Ménière's disease: Difference between revisions
No edit summary |
No edit summary |
||
| (23 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = Ménière's disease | | Name = Ménière's disease | | ||
| Line 9: | Line 10: | ||
OMIM = 156000 | | OMIM = 156000 | | ||
MedlinePlus = 000702 | | MedlinePlus = 000702 | | ||
eMedicineSubj = | eMedicineSubj = | | ||
eMedicineTopic = | eMedicineTopic = | | ||
MeshID = | | MeshID = | | ||
}} | }} | ||
| Line 17: | Line 18: | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
{{CMG}} | {{CMG}} {{AE}}{{SUF}} | ||
{{ | |||
==Overview== | ==Overview == | ||
'''Ménière's disease''' is a disorder | '''Ménière's disease''' is a disorder affecting the sensory organ within the [[inner ear]] responsible for balance and hearing. It is characterized by episodes of [[dizziness]], [[tinnitus]] and progressive hearing loss, usually in one ear. This disturbance in the normal physiological functioning of the inner ear can be attributed to an increase in volume and pressure in the [[endolymph]] of the inner ear. The term "Ménière's" takes it origin after the French physician [[Prosper Ménière]], who first reported that [[Vertigo (medical)|vertigo]] was caused by disorders of the inner ear in an article published in 1861. | ||
==Historical Background== | ==Historical Background== | ||
Ménière's disease had been recognized prior to 1972 | Ménière's disease had been recognized prior to 1972 but the information available on its prevalence and understanding remained rather vague. Committees at the Academy of Ophthalmology and Otolaryngology made set criteria for diagnosing Ménière's, as well as defining two sub categories of Ménière's: cochlear (without vertigo) and vestibular (without deafness). | ||
In 1972, the academy defined | In 1972, the academy defined criteria for diagnosing Ménière's disease as: | ||
#Fluctuating, progressive, sensorineural deafness. | #Fluctuating, progressive, sensorineural deafness. | ||
#Episodic, characteristic definitive spells of vertigo lasting 20 minutes to 24 hours with | #Episodic, characteristic definitive spells of vertigo lasting 20 minutes to 24 hours without loss of consciousness and associated with the presence of vestibular nystagmus . | ||
#Usually tinnitus. | #Usually tinnitus. | ||
#Attacks are characterized by periods of remission and exacerbation. | #Attacks are characterized by periods of remission and exacerbation. | ||
In 1985, this list changed to alter wording, such as | In 1985, this list changed to alter wording, such as "deafness" changed to "hearing loss associated with tinnitus, characteristic of low frequencies" and requiring more than one attack of vertigo to diagnose. Finally in 1995, the list was again altered to allow for its documentation based on various degrees of probability of having the disease: | ||
# Certain - Definite disease with [[Histopathology|histopathological]] confirmation | # Certain - Definite disease with [[Histopathology|histopathological]] confirmation | ||
# Definite - Requires two or more definitive episodes of vertigo with hearing loss plus tinnitus and/or aural fullness | # Definite - Requires two or more definitive episodes of vertigo with hearing loss plus tinnitus and/or aural fullness | ||
# Probable - Only one definitive episode of vertigo and the other symptoms and signs | # Probable - Only one definitive episode of vