Meningioma pathophysiology
|
Meningioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Meningioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Meningioma pathophysiology |
|
Risk calculators and risk factors for Meningioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
Meningioma arises from the arachnoid "cap" cells, which are normally involved in the protection of the central nervous system by forming a thick envelope of meninges around the brain and spinal cord.[1][2][3] The majority of meningiomas are benign. Development of meningioma is the result of multiple genetic mutations The majority of meningioma cases involve a deletion of the neurofibromatosis 2 gene located on chromosome 22. On gross pathology, a gray, well-circumscribed, dome-shaped mass is a characteristic finding of meningioma. On microscopic histopathological analysis, whorled appearance, calcification, and psammoma bodies are characteristic findings of meningioma.[4]
Pathogenesis
- Meningiomas are the most common benign tumors of the brain. They are also the most common nonglial brain tumors.[5]
- Meningioma arises from the arachnoid "cap" cells, which are normally involved in the protection of the central nervous system by forming a thick envelope of meninges around the brain and spinal cord.[6]
- Meningiomas are commonly found in the base of the skull and perivenous sinuses due to the abundance of arachnoid cap cells in these sites. They are usually non-infilterative.[5]
- The majority of meningiomas are benign (90%), about 6% are atypical, and 2% are malignant.[5]
- Some meningiomas may be positive for progesterone receptors on histological examination. This can lead to increased tumor size and symptom burden during pregnancy and the luteal phase of the menstural cycle.[5]
- Meningiomas may possess receptors for platelet derived growth factor, vascular endothelial growth factor (VEGF), glucocorticoid, and epidermal growth factor.[5]
- Meningiomas can be found anywhere in the central nervous system, with its most frequent distribution as follows: parasagittal (20.8%), then convexity (15.2%), and tuberculum sellae (12.8%).[7]
- A meningioma can be localized in the following areas: sphenoid ridge, olfactory groove, falx, lateral ventriculi, tentorium, the middle fossa, the orbit, the spinal channel, the Sylvian fissure, extracalvarial, multiple localization, the pontocerebral angle, the sphenoidal plane, and the foramen magnum.[7]
- The characteristics of a meningioma can be determined based on histopathological variables like tumor gradient, histological subtype, proliferative index, and invasiveness of a tumor to the brain.[7]
- Meningiomas demonstrate estrogen and progesterone sensitivity and may grow during pregnancy.[3]
- About 90% of meningiomas are benign, 6% are atypical, and 2% are malignant.[5]
Genetics
- Development of meningioma is the result of multiple genetic mutations.[1]
- The majority of meningioma cases involve a deletion of the neurofibromatosis 2 gene located on chromosome 22.
- Other genes involved in the pathogenesis of meningioma include:
- Protein kinase AKT1 gene located on chromosome 14
- Meningioma 1 MN1 gene located on chromosome 22
- Phosphatase and tensin homolog PTEN gene located on chromosome 10
- SMO gene located on chromosome 6
Gross Pathology
- On gross pathology, a gray, well-circumscribed, dome-shaped mass is a characteristic finding of meningioma.[1]

Microscopic Pathology
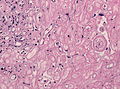
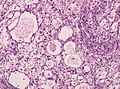
- On microscopic histopathological analysis, whorled appearance, calcification, and psammoma bodies are characteristic findings of meningioma.[4]
- The table below differentiates between the three main groups of meningioma according to WHO histological classification:[2][3][4]
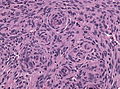
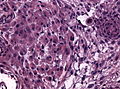
| Grade | Histologic features | Image |
|---|---|---|
|
Benign (Grade I) meningioma |
 | |
|
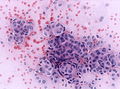
Atypical (Grade II) meningioma |
Brain invasion, 4 or more mitosis/10 HPF, necrosis, increased cell count, high nucleus:cytoplasm ratio, increased nucleoli size, presence of sheeting |
 |
|
Anaplastic (Grade III) meningioma |
20 or more mitoses/10 HPF, histology may be similar to carcinoma or sarcoma |
 |
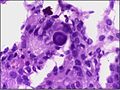
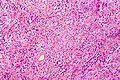
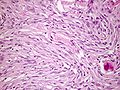
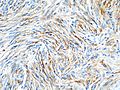
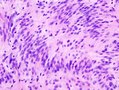
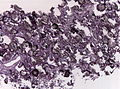
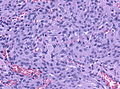
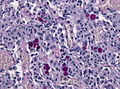
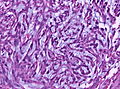
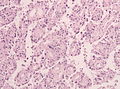
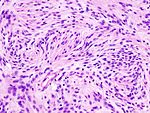
- Shown below is a series of microscopic images of different subtypes of meningioma:[4]
-
Meningothelial meningioma with syncytial appearance and whorl formation
-
Meningothelial meningioma with psammoma body
-
Meningothelial meningioma with onion bulb formation
-
Meningothelial meningioma on HPS stain
-
Fibrous meningioma with spindle cells in parallel bundles
-
Fibrous meingioma on EMA stain
-
Transitional meningioma with coexisting lobular and fasicular growth patterns
-
Psammomatous meningioma with numerous psammoma bodies
-
Angiomatous meningioma with hyalinized vessels
-
Microcystic meningioma with cystic appearance and increased pleomorphism of the elongated cells
-
Secretory meningioma with secretory granules
-
Secretory meningioma with PAS stain positive secretory granules
-
Chordoid meningioma with myxoid appearance
-
Rhabdoid meningioma with abundant cytoplasm and cross-striations
References
- ↑ 1.0 1.1 1.2 Meningioma. Wikipedia(2015) https://en.wikipedia.org/wiki/Meningioma#cite_note-pmid7731706-9 Accessed on September, 25 2015
- ↑ 2.0 2.1 Meningioma. Canadian Cancer Society http://www.cancer.ca/en/cancer-information/cancer-type/brain-spinal/brain-and-spinal-tumours/meningioma/?region=mb September, 25 2015
- ↑ 3.0 3.1 3.2 Meningeoma. Radiopaedia(2015)http://radiopaedia.org/articles/meningioma Accessed on September, 25 2015
- ↑ 4.0 4.1 4.2 4.3 Meningioma. Libre Pathology(2015) http://librepathology.org/wiki/index.php/Meningioma#Quick_overview accessed on September, 25 2015
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Gurcay AG, Bozkurt I, Senturk S, Kazanci A, Gurcan O, Turkoglu OF; et al. (2018). "Diagnosis, Treatment, and Management Strategy of Meningioma during Pregnancy". Asian J Neurosurg. 13 (1): 86–89. doi:10.4103/1793-5482.181115. PMC 5820904. PMID 29492130.
- ↑ Wiemels J, Wrensch M, Claus EB (2010) Epidemiology and etiology of meningioma. J Neurooncol 99 (3):307-14. DOI:10.1007/s11060-010-0386-3 PMID: 20821343
- ↑ 7.0 7.1 7.2 Sumkovski R, Micunovic M, Kocevski I, Ilievski B, Petrov I (2019). "Surgical Treatment of Meningiomas - Outcome Associated With Type of Resection, Recurrence, Karnofsky Performance Score, Mitotic Count". Open Access Maced J Med Sci. 7 (1): 56–64. doi:10.3889/oamjms.2018.503. PMC 6352459. PMID 30740161.
- ↑ Image courtesy of Dr Dharam Ramnani Radiopaedia(original file "here"). Creative Commons BY-SA-NC