Pulmonary hypertension pathophysiology: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 83: | Line 83: | ||
[[Image:Pathophysiology_of_pulmonary_hypertension.png|500px]] | [[Image:Pathophysiology_of_pulmonary_hypertension.png|500px]] | ||
===The Role of Endothelial Injury=== | ===The Role of Endothelial Cells Injury=== | ||
All classes of pulmonary hypertension are associated with narrowing and obliteration of the pulmonary arterioles due to thickening of the [[intima]] by [[fibromuscular dysplasia]]. This constant finding has increased the interest in the role of [[endothelial]] injury and the release of [[vasoactive]] mediators in the pathogenesis of pulmonary hypertension. These mediators include both [[vasoconstrictors]] and [[vasodilators]]. Whereas the main vasoconstrictor is [[Endothelin]], Nitric Oxide (NO), [[PGI2]] and endothelium derived hyperpolarizing factor (EDHF) are vasodilators, of which NO is the most potent in reversing the effects of Endothelin.<ref> Higenbottam Tim(1994) "Pathophysiology of Pulmonary Hypertension, A role for endothelial dysfunction" Chest journal"</ref> | All classes of pulmonary hypertension are associated with narrowing and obliteration of the pulmonary arterioles due to thickening of the [[intima]] by [[fibromuscular dysplasia]]. This constant finding has increased the interest in the role of [[endothelial]] injury and the release of [[vasoactive]] mediators in the pathogenesis of pulmonary hypertension. These mediators include both [[vasoconstrictors]] and [[vasodilators]]. Whereas the main vasoconstrictor is [[Endothelin]], Nitric Oxide (NO), [[PGI2]] and endothelium derived hyperpolarizing factor (EDHF) are vasodilators, of which NO is the most potent in reversing the effects of Endothelin.<ref> Higenbottam Tim(1994) "Pathophysiology of Pulmonary Hypertension, A role for endothelial dysfunction" Chest journal"</ref> | ||
===Factors Determining the Ability of the RV to Adapt to Increased PVR=== | ===Factors Determining the Ability of the RV to Adapt to Increased PVR=== | ||
Revision as of 12:59, 14 October 2012
|
Pulmonary Hypertension Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary hypertension pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pulmonary hypertension pathophysiology |
|
Risk calculators and risk factors for Pulmonary hypertension pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor(s)-in-Chief: Ralph Matar
Overview
The pulmonary artery pressure is considered normal at a mean pressure of ≤20 mmHg at rest. Pulmonary hypertension is defined as a mean pulmonary artery pressure ≥25 mmHg at rest.[1]
The factors that are in involved in the pathophysiology of the increase in the mean pulmonary arterial pressure are: increase in pulmonary vascular resistance, increase in the right sided cardiac output and increase in the mean pulmonary venous pressure.
To note that “Pulmonary arterial hypertension” (PAH) refers to group 1 PAH in the updated WHO classification. “Pulmonary hypertension” (PH) refers to any of group 2 PH through group 5 PH. PH is also used when referring to all five groups collectively.
Pathophysiology
Increase in the Mean Pulmonary Arterial Pressure
Increase in the Pulmonary Vascular Resistance
Occlusive vasculopathy of the small pulmonary arteries and arteriole
- Idiopathic PAH
- Connective tissue disease
- HIV infection
- Congenital heart disease
Decrease in the area of the pulmonary vascular bed
Hypoxic vasoconstriction[2]
- Hypoventilation syndromes
- Parenchymal lung disease
Increase in The Right-sided Cardiac Output due to Left-to-Right Shunt
- Congenital heart diseases: atrial septal defects, ventricular septal defects, patent ductus arteriosus[3]
Increase in the Pulmonary Venous Pressure
- Mitral valve disease
- Left ventricular systolic or diastolic dysfunction
- Constrictive pericarditis
- Restrictivecardiomyopathy
- Pulmonary veno-occlusive disease
Sequence of Events in Pulmonary Hypertension
Pulmonary hypertension has several pathophysiologic mechanisms depending on the underlying etiology. Nevertheless, the following sequence of events is almost always present:
- An initiating factor leads to increased resistance in the pulmonary vasculature causing narrowing of the vessels and impaired blood flow, much as it is harder to make water flow through a narrow pipe as opposed to a wide one.
- As a consequence, the right ventricle adapts by increasing right ventricular systolic pressures to preserve the cardiac output from the right heart.
- Over time, increasing right ventricular systolic pressures will subsequently result in chronic changes in the pulmonary circulation and progressively the affected blood vessels become both stiffer and thicker, further increasing the blood pressure within the lungs and impairing blood flow.
- In addition, the increased workload of the heart causes thickening and enlargement of the right ventricle, making the heart less able to pump blood through the lungs, causing right heart failure.
- As the blood flowing through the lungs decreases, the left side of the heart receives less blood. This blood may also carry less oxygen than normal. Therefore it becomes harder and harder for the left side of the heart to pump to supply sufficient oxygen to the rest of the body, especially during physical activity.
