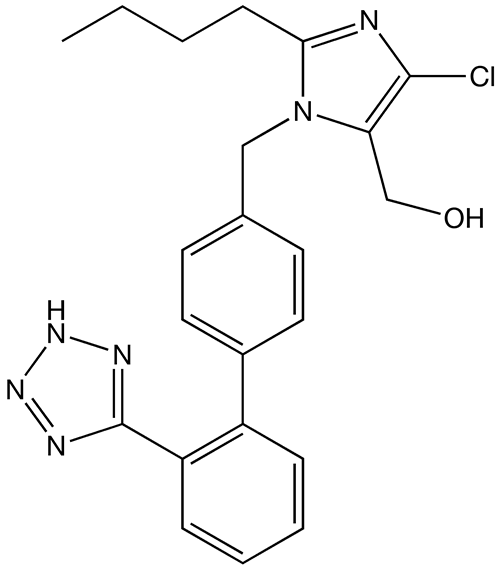
Members
References
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006.
- Cough and Angioedema From ACE Inhibitors
- ↑ Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G. (2003). "Prophylactic treatment of migraine with an angiotensin II receptor blocker: a randomized controlled trial". JAMA. 1 (289 Pt 1): 65–9. PMID 12503978.
- ↑ Kassler-Taub K, Littlejohn T, Elliott W, Ruddy T, Adler E. (1998). "Comparative efficacy of two angiotensin II receptor antagonists, irbesartan and losartan in mild-to-moderate hypertension. Irbesartan/Losartan Study Investigators". Am J Hypertens. 11 (4 Pt 1): 445–53. PMID 9607383.