Meningioma pathophysiology
|
Meningioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Meningioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Meningioma pathophysiology |
|
Risk calculators and risk factors for Meningioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
Pathogenesis
Meningioma arise from arachnoidal cells, most of which are near the vicinity of the venous sinuses, and this is the site of greatest prevalence for meningioma formation. They are most frequently attached to the dura over the superior parasagittal surface of frontal and parietal lobes, along the sphenoid ridge, in the olfactory grooves, the sylvian region, superior cerebellum along the falx cerebri, cerebellopontine angle, and the spinal cord. The tumor is usually gray, well-circumscribed, and takes on the form of space it occupies. They are usually dome-shaped, with the base lying on the dura.
Meningiomas are the most common benign tumors of the brain (95% of benign tumors), rare meningioma can be malignant. It arises from the meninges which surround the brain and spinal cord. A small meningioma causes no significant signs. With the development of the lump, frequent symptoms include changes in vision, for example seeing double or blurriness, headache, hearing loss memory loss, etc. A meningioma doesn't always require immediate treatment. Treatments include surgery, radiation and a combination of them.
Histologically, the cells are relatively uniform, with a tendency to encircle one another, forming whorls and psammoma bodies (laminated calcific concretions). They have a tendency to calcify and are highly vascularized.
Genetics
- Development of meningioma is the result of multiple genetic mutations.
- The most common gene involved in the pathogenesis of meningioma is the neurofibromatosis 2 gene located on chromosome 22.
- Other genes involved in the pathogenesis of meningioma include:
- Protein kinase (AKT1) gene located on human chromosome 14
- MN1 gene located on human chromosome 22
- Phosphatase and tensin homolog (PTEN) gene located on both human chromosomes 10 and 19
- SMO gene located on human chromosome 6 and 7
Gross Pathology
On gross pathology, a gray, well-circumscribed, dome-shaped mass is a characteristic finding of meningioma.[1]
Microscopic Pathology
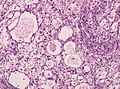
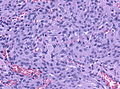
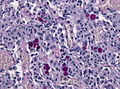
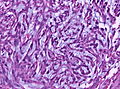
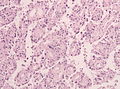
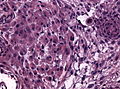
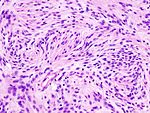
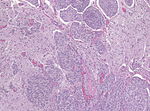
- On microscopic histopathological analysis, whorled appearance, calcification, and psammoma bodies are characteristic findings of of meningioma.[2]
- The table below differentiates between the three main groups of meningioma according to WHO histological classification:[2]
| Grade | Histologic features | Image |
|---|---|---|
|
Benign (Grade I) meningioma |
 | |
|
Atypical (Grade II) meningioma |
Brain invasion, 4 or more mitosis/10 HPF, necrosis, increased cell count, high nucleus:cytoplasm ratio, increased nucleoli size, presence of sheeting |
 |
|
Anaplastic (Grade III) meningioma |
20 or more mitoses/10 HPF, histology similar to carcinoma or sarcoma |
 |
- Shown below is a series of microscopic images featuring specific findings seen in each subtype of meningioma:[2]
-
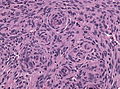
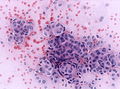
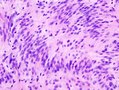
A smear showing meningothelial meningioma with syncytial appearance and whorl formation
-
A smear showing meningothelial meningioma with onion bulb formation
-
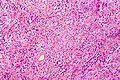
A smear showing meningothelial meningioma HPS stain
-
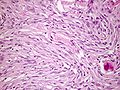
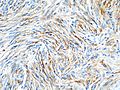
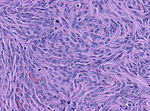
A smear showing fibrous meningioma with spindle cells in parallel bundles
-
A smear showing fibrous meingioma on EMA stain
-
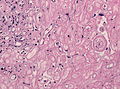
A smear showing transitional meningioma with coexisting lobular and fasicular growth patterns
-
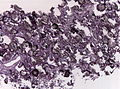
A smear showing psammomatous meningioma with numerous psammoma bodies
-
A smear showing angiomatous meningioma with hyalinized vessels
-
A smear showing microcystic meningioma with cystic appearance and increased pleomorphism of the elongated cells
-
A smear showing secretory meningioma with secretory granules
-
A smear showing secretory meningioma with PAS stain positive secretory granules
-
A smear showing chordoid meningioma with myxoid appearance
-
A smear showing rhabdoid meningiomao with abundant cytoplasm and cross-striations
References
- ↑ Meningeoma. Wikipedia(2015) https://en.wikipedia.org/wiki/Meningioma#History_and_nomenclature Accessed on September, 25th 2015
- ↑ 2.0 2.1 2.2 Meningioma. Liberpathology(2015) http://librepathology.org/wiki/index.php/Meningioma#Quick_overview accessed on September, 25th 2015