Pneumonia differential diagnosis: Difference between revisions
Ahmed Younes (talk | contribs) |
|||
| Line 355: | Line 355: | ||
+++, occurs frequently | +++, occurs frequently | ||
Pnemonia must be differentiated from other diseases that cause [[atypical pneumonia]] such as Q fever and legionella pneumonia: | |||
{| class="wikitable" | |||
!Disease | |||
!Prominent clinical features | |||
!Lab findings | |||
!Chest X-ray | |||
|- | |||
|Q fever | |||
| | |||
* Q fever is characterized by abrupt onset of [[fever]], [[myalgia]], [[headache]], and other constitutional symptoms. | |||
* [[Cough]] is the most prominent respiratory symptom and it is usually dry.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* [[Cough]] is associated with [[dyspnea]] and [[pleuritic chest pain]]. | |||
| | |||
* [[Antibody]] detection using [[Immunofluorescence|indirect immunofluorescence]] (IIF) is the preferred method for diagnosis. | |||
* [[Polymerase chain reaction|PCR]] can be used if IIF is negative, or very early once disease is suspected. | |||
* [[Coxiella burnetii|''C. burnetii'']] does not grow on ordinary blood cultures, but can be cultivated on special media such as embryonated eggs or cell culture. | |||
* A two-to-three fold increase in [[Aspartate transaminase|AST]] and [[ALT]] is seen in most patients. | |||
| | |||
[[Image:Q fever.gif|center|300px|thumb|Q fever pneumonia - - Case courtesy of Royal Melbourne Hospital Respiratory, Radiopaedia.org, rID 21993 ]] | |||
