Rheumatic fever: Difference between revisions
No edit summary |
No edit summary |
||
| Line 94: | Line 94: | ||
*[[Abdominal pain]] | *[[Abdominal pain]] | ||
*[[Nosebleed]]s | *[[Nosebleed]]s | ||
* [[neurological pain such as lumbago or low back pain]] | *[[neurological pain such as lumbago or low back pain]] | ||
* [[delirium, stupor, seizures, coma]] | *[[delirium, stupor, seizures, coma]] | ||
* [[renal failure]] | *[[renal failure]] | ||
* [[pulmonary edema]] | *[[pulmonary edema]] | ||
* [[ruddiness of the skin secondary to rheumatic vasculitis] | *[[ruddiness of the skin secondary to rheumatic vasculitis]] | ||
* [[ruddiness and swelling of the face and neck secondary to jugular system | *[[ruddiness and swelling of the face and neck secondary to jugular system congestion itself secondary to rheumatic carditis and acute, congestive heart failure]] | ||
*[[rheumatic pneumonitis causing a congestive lung condition]] | |||
* [[rheumatic pneumonitis causing a congestive lung condition]] | |||
Unfortunately, since the 1930's, most physicians in modern western countries have dealt with fewer and fewer cases of rheumatic fever so at this time only the very most high-grade cases can be recognized and the symptoms and signs of those cases are what compose the "Jones Criteria". Even with the Jones Criteria having existed for decades, most cases of rheumatic fever suffer from mis-diagnosis, because most physicians simply do not think that rheumatic fever exists in modern, western countries including the USA. Out of mind out of sight is the rule. | Unfortunately, since the 1930's, most physicians in modern western countries have dealt with fewer and fewer cases of rheumatic fever so at this time only the very most high-grade cases can be recognized and the symptoms and signs of those cases are what compose the "Jones Criteria". Even with the Jones Criteria having existed for decades, most cases of rheumatic fever suffer from mis-diagnosis, because most physicians simply do not think that rheumatic fever exists in modern, western countries including the USA. Out of mind out of sight is the rule. | ||
Revision as of 04:10, 22 August 2011
For patient information click here
| Rheumatic fever | |
 | |
|---|---|
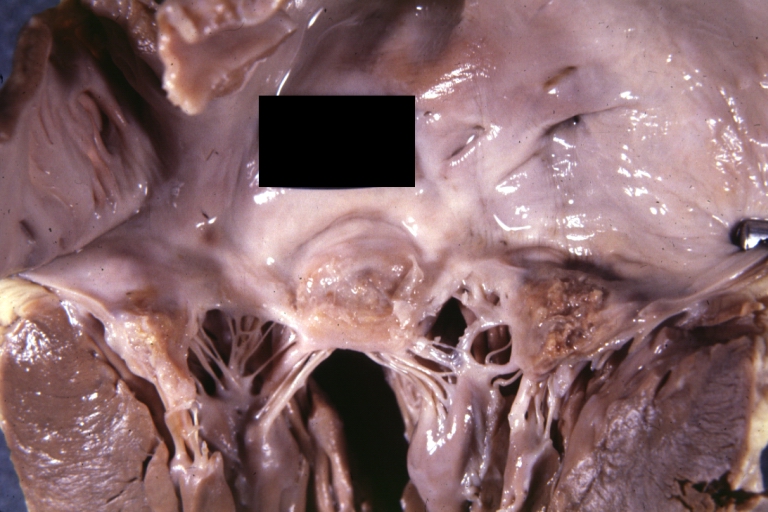
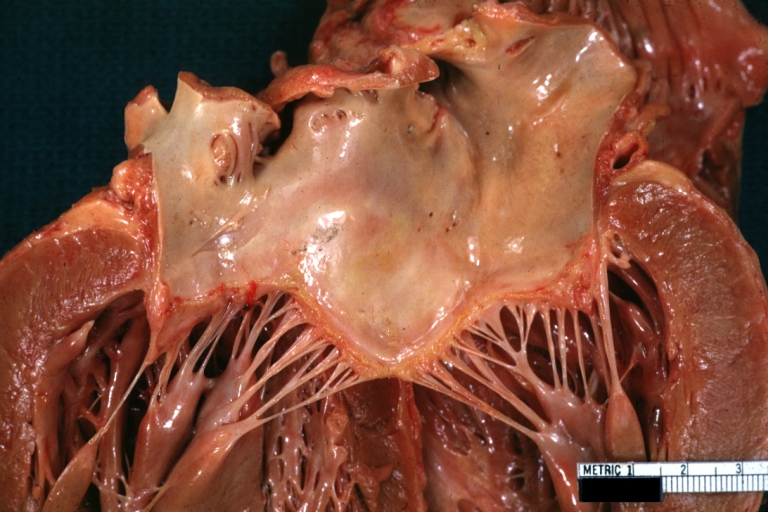
| Rheumatic Mitral Valvulitis: Gross; an excellent example of acute rheumatic fever lesion along line of closure of mitral valve Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | I00-I02 |
| ICD-9 | 390–392 |
| DiseasesDB | 11487 |
| MedlinePlus | 003940 |
| MeSH | D012213 |
|
WikiDoc Resources for Rheumatic fever |
|
Articles |
|---|
|
Most recent articles on Rheumatic fever Most cited articles on Rheumatic fever |
|
Media |
|
Powerpoint slides on Rheumatic fever |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Rheumatic fever at Clinical Trials.gov Trial results on Rheumatic fever Clinical Trials on Rheumatic fever at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Rheumatic fever NICE Guidance on Rheumatic fever
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Rheumatic fever Discussion groups on Rheumatic fever Patient Handouts on Rheumatic fever Directions to Hospitals Treating Rheumatic fever Risk calculators and risk factors for Rheumatic fever
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Rheumatic fever |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss Rheumatic fever further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Lance Christiansen, D.O.; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
The systemic signs and symptoms of rheumatic fever are caused by a systemic attack on a human host's tissues, and therefore organs, by autoantibodies and other autoimmunological elements that are self-developed, after a Streptococcus pyogenic sensitized patient experiences an additional infection by a virulent strain of Streptococcus pyogenes.