Pulmonary Arterial Hypertension
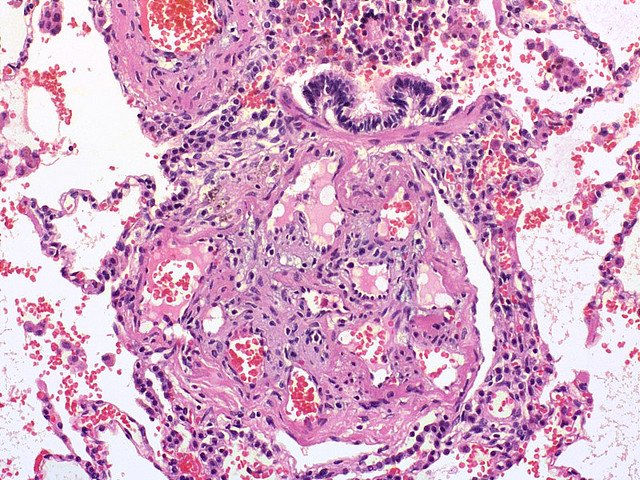
PAH is a proliferative vasculopathy of the small muscular arteries and arterioles, involving vasoconstriction, endothelial and smooth cell proliferation, fibrosis, and thrombosis. Multiple pathologic patterns are found in PAH, including:
- Intimal hyperplasia.
- Medial hypertrophy.
- Adventitial proliferation.
- In-situ thrombosis.
- Inflammation
- Plexiform arteriopathy.
Medial hypertrophy is considered an early and reversible lesion in contrast to intimal fibrosis or plexogenic arteriopathy.
In fact, the vascular proliferative nature of PAH is probably the result of sequences of injury and repair of the pulmonary vasculature in the context of a combination of noxious stimuli affecting a predisposed vasculature. Some of the well-described predisposing factors are the mutations in the BMPR2 gene[4].
The increase in pulmonary vascular resistance results from vascular changes that are the consequences of:
1- Release of cytokines and chemokines and influx of inflammatory cells and mediators
2- An imbalance between
- Locally produced vasodilators (nitric oxide and prostacyclin) [5]
- Vasoconstrictors (endothelin and thromboxane)[6]
- Apoptotic and mitogenic factors[7]
- Prothrombotic and antithrombotic factors [8]
3- Vascular wall remodeling
- Endothelial and smooth muscle cells proliferation in addition to changes in the extracellular matrix[1]
The Role of Endothelial Cells Injury
All classes of pulmonary hypertension are associated with narrowing and obliteration of the pulmonary arterioles due to thickening of the intima by fibromuscular dysplasia. This constant finding has increased the interest in the role of endothelial injury and the release of vasoactive mediators in the pathogenesis of pulmonary hypertension. These mediators include both vasoconstrictors and vasodilators. Whereas the main vasoconstrictor is Endothelin, Nitric Oxide (NO), PGI2 and endothelium derived hyperpolarizing factor (EDHF) are vasodilators, of which NO is the most potent in reversing the effects of Endothelin.[9]
Factors Determining the Ability of the RV to Adapt to Increased PVR
- Age of the patient at onset.
- Rapidity of onset of pulmonary hypertension.
- Coexisting hypoxemia.
Molecular Abnormalities
- Pulmonary arterial hypertension is characterized by endothelial dysfunction such that there is an imbalance between apoptosis and pulmonary artery smooth muscle proliferation favoring the proliferation. There is also thickened and disordered adventitia due to excessive amounts of adventitial metalloproteases.
- Mutations of two genes in the TGF-beta receptor pathway have been identified in familial pulmonary arterial hypertension:
- BMPR2: Modulates vascular cell growth. A loss of function mutation would cause unregulated smooth muscle growth.
- Activin-like kinase 1: detected in patients with hereditary hemorrhagic telangiectasia and pulmonary arterial hypertension. Mutation would cause growth-promoting alterations.
Both genes are involved SMAD-dependant signaling pathways.
References
- ↑ 1.0 1.1 International PPH Consortium. Lane KB, Machado RD, Pauciulo MW, Thomson JR, Phillips JA; et al. (2000). "Heterozygous germline mutations in BMPR2, encoding a TGF-beta receptor, cause familial primary pulmonary hypertension". Nat Genet. 26 (1): 81–4. doi:10.1038/79226. PMID 10973254.
- ↑ Sommer N, Dietrich A, Schermuly RT, Ghofrani HA, Gudermann T, Schulz R; et al. (2008). "Regulation of hypoxic pulmonary vasoconstriction: basic mechanisms". Eur Respir J. 32 (6): 1639–51. doi:10.1183/09031936.00013908. PMID 19043010.
- ↑ Schulze-Neick I, Kaemmerer H (2009). "[Pulmonary hypertension and pulmonary circulation in congenital heart disease]". Dtsch Med Wochenschr. 134 Suppl 5: S170–2. doi:10.1055/s-0029-1225317. PMID 19718608.
- ↑ Yuan JX, Rubin LJ (2005). "Pathogenesis of pulmonary arterial hypertension: the need for multiple hits". Circulation. 111 (5): 534–8. doi:10.1161/01.CIR.0000156326.48823.55. PMID 15699271.
- ↑ Giaid A, Saleh D (1995). "Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension". N Engl J Med. 333 (4): 214–21. doi:10.1056/NEJM199507273330403. PMID 7540722.
- ↑ Christman BW, McPherson CD, Newman JH, King GA, Bernard GR, Groves BM; et al. (1992). "An imbalance between the excretion of thromboxane and prostacyclin metabolites in pulmonary hypertension". N Engl J Med. 327 (2): 70–5. doi:10.1056/NEJM199207093270202. PMID 1603138.
- ↑ Harrison W. Pulmonary Arterial Hypertension, N Engl J Med 2004;351:1655-65
- ↑ Harrison W. Pulmonary Arterial Hypertension, N Engl J Med 2004;351:1655-65
- ↑ Higenbottam Tim(1994) "Pathophysiology of Pulmonary Hypertension, A role for endothelial dysfunction" Chest journal"