|- | |||
|[[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] | |||
| | |||
* [[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] can be [[asymptomatic]]. | |||
* [[Headache]], [[Nausea and vomiting|nausea]], and [[malaise]] usually precede the onset of symptoms.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* [[Cough]] is intractable and nonproductive. | |||
| | |||
* Postitve [[Coombs test]] | |||
* [[Leukocytosis]] | |||
* [[Thrombocytosis]] | |||
| | |||
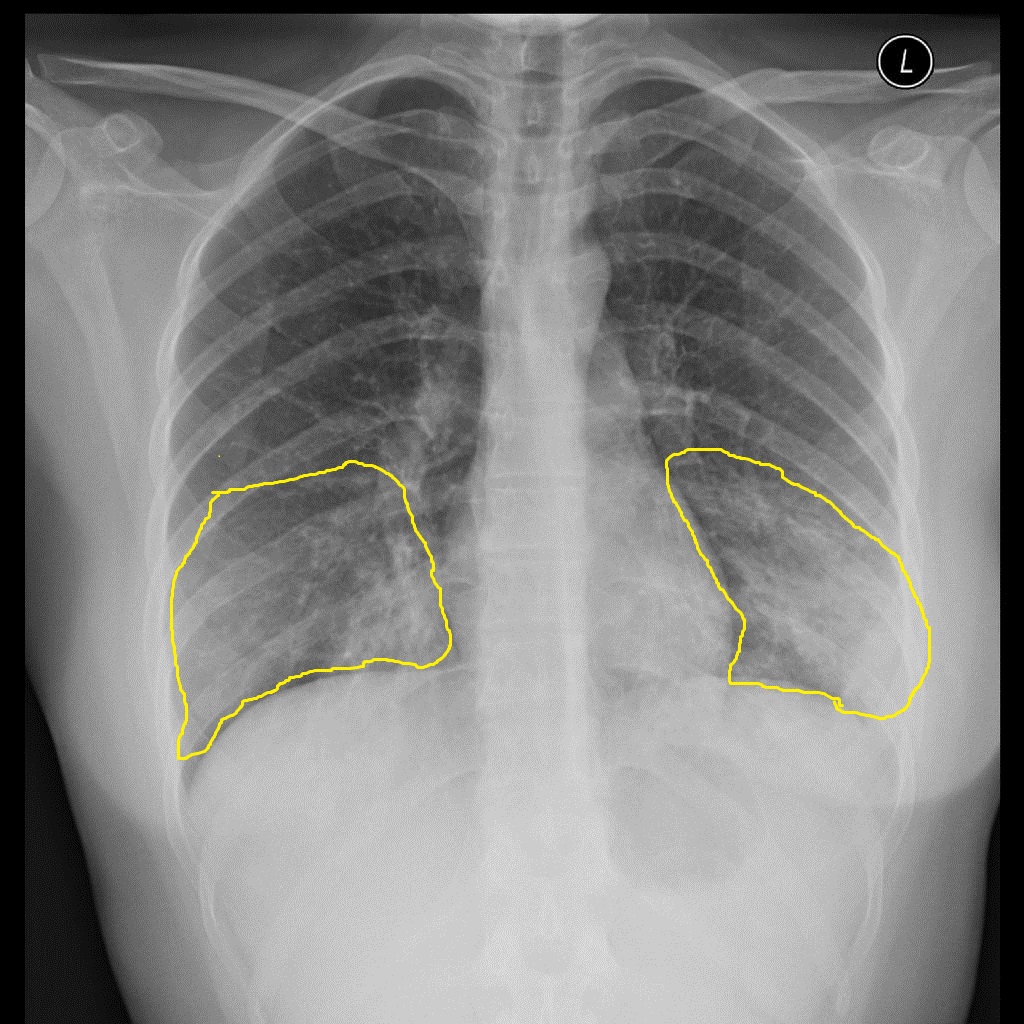
[[Image:Atypical-pneumonia-mycoplasma - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781.jpg|center|300px|thumb|Mycoplasma pneumonia - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781]] | |||
|- | |||
|[[Legionellosis]] | |||
| | |||
* [[Legionellosis]] is characterized by cough that is slightly productive.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* Constitutional symptoms such as [[chills]], [[myalgia]], and [[arthralgia]]. | |||
* Gastrointestinal symptoms such as [[diarrhea]], [[nausea]], and [[vomiting]]. | |||
| | |||
* Labs are nonspecific for diagnosing [[legionellosis]] | |||
* [[Renal dysfunction|Renal]] and [[hepatic dysfunction]] | |||
* [[Thrombocytopenia]] and [[leukocytosis]] | |||
* [[Hyponatremia]] | |||
| | |||
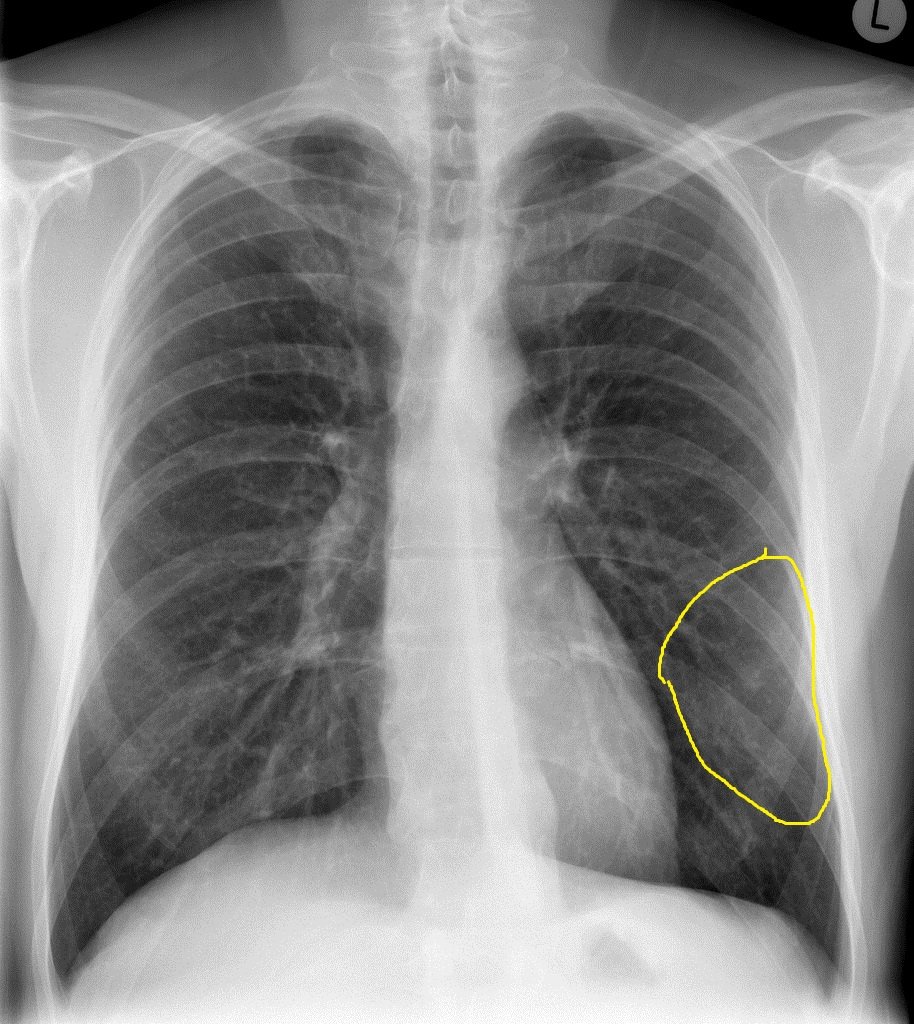
[[Image:Legionella-pneumonia - Case courtesy of Dr Henry Knipe, Radiopaedia.org, rID 31816.jpg|center|300px|thumb|Legionella pneumonia - Case courtesy of Dr Henry Knipe, Radiopaedia.org, rID 31816 ]] | |||
|- | |||
|[[Chlamydia pneumonia]] | |||
| | |||
* There are no specific clinical features of [[chlamydia pneumonia]]. | |||
* Symptoms appear gradually. | |||
* [[Chlamydia infection]] is usually associated with [[upper respiratory tract]] symptoms ([[pharyngitis]], [[sinusitis]], etc). | |||
* It might be associated with extrapulmonary maifestations such as [[meningitis]] and [[Guillain-Barre syndrome]].<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
| | |||
* [[Chlamydia pneumonia]] is usually associated with normal [[WBC|WBC count.]] | |||
* Diagnosed with the presence of [[Antibody|antichlamydial antibody]] (through [[complement fixation]] or direct immunofluoroscence) or direct antigen detection. | |||
| | |||
[[Image:Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567.jpg|center|300px|thumb|Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567]] | |||
|} | |||
==References== | ==References== | ||
Revision as of 15:46, 29 August 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.D. [2]
|
Pneumonia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumonia differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Pneumonia differential diagnosis |
|
Risk calculators and risk factors for Pneumonia differential diagnosis |
Overview
Pneumonia should be differentiated from other conditions that cause cough, fever, shortness of breath and tachypnea, such as asthma, COPD, CHF, cancer, GERD, pulmonary emboli.