In order to develop an acute, rheumatic, response, a host must be autoimmunologically sensitized to Streptococcus pyogene's autoantigens and secreted toxic products from a number of prior, timely infections by Streptococcus pyogenes. A rheumatic fever episode is primarily an autoimmunological, non-suppurative sequela of a virulent Streptococcus pyogenes infection and not a function of direct pathological, suppurative damage from the bacterial infection itself.
General information
Rheumatic fever, and therefore Streptococus pyogenes infections, are endemic in all areas of the world. In countries affected by the industrial revolution, domestic living conditons became less crowded, due to the development of larger homes and families had fewer children. In addition, iving conditions became, generally, more hygienic. The introduction of antibiotics, first sulfonamide in the early 1930's and then penicillin in the 1940's, further caused Streptococcus pyogenes infections to become less common and less severe in economically developed countries although they never disappeared.
Rheumatic fever was a scorge of society for hundreds of years, until the post WW II era, for in the text, Rheumatic Fever and Streptococcal Infection (Massell, B., Harvard Press, 1997)the author indicates, "For the period 1939-1943, statistics published by the Metropolitan Life Insurance Company indicated that rheumatic fever was the leading cause of death among policy holders for persons from five to nineteen years of age and the second leading fatal disease among twenty to twenty-four year olds."
The indicence of rheumatic fever had been decreasing, as society became more wealthy, as the industrial revolution progressed and by the late 1960's it seemed that rheumatic fever has nearly disappeared. Rheumatic fever became so undommon in economically developed countries that physicians, in general, lost their clinical knowledge of the disease.
Rheuamtic fever has been a puzzling disease for a long period and it was not until 1931 that Alvin Coburn, MD determined, for sure, that Streptococcus pyogenes infections caused its development. It was not until the 1950's that all physicians agreed that Streptococcus pyogenes was its cause. Even T. Duckett Jones, MD, the physician who first developed the Jones Criteria, did not accept the fact that Streptococcus pyogenes was the sole cause of rheumatic fever.
It was first thought that individuals developed an allergic response to the bacteria, but later it was determined that rheumatic fever was an autoimmunological sequela to a virulent Streptococcus pyogenes infection in a patient who had adequate rheumatic sensitivity from prior infections by Streptococcus pyogenes.
The development of a rheumatic fever episode depends on the involved host being highly autoimmunologically sensitized to autoantigens exhibited by Streptococcus pyogenes to its host during prior Streptococcus pyogenes infectious episodes, so a decrease in the frequency and virulence of infections by Streptococcus pyogenes in a society can cause rheumatic fever, as a disease entity, to be less frequent and less severe.
In north America, western Europe, Japan, much of Australia and New Zealand rheumatic fever became very uncommon. It decreased in frequency in modern western societies in a progressive fashion from the early 1900's, but it decreased remarkably after WW II so by 1970 it was thought to be a very rare disease in the USA, for instance, but it never disappeared. In certain populations such as the aboriginies of Austrialia and New Zealand it remained common and it also remained common in the aborigines of North America although it is not mentioned frequently in medical literature.
Rheumatic fever affects individuals who are thought to be "young and healthy", for instance, individuals between four years and fifty years of age, but during most eras rheumatic fever was most commonly noted in individuals between the six and thirty. The reason children younger than four years of age, or so, do not usually develop rheumatic fever is that an individual must have sufficient, prior stimulation by Streptococcus pyogens autoantigens, which is, typically, caused by multiple infections by Streptococcus pyogenes, over a relatively short period of time, and that situation is less likely to occur in younger children (although it does happen!). Older individuals are expected, somewhat, to develop diseases of aging and so it is often not surprising when they become sick; it is surprising when individuals in their teens, twenties, thirties, forties and even fifties, for instance, become very sick so those cases attract more "medical" attention. Individuals of all ages, however, can develop rheumatic fever.
