Papilledema: Difference between revisions
No edit summary |
|||
| Line 20: | Line 20: | ||
== Overview == | == Overview == | ||
Papilledema is defined as swelling of the [[optic disc]] that is caused by increased [[intracranial pressure]]. The swelling is usually bilateral and can occur over a period of hours to weeks. | Papilledema is defined as swelling of the [[optic disc]] that is caused by increased [[intracranial pressure]]. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare. Papilledema is mostly seen as a symptom resulting from another pathophysiological process. | ||
In intracranial hypertension, papilledema most commonly occurs bilaterally. When papilledema is found on fundoscopy, further evaluation is warranted as vision loss can result if the underlying condition is not treated. Further evaluation with a CT or MRI of the brain and/or spine is usually performed. Unilateral papilledema can suggest orbital pathology, such as an optic nerve glioma. | |||
==Pathophysiology== | ==Pathophysiology== | ||
Revision as of 15:46, 16 July 2012
|
Papilledema |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Papilledema On the Web |
|
American Roentgen Ray Society Images of Papilledema |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Kalsang Dolma, MBBS
Synonyms and Keywords: papilloedema
Overview
Papilledema is defined as swelling of the optic disc that is caused by increased intracranial pressure. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare. Papilledema is mostly seen as a symptom resulting from another pathophysiological process.
In intracranial hypertension, papilledema most commonly occurs bilaterally. When papilledema is found on fundoscopy, further evaluation is warranted as vision loss can result if the underlying condition is not treated. Further evaluation with a CT or MRI of the brain and/or spine is usually performed. Unilateral papilledema can suggest orbital pathology, such as an optic nerve glioma.
Pathophysiology
As the optic nerve sheath is continuous with the subarachnoid space of the brain (and is regarded as an extension of the central nervous system), increased pressure is transmitted through to the optic nerve. The brain itself is relatively spared from pathological consequences of high pressure.
However, the anterior end of the optic nerve stops abruptly at the eye. Hence the pressure is asymmetrical and this causes a pinching and protrusion of the optic nerve at its head.
The fibers of the retinal ganglion cells of the optic disc become engorged and bulge anteriorly. Persistent and extensive optic nerve head swelling, or optic disc edema, can lead to loss of these fibers and permanent visual impairment.
Causes
Common Causes
Cerebral venous sinus thrombosis
Idiopathic intracranial hypertension
Causes by Organ System
Causes in Alphabetical Order
Differentiation of Papilledema from other Disorders
Papilledema should be distinguished from pseudopapilledema which is caused by
- Optic disc drusen
- Tilted optic disc
Epidemiology and Demographics
Papilledema occurs in approximately 50% of those with a brain tumour.
Diagnosis
Checking the eyes for signs of papilledema should be carried out whenever there is a clinical suspicion of raised intracranial pressure. Because of the (rare) possibility of a brain tumor, pseudotumor cerebri or cerebral venous sinus thrombosis, all of which can increase intracranial pressure, this examination has become common for patients suffering from headaches.
Physical Examination
Eyes
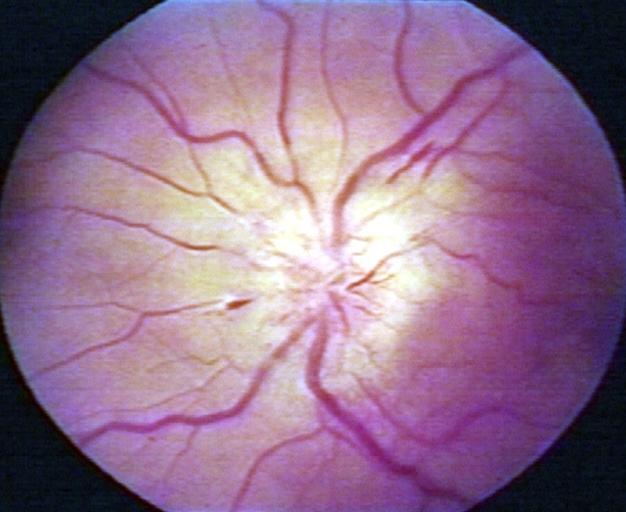
-
Papilledema.
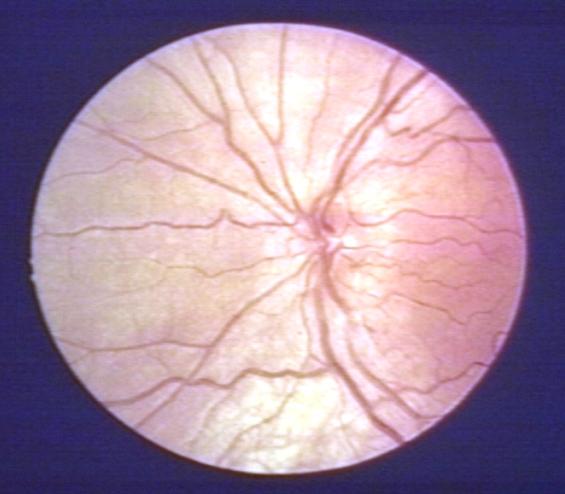
-
Pseudopapilledema.
There are 10 hallmarks of papilledema:
- Blurring of the disc margins
- Filling in of the optic disc cup
- Anterior bulging of the nerve head
- Edema of the nerve fiber layer
- Retinal or choroidal folds
- Congestion of retinal veins
- Peripapillary hemorrhages
- Hyperemia of the optic nerve head
- Nerve fiber layer infarcts
- Hard exudates of the optic disc