Differentiating Pneumonia from other Diseases
| Disease | Findings |
|---|---|
| Acute bronchitis | No infiltrates seen on the chest X-ray. |
| Asthma | Past medical history, no infiltrates seen on chest X-ray. |
| Bronchiolitis obliterans | Should be suspected in patients with pneumonia who do not respond to antibiotics treatment. |
| Congestive heart failure | Bilateral pulmonary edema, shortness of breath. |
| COPD | Past medical history, no infiltrates on chest X-ray, fever is uncommon. |
| Empyema | CXR showing features of pleural effusion, inflammatory markers on thoracocentesis. |
| Endocarditis | Finding of septic pulmonary emboli |
| Gastroesophageal reflux disease (GERD) | Normal chest X-ray, symptoms are worse during night and associated with meals. |
| Lung abscess | Chest X-ray shows signs of lung abscess. |
| Lung cancer | Weight loss, clear sputum. CT scan and biopsy are helpful in ruling out malignancy. |
| Pertussis | Productive cough for weeks, nasopharyngeal aspirate aids in diagnosis. |
| Pulmonary embolus | A high degree of suspicion should be kept for pulmonary embolus. Chest X-ray may be normal. |
| Sinusitis | Sinus tenderness, post nasal drip. |
| Vasculitis | Systemic manifestations of collagen vascular disease may be seen. |
Differential diagnosis
| Causes of
lung cavities |
Differentiating Features | Differentiating radiological findings | Diagnosis
confirmation |
|---|---|---|---|
|
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
|
| |
|
|
| |
|
|
||
|
|
| |
|
|
|
Table 1; Differentiating psittacosis from other diseases
| Clinical feature | Cough | Sputum | Dyspnea | Sore throat | Headache | Confusion | Diarrhea | Chest radiograph changes | Hyponatremia | Leukopenia | Abnormal Liver function tests | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psittacosis | ++ | - | + | - | +++ | + | Minimal |
|
- | + | - | Doxycycline |
| C.pneumoniae pneumonia | + | + | + | +++ | ++ | + | - |
|
- | - | - | Doxycycline, Azithromycin |
| M. pneumoniae pneumonia | ++ | ++ | ++ | - | - | - | - |
|
- | - | + | Doxycycline |
| L. Pneumophila infection | + | +++ | +++ | - | + | ++ | + | Often Multifocal | ++ | + | ++ | Doxycycline |
| Influenza | ++ | ++ | ++ | ++ | ++ | +/- | +/- |
|
- | - | - | zanamivir, oseltamivir, |
| Endocarditis | ++ | ++ | + | - | - | - | - |
bases bilaterally |
- | +/- | +/- | Vancomycin |
| Coxiella burnetii infection | ++ | - | + | +/- | - | +/- | Minimal |
|
- | +/- | =/- | Doxycycline |
| Leptospirosis | ++ | + | ++ | + | + | ++ | - |
|
+++ | Doxycycline, azithromycin, amoxicillin | ||
| Brucellosis | ++ | - | + | - | ++ | + | - |
|
-/+ | +/- | +/- | Doxycycline, rifampin |
Key;
+, occurs in some cases
++, occurs in many cases,
+++, occurs frequently
Pnemonia must be differentiated from other diseases that cause atypical pneumonia such as Q fever and legionella pneumonia:
| Disease | Prominent clinical features | Lab findings | Chest X-ray |
|---|---|---|---|
| Q fever |
|
 | |
| Mycoplasma pneumonia |
|
|
 |
| Legionellosis |
|
|
 |
| Chlamydia pneumonia |
|
|
 |
References
- ↑ Schiele F, Muller J, Colinet E, Siest G, Arzoglou P, Brettschneider H; et al. (1992). "Interlaboratory study of the IFCC method for alanine aminotransferase performed with use of a partly purified reference material". Clin Chem. 38 (12): 2365–71. PMID 1458569.
- ↑ Castro-Guardiola A, Armengou-Arxé A, Viejo-Rodríguez A, Peñarroja-Matutano G, Garcia-Bragado F (2000). "Differential diagnosis between community-acquired pneumonia and non-pneumonia diseases of the chest in the emergency ward". Eur J Intern Med. 11 (6): 334–339. PMID 11113658.
- ↑ Ahnsjö, Sven (1935). "Contribution to the Differential Diagnosis of Pneumonia in Childhood". Acta Paediatrica. 17 (3): 439–446. doi:10.1111/j.1651-2227.1935.tb07697.x. ISSN 0803-5253.
- ↑ 4.0 4.1 Chaudhuri MR (1973). "Primary pulmonary cavitating carcinomas". Thorax. 28 (3): 354–66. PMC 470041. PMID 4353362.
- ↑ Mouroux J, Padovani B, Elkaïm D, Richelme H (1996). "Should cavitated bronchopulmonary cancers be considered a separate entity?". Ann. Thorac. Surg. 61 (2): 530–2. doi:10.1016/0003-4975(95)00973-6. PMID 8572761.