Scarlet fever and rheumatic fever are, primarily, the same disease. The somewhat typical rash of scarlet fever develops if an individual contracts an infecton from a strain of Streptococcus pyogenes that secretes erythrotoxin A, B, and C, and if the individual involved has not had an infection by that particular strain previously, since during a previous infection antibodies will have been developed against the erythrogenic toxin of interest. Repeated infections by strains of Streptococcus pyogenes that have, and do not have, erythrotoxin A, B, and C can reinforce each other in the development of autoimmunological reactions by a host, since they all have certain autoantigens and secreted toxic products, other than erythrotoxin A, B, and C, in commonk. If a person, usually a child, develops an infection from Streptococcus pyogenes that secretes A, B, or C erythrotixin they will develop a mild infectious/autoimmunological disease and the classic, mild rash of scarletina, the diminuative term for scarlet fever, will often develop.
Since the development of rheumatic fever depends upon a prior, high-level of autoimmunological stimulation, which itself depends upon an individual, in the past, experiencing many infectious episodes by Streptococcus pyogenes, and since Streptococcus pyogenes are endemic in human and domestic animal populations (information from the Russian Encyclopedia (V.Nasonova,E. Talahaev), it must be understood that all individuals experience pathological, autoimmunological stimulation during Streptococcus pyogenes infections.
The rate of development of rheumatic fever, in a somewhat homogeneous population, will depend upon the environmental conditions mentioned above, wherein crowding and unhygienic living conditions are two of the most important. Information in the text Streptococcal Infections (Stevens, D., Kaplan, E., Oxford University Press, 2000) indicate that 1% to 70% of individuals in various populations are carriers of Streptococcus pyogenes and many of them are asymptomatic carriers. Perhaps, 2% to 4% of individuals who contract Streptoccus pyogenes infections develop recognizable rheumatic fever (but most mild cases go unrecognized) and of those, a low percentage, about 1% to 3% die from rheumatic fever. The incidence of rheumatic fever depends, to a great degree, upon the general level of Streptococcal pyogenic, autoimmunological sensitivity that exists within members of a given population.
Contrary to the immunological protection developed by humans during most infections, infections by Streptococcus pyogenes cause both a protective immunological and a pathological autoimmunological stimulation and so repeated infections by Streptococcus pyogenes will cause both a heightened protective immune, and pathological autoimmune response. The immune response causes Streptococcus pyogenes to be controlled, but the concomitant, autoimmunological response causes an inflammatory, systemic, disease process to be developed within the affected individual. The systemic, inflammatory, autoimmunological disease process is termed rheumatic fever and it is a sequela of both the virulent, triggering Streptococcus pyogenes infection and the prior infections that the individual developed that caused them to have elevated autoimmunological sensitivity to Streptococcus pyogenes' autoantigens.
If an individual develops rheumatic fever, they will experience the development of increased sensitization to Streptococcus pyogenes autoantigens. An infection by a virulent strain of Streptococcus pyogenes, at a later date, will likely cause an elevated, autoimmunological response and a recurrent case, probably a more severe case, of rheumatic fever will develop.
If an individual does not contract a Streptococcus pyogenes infection for a long period, perhaps for five years or longer, an individual's immunological/autoimmunological responsivness will naturally decrease and, perhaps, there will be less chance of developing rheumatic fever if the individual contracts a future Streptococcus pyogenes infection.
The above natural phenomenon is the basis for the use of prophylactic penicillin therapy for individuals, and populations of individuals, who are at risk for rheumatic fever. Providing individuals who have had rheumatic fever with monthly (or maybe every three weeks) injections of Benzathine Penicillin G, 1,200,000 units, or oral penicillin VK or G, 250mg twice daily (I think 500 mg twice daily is more efficacious), decreases the frequency of recurrent Streptococcus pyogenes infections and therefore recurrent rheumatic fever episodes. It is estimated that the recurrence rate of rheumatic fever is decreased about 85% by providing prophylactic penicillin therapy.
Streptococcus pyogenes is a complex microorganism and it causes many disease entities both from the suppurative aspect of Streptococcus pyogenes infections and from nonsuppurative, systemic, autoimmunological sequelae to the infections. The nonsuppurative, systemic, autoimmunological sequelae are inflammatory in nature and therefore all tissues and organs are affected, but certain organs are noted to be affected in an important and acute fashion: the heart, kidneys and brain.