- ↑ Onn A, Choe DH, Herbst RS, Correa AM, Munden RF, Truong MT, Vaporciyan AA, Isobe T, Gilcrease MZ, Marom EM (2005). "Tumor cavitation in stage I non-small cell lung cancer: epidermal growth factor receptor expression and prediction of poor outcome". Radiology. 237 (1): 342–7. doi:10.1148/radiol.2371041650. PMID 16183941.
- ↑ 7.0 7.1 Langford CA, Hoffman GS (1999). "Rare diseases.3: Wegener's granulomatosis". Thorax. 54 (7): 629–37. PMC 1745525. PMID 10377211.
- ↑ Lee KS, Kim TS, Fujimoto K, Moriya H, Watanabe H, Tateishi U, Ashizawa K, Johkoh T, Kim EA, Kwon OJ (2003). "Thoracic manifestation of Wegener's granulomatosis: CT findings in 30 patients". Eur Radiol. 13 (1): 43–51. doi:10.1007/s00330-002-1422-2. PMID 12541109.
- ↑ Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA, DePalo L, Hunninghake G, Iannuzzi MC, Johns CJ, McLennan G, Moller DR, Newman LS, Rabin DL, Rose C, Rybicki B, Weinberger SE, Terrin ML, Knatterud GL, Cherniak R (2001). "Clinical characteristics of patients in a case control study of sarcoidosis". Am. J. Respir. Crit. Care Med. 164 (10 Pt 1): 1885–9. doi:10.1164/ajrccm.164.10.2104046. PMID 11734441.
- ↑ Brauner MW, Grenier P, Mompoint D, Lenoir S, de Crémoux H (1989). "Pulmonary sarcoidosis: evaluation with high-resolution CT". Radiology. 172 (2): 467–71. doi:10.1148/radiology.172.2.2748828. PMID 2748828.
- ↑ Murphy J, Schnyder P, Herold C, Flower C (1998). "Bronchiolitis obliterans organising pneumonia simulating bronchial carcinoma". Eur Radiol. 8 (7): 1165–9. doi:10.1007/s003300050527. PMID 9724431.
- ↑ 12.0 12.1 Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan AN (2008). "Bronchiolitis obliterans organizing pneumonia: pathogenesis, clinical features, imaging and therapy review". Ann Thorac Med. 3 (2): 67–75. doi:10.4103/1817-1737.39641. PMC 2700454. PMID 19561910.
- ↑ Cordier JF, Loire R, Brune J (1989). "Idiopathic bronchiolitis obliterans organizing pneumonia. Definition of characteristic clinical profiles in a series of 16 patients". Chest. 96 (5): 999–1004. PMID 2805873.
- ↑ Lee KS, Kullnig P, Hartman TE, Müller NL (1994). "Cryptogenic organizing pneumonia: CT findings in 43 patients". AJR Am J Roentgenol. 162 (3): 543–6. doi:10.2214/ajr.162.3.8109493. PMID 8109493.
- ↑ Suri HS, Yi ES, Nowakowski GS, Vassallo R (2012). "Pulmonary langerhans cell histiocytosis". Orphanet J Rare Dis. 7: 16. doi:10.1186/1750-1172-7-16. PMC 3342091. PMID 22429393.
- ↑ Moore AD, Godwin JD, Müller NL, Naidich DP, Hammar SP, Buschman DL, Takasugi JE, de Carvalho CR (1989). "Pulmonary histiocytosis X: comparison of radiographic and CT findings". Radiology. 172 (1): 249–54. doi:10.1148/radiology.172.1.2787035. PMID 2787035.
- ↑ 17.0 17.1 17.2 17.3 Irfan M, Farooqi J, Hasan R (2013). "Community-acquired pneumonia". Curr Opin Pulm Med. 19 (3): 198–208. doi:10.1097/MCP.0b013e32835f1d12. PMID 23422417.