Since the heart, kidneys and brain are vital organs, and their functional abnormalities causes obvious clinical abnormalities, and even death, to individuals, acute rheumatic abnormalities to the heart, kidneys and brain, that individuals experience, are medically-noted more frequently than acute rheumatic damage to other organs. The symptoms and signs of acute rheumatic fever, however, indicates that virtually all tissues, and therefore organs, of the body are affected: connective tissue (arthritis); lethargy, stupor, seizures, coma, post-disease fatigue, tics, chorea, chronic mental disturbances such as obsessive-compulsive behavior and PANDAS(rheumatic encephalomyelitis); acute rheumatic myocarditis,endocarditis, pericarditis and cardiac arrhythmias with the myocarditis and endocarditis causing cardiac failure and pulmonary edema (the heart); autoimmune pneumonitis (the lungs); rheumatic, vasculitic renal failure (kidneys); erythema marginatum, papulatum, miliary rash, purpura, petechiae, and scarlet fever rash (the skin); anemia, including aplastic anemia (bone marrow); autoimmune hepatitis (the liver); acute, peripheral, painful neuropathies (peripheral nerves); nausea, vomiting, diarrhea, crampy abdominal pain (gastrointestinal organs); other organs such as the pancreas, endocrine organs, and elements of the circulatory system are also affected. Since rheumatic fever is, basically and initially, an autoimmune inflammatory disorder, and the autoimmunological elements travel throughout the body via the circulatory system. Vascular elements, arteries, arterioles, capillaries, venules, veins and lymph vessels are attracked initially and in that way rheuamtic fever becomes a systemic disease process.
Information in modern texts has emphasized for many decades the affect of rheumatic fever on the heart, because its inflammatory, autoimmunological effects are exacerbated in that organ, and since the heart is a vital organ the clinical ramifications are easily noted. The reason that rheumatic autoimmunity is exacerbated in the heart's tissues is because the cyclic, physiological compression developed by the heart also causes an elevated vascular triple response of Lewis phenomenon within the heart's tissues. The triple response of Lewis phenomenon is usually thought to be a dermatological concept since it can be elicited by stroking the skin of most individuals. Those who have elevated Streptococcus pyogenic autoimmunity exhibit a very high-grade triple response of Lewis phenomenon dermatologically. Surpisingly, the triple response of Lewis phenomenon that all people exhibit indicates that all people have, at least, a low-level of rheuamtic autoimmunity (from personal research).
More important, perhaps, are the more chronic, inflammatory, autoimmunologial disease states, which have not been well appreciated in modern times, but which were understood, at least to some degree, during prior eras. Rheumatic fever, an acute, inflammatory, autoimmune disease state was, from the mid-1600's at least, when Sydemham discribed rheumatic fever reasonably accurately, until the early 1900's was termed, often, acute rheumatism or acute articular rheumatism. The chronic disease state of rheumatic, inflammatory autoimmunity was termed chronic rheumatism or simply, rheumatism. Galen, during the second century A.D. coined the word, rheumatismos, and it was first used in post-renaissance times by Guillaume Bailou (1538-1616)(Rheumatic Fever and Streptococcal Infections, cited above).
The chronic non-suppurative target-organ manifestions of rheumatic fever, rheumatic heart-valve disease, is not caused by acute rheumatic fever, but it is due to a reasonably elevated, chronic, inflammatory, rheumatic, autoimmune state, which is caused by repeated, or at times chronic, infections by virulent strains of Streptococcus pyogenes. Rheumatic heart-valve disease is common in American society, but there is no outcry from treating cardiologists, and cardiac surgeons, concerning the ongoing development of the high-grade, chronic, rheumatic state within individuals in the American population.
Sir William Osler, in his famous text, Osler's Principles and Practice of Medicine, Twelfth Edition (McCrea, T, D. Appleton-Century Company, 1935) indicates that rheumatic fever can exist in the typically understood classic high-grade presentation (some of the signs and symptoms thereof are listed in the Jones Criteria), as subacute rheumatic fever, and as rheumatic fever of the less than subacute variety. Osler indicates the following: "Subacute rheumatic fever represents a milder form of the disease, in which all the symptoms are less pronounced. The fever rarely rises abo e 101 deg. F.; fewer joints are involved; and the arthritis is less intense. The cases may drag on for weeks or months. It should not be forgotten that mild or subacute forms may be associated with endocarditis or pericarditis...in young children there may not be any pronounced arthritis or any arthritis at all, and the discovery of endocarditis often suggests the diagnosis. Endocariditis and myocarditis are the prominent features in children in whom the picture may be very variable...The onset may be so insidious that it can hardly be termed even subacute. Ill health without any evident cause, loss of weight, anorexia, fatigue, complaint of slight pains and fever with no apparent cause should suggest the possibility." As an example of the "...complaint of slight pains...", mentioned in the above quote, growing pains, that many younger people have, is a sign of mild, semi-chronic rheuamtic fiver.
Diagnosis of Rheumatic Fever The diagnosis of rheumatic fever has been historically difficult, but certain physicians, since the 1500's, understood, at least in part, the complex of signs and symptoms that indicate its existence. Thomas Sydenham discribed a case of severe rheumatic fever in the late 1600's and a similar discription is provided in the Encyclopedia Britanica's first edition published in 1771: "The rheumatism chiefly attacks persons in the flower of their age, after violent exercise, or a great heat of the body from any other cause, and then being too suddenly cooled; but spares neither men nor women, old nor young...It begins with chiliness and shivering, followed by inquietude and thirst. Which is preceded with spontaneous lassitude, a heaviness of the joints, and coldness of the extreme parts. When the fever appears, there is an inward heat, chiefly about the praecordia, attended with anxiety. The pulse is quick and strait, the appetite is lost, and the body is coftive. In a day or two, sometimes sooner, the patient feels a racking pain, sometimes in one joint, sometimes in another, but more frequently in the wrists, shoulders and knees; frequently shifting from place to place, and leaving redness and swelling in the part visited last. The pain is exasperated upon the least motion; it sometimes attacks the loins and the coxendix. When it seizes the loins, it is called the lumbago; and there is a most violent pain in the small of the back, which sometimes extends to the os sacrum, and is like fit of the gravel...it may continue for months or years, but not always with the same violence, but by fits. If it continues and increases, it may cause a stiff joint, which will scarce yield to any remedy." Further,"Its proximate cause seems to be the inflammation of the lymphatic arteries." And finally, "The chronic rheumatism is either the remains of a rheumatic fever, or a continuation of pains that proceeded at first from lesser but neglected colds."
The above quote is very important for it specifies that since the late 1700's physicians knew that a contagion caused acute rheuamtism, also termed, a rheumatic fever, but also that it caused chronic rheumatism. At times the word, rheumatism, was used as a general term for both acute rheumatism and chronic rheumatism since certain physicians from the time of Galen knew that a respiratory disease, which caused the development of "a defluxion of rheum", phlegm (Rheum means, "to flow or to flow down" in Greek), would cause a painful systemic malady in humankind. Galen, in fact, coined the word rheumatismos about 200 AD.
As rheumatic fever slowly, but progressively became less common after about 1850, as the advances of the industrial revolution were instituted into economically developed societies, especially after 1900, high-grade cases of rheumatic fever became less common in modernized parts of the world. Fewer physicians took care of patients with severe rheumatic fever so it slowly became difficult to diagnose, even in the late 1930's, by modern, western-educated physicians. One might think that physicians in modern countries have the least experience and therefore the least knowledge about rheumatic fever, however, they often have advanced knowledge about other aspects of medical science.
During WW II, conditions of over-crowding developed in military training sites, and at sites of war-making activities, so rheumatic fever, as a disease entity, became more common in that environment. Leaders in the U.S. Navy Medical Corps hired T. Duckett Jones, MD, an investigator in the area of rheumatic fever, to study rheumatic fever's epidemiology and clinical development. Dr. Jones, eventually, devised certain sign and symptom criteria to provide an aid for diagnosing rheumatic fever. Those diagnostic criteria were published in the following text, (Jones,T.D., Journal of the American Medical Association|JAMA], 1944; 126:481–484) and have become known as the "Jones Criteria". They are still currently used, in a modified form, to diagnose rheumatic fever. They have been periodically revised by the American Heart Association in collaboration with other groups.[1] Two major criteria, or one major and two minor criteria, when there is also evidence of a previous strep infection, support the diagnosis of rheumatic fever.[2][3]
Major criteria
- Carditis: inflammation of the heart muscle which can manifest as congestive heart failure with shortness of breath, pericarditis with a rub, or a new heart murmur.
- Migratory polyarthritis: a temporary migrating inflammation of the large joints, usually starting in the legs and migrating upwards.
- Sydenham's chorea (St. Vitus' dance): a characteristic series of rapid movements without purpose of the face and arms. This can occur very late in the disease.
- Erythema marginatum: a long lasting rash that begins on the trunk or arms as macules and spread outward to form a snakelike ring while clearing in the middle. This rash never starts on the face and is made worse with heat.
- Subcutaneous nodules (a form of Aschoff bodies): painless, firm collections of collagen fibers on the back of the wrist, the outside elbow, and the front of the knees. These now occur infrequently.
Minor criteria
- Fever: temperature elevation
- Arthralgia: Joint pain without swelling
- Laboratory abnormalities: increased Erythrocyte sedimentation rate, increased C reactive protein, leukocytosis
- Electrocardiogram abnormalities: a prolonged PR interval
- Evidence of Group A Strep infection: positive culture for Group A Strep, elevated or rising Antistreptolysin O titre
- Previous rheumatic fever or inactive heart disease
Other signs and symptoms
- Abdominal pain
- Nosebleeds
- neurological pain such as lumbago or low back pain
- delirium, stupor, seizures, coma
- renal failure
- pulmonary edema
- ruddiness of the skin secondary to rheumatic vasculitis
- ruddiness and swelling of the face and neck secondary to jugular system congestion itself secondary to rheumatic carditis and acute, congestive heart failure
- rheumatic pneumonitis causing a congestive lung condition
Unfortunately, since the 1930's, most physicians in modern western countries have dealt with fewer and fewer cases of rheumatic fever so at this time only the very most high-grade cases can be recognized and the symptoms and signs of those cases are what compose the "Jones Criteria". Even with the Jones Criteria having existed for decades, most cases of rheumatic fever suffer from mis-diagnosis, because most physicians simply do not think that rheumatic fever exists in modern, western countries including the USA. Out of mind out of sight is the rule.
Sir William Osler indicates in his text, Osler's Principles and Practices of Medicine, Twelfth Edition, cited above, presents many clinical and epidemiological factors concerning rheumatic fever. All physicians dealing with patient sicknesses should read it completely, because modern texts, written by individuals who have never, or rarely, treated rheumatic fever patinets usually mimic information in prior texts. It does indicate that rheumatic fever is often a disease that exists commonly within family members (Streptococcus pyogenese is highly contagious), he indicates that it is due to a "hypersensitiveness" to...streptococci. "There is an initial lesion with more serious manifestations occuring elsewhere in the body...The initial lesion may be in the tonsils with resulting sensitization and subsequent attacks may be due to fresh infection or to areas of chronic infection (tonsils, sinuses)...A hypersensitive state once established, a chronic infection or a repeated slight infection may serve to prolong it and an acute infection may precipitate another attack."
Further, he indicates, "As a rule, the disease sets in abruptly, but it may be preceded by irregular pains in the joints, slight malaise, sore throat, and particularly by tonsillitis...A definite rigor is uncommon; more often there is a slight chilliness. The fever rises quickly, and one or more of the joints may become painful. Within twenty-four hours from the onset the disease is fully manifest. The temperature range is from 102 deg. to 104 deg. The pulse is frequent, soft, and usually above 100. The tongue is moist and covered wiht white fur. There are...loss of appetite, thirst, constipation, and scanty, highly acid urine. In the majority of cases there are profuse, acid sweats, of a paeculiar sour odor. Sudaminal and miliary vesicles are abundant, the latter being surrounded by a minute ring of hyperemia."
In addition Dr. Osler Indicates, "The affected joints become are painful to move, soon become swollen and hot, and present a reddish flush. The order of frequency of involvement of the joints in our series was knee, ankle, shoulder, wrist, elbow, hip, hand, foot. The joints are not attacked together, but successively. The amount of swelling is variable. Extensive effusion into a joint is ratre, and much of the enlargement is due to the infiltration of the periarticular tissues with serum."
Importantly, Dr. Osler indicates, "Perhaps no disease is more painful; the inability to change posture without agonizing pain, the drenching sweats, the prostration and helplessness, combine to make it a most distressing affection...In children there may be no arthritis whatever or if present only in a mild form...The blood is profoundly altered and there is no acute febrile disease in which an anemia occurs with greater rapidity...The average leucocyte count in our cases was about 12,000 per c. mm. Epistaxis is not uncommon...With a high fever a murmur may often be heard at the apex region...Febrile albuminuria is not uncommon. Hematuria occurs occassionally."
Rheumatic fever is highly variable, enough so that a rigid set of criteria, such as the Jones Criteria, is somewhat superficial and only meaninful in very high-grade cases of rheumatic fever. Since the majority of cases of rheumatic fever are lower-grade cases, reliance on the Jones Criteria will cause physicians to simply miss, or ignore, most of the cases, probably over ninety-five percent of cases.
Dr. Osler continues with the following most important information: "Subacute rheumatic fever represents a milder form of the disease, in which all the symptoms are less pronounced. The fever rarely rises above 101 deg. F.; fewer joints are involved; and the arthritis is less intense. The cases may drag on for weeks or months. It should not be forgotten that mild or subacute forms may be associated with endocarditis or pericarditis.
The influence of age on the manifestations is marked. While the usual description applies to the disease as seen in adults, in young children there may not be any pronounced arthritis or any arthritis at all, and the discovery of endocarditis often suggests the diagnosis. Endocarditis and myocarditis are the prominant features in children in whom the picture may be very variable. The onset may be so insidious that it can hardly be termed even subacute. Ill health without any evident cause, loss of weight, anorexia, fatigue, complaint of slight pains and fever with no apparent cause should suggest the possibility. Acute arthritis is the exception in the child; cardiac involvement of some kind is the rule."
It is very difficult to record the symptoms and signs of a disease with so much variation, since they depend on the age of the sick individual, on the level of prior rheumatic sensitization, on the strain of Streptococcus pyogenes involved in the acute infection, on the pattern of infection and its secondary autoimmunological response, and on prior autoimmunological damage that has taken place during prior rheumatic, autoimmunological episodes. Then there is randomness, which is statistically enhanced in complex, systemic diseases.
One type of pathology, which is omitted from the "Jones Criteria", and from Dr. Osler's description of the signs and symptoms of rheumatic fever, but not omitted from the description provided by the information on rheumatic fever in the first edition of the Encyclopedia Britannica,cited above, is the existence of lumbago, or lumbosacral pain. Lumbosacral pain is neurological in nature and its anatomical source is deep in the gluteal area, but pain radiates centrepitally into the lumbosacral area and, of course, at times, dysesthesias radiate down the leg. Neurological pain is the worst type of pain patients with severe rheumatic fever experience, and when Dr. Osler indicates, "In attacks of great severity every one of the larger joints may be involved. Perhaps no disease is more painful..." he means that larger joints such as the shoulder and hip are involved. Within those joints patients suffer from acute brachial plexitis and neuritis of the terminal nerves of the sacral plexus with the sciatic, the posterior femoral cutaneous, and the pudendal nerves, respectively, being involved. Another name for the latter condition is, sciatica. A name provided during the late 1800's and early 1900's was sciatic rheumatism or hip gout.
Not surprisingly, lesser, more chronic levels of rheumatic autoimmunity also affect the peripheral nervous system and the many cases of lumbosacral/buttock pain and shoulder/cervical pain, which are treated as surgical conditions (herniated discs of the lumbar and cervical spine)are often caused by chronic, relatively high-levels of rheumatic autoimmune mediated neuropathy secondary to Streptococcus pyogenes infections. Often pain syndromes with the above character are "familial" in nature. One might think that the frequency of sciatic pain reflects the frequency of rheumatic autoimmunity in a community. In addition, the increased incidence of fibromyalgia, that was termed in prior eras, muscular rheuamtism, is also an indication of the increase in rheumatic autoimmunity of the American population.
It is somewhat common for individuals who have chronic pain after spinal surgery to die, compared to age-matched groups. The reason they die more frequently, even at a young age, is because such individuals have relatively high-grade, chronic rheumatism, from, perhaps, chronic Streptococcus pyogenese stimulation, and so they can develop recurrent rheumatic fever somewhat frequently or they develop rheumatic autonomic neuropathies: cardiac arrhythmias, and so they die from those maladies and not from taking opiate analgesics that most of them need to fend off the chronic neurological pain from which they suffer.
Pathophysiology
Rheumatic fever is a systemic disease affecting the peri-arteriolar connective tissue and can occur after an untreated Group A streptococcal pharyngeal infection. It is believed to be caused by antibody cross-reactivity. This cross-reactivity is a Type II hypersensitivity reaction and is termed molecular mimicry.
Usually, self reactive B cells remain anergic in the periphery without T cell co-stimulation. During a Strep. infection activated antigen presenting cells such as macrophages present the bacterial antigen to helper T cells. Helper T cells subsequently activate B cells and induce the production of antibodies against the cell wall of Streptococcus. However the antibodies may also react against the myocardium and joints[4], producing the symptoms of Rheumatic fever.
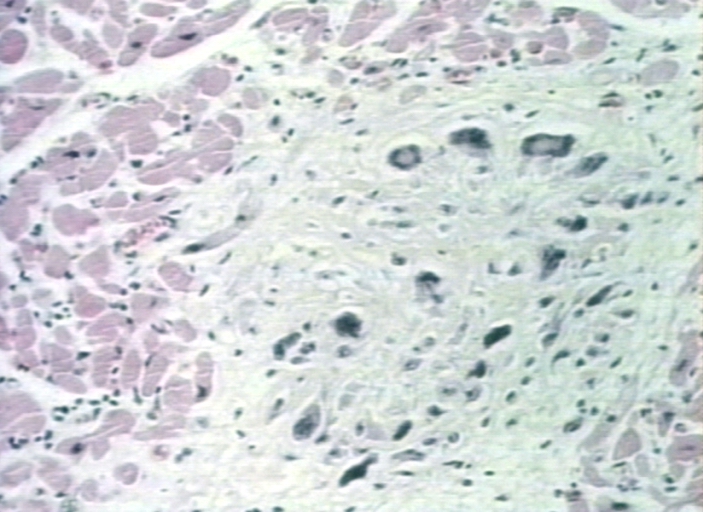
Group A streptococcus pyogenes has a cell wall composed of branched polymers which sometimes contain "M proteins" that are highly antigenic. The antibodies which the immune system generates against the "M proteins" may cross react with cardiac myofiber sarcolemma and smooth muscle cells of arteries, inducing cytokine release and tissue destruction. This inflammation occurs through direct attachment of complement and Fc receptor-mediated recruitment of neutrophils and macrophages. Characteristic Aschoff bodies, composed of swollen eosinophilic collagen surrounded by lymphocytes and macrophages can be seen on light microscopy. The larger macrophages may become Aschoff giant cells. Acute rheumatic valvular lesions may also involve a cell-mediated immunity reaction as these lesions predominantly contain T-helper cells and macrophages.[5]
In acute RF, these lesions can be found in any layer of the heart and is hence called pancarditis. The inflammation may cause a serofibrinous pericardial exudates described as “bread-and-butter” pericarditis, which usually resolves without sequelae. Involvement of the endocardium typically results in fibrinoid necrosis and verrucae formation along the lines of closure of the left-sided heart valves. Warty projections arise from the deposition, while subendothelial lesions may induce irregular thickenings called MacCallum plaques.
Chronic rheumatic heart disease is characterized by repeated inflammation with fibrinous resolution. The cardinal anatomic changes of the valve include leaflet thickening, commissural fusion and shortening and thickening of the tendinous cords. RHD cause 99% of mitral stenosis often resulting in a “fish mouth” gross appearance.[6]
Treatment
The management of acute rheumatic fever is geared toward the reduction of inflammation with anti-inflammatory medications such as aspirin or corticosteroids. Individuals with positive cultures for strep throat should also be treated with antibiotics. Another important cornerstone in treating rheumatic fever includes the continuous use of low dose antibiotics (such as penicillin, sulfadiazine, or erythromycin) to prevent recurrence.
Infection
Patients with positive cultures for streptococcus pyogenes should be treated with penicillin as long as allergy is not present. This treatment will not alter the course of the acute disease.
Inflammation
Patients with significant symptoms may require corticosteroids. Salicylates are useful for pain.
Heart failure
Some patients develop significant carditis which manifests as congestive heart failure. This requires the usual treatment for heart failure: diuretics and digoxin. Unlike normal heart failure, rheumatic heart failure responds well to corticosteroids.
Prevention
Prevention of recurrence is achieved by eradicating the acute infection and prophylaxis with antibiotics. The American Heart Association recommends daily or monthly prophylaxis continue long-term, perhaps for life.[7]
Primary care physicians, nurses also have a role in prevention, primarily in screening school-aged children for sore throats that may be caused by Group A streptococci(especially Group A β Hemolytic Streptococcus pyogenes).
Pathological Findings
-
Aortic Stenosis (Tricuspid aorta): Gross, good example of aortic stenosis due to rheumatic fever
-
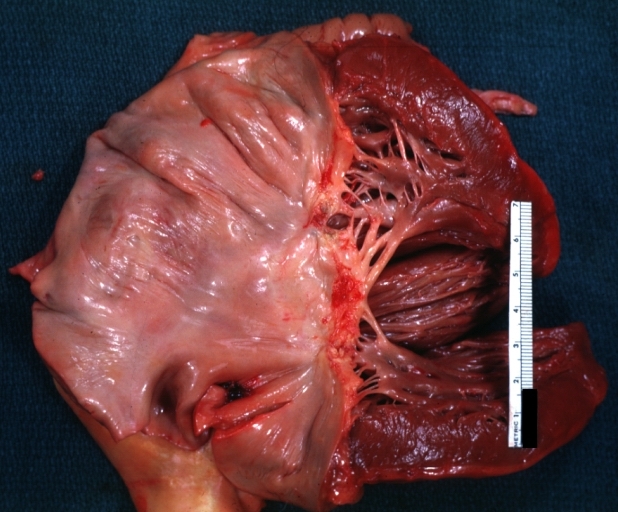
Gross, an excellent example of mitral scarring due to rheumatic fever (healing phase of an infectious lesion).
-
Rheumatic mitral valvulitis: Gross, an excellent example of fibrosis, chorda thickening and shortening has thrombus around the large left atrium
-
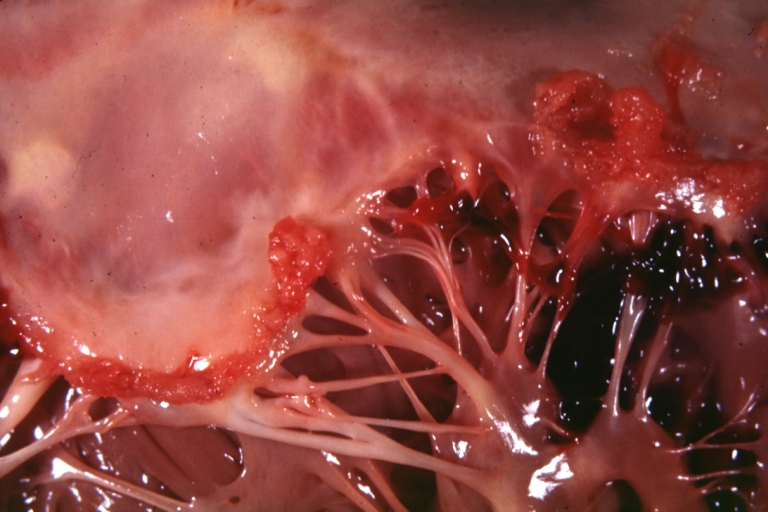
Mitral valve: acute rheumatic fever
-
Aschoff bodies in rheumatic heart disease
References
- ↑ Ferrieri P. Proceedings of the Jones criteria workshop. Circulation 2002; 106: 2521–23
- ↑ Steven J Parrillo, DO, FACOEP, FACEP. "eMedicine — Rheumatic Fever".
- ↑ "Guidelines for the diagnosis of rheumatic fever. Jones Criteria, 1992 update. Special Writing Group of the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young of the American Heart Association". JAMA. 268 (15): 2069–73. 1992. PMID 1404745.
- ↑ Abbas and Lechtman. mBasic Immunology: Functions and Disorders of the Immune System. Elsevier Inc. 2004.
- ↑ Kumar et al. Robbins and Cotran Pathologic Basis of Disease. Elsevier Inc. 2005
- ↑ "Robbins & Cotran Pathologic Basis of Disease".
- ↑ "Rheumatic Heart Disease/Rheumatic Fever". American Heart Association. Retrieved 2008-02-17.
External links
- Rheumatic fever information from Seattle Children's Hospital Heart Center
Template:Bacterial diseases Template:Hypersensitivity and autoimmune diseases zh-min-nan:Hong-sip-jia̍t de:Rheumatisches Fieber it:Febbre reumatica nl:Acuut reuma sr:Реуматска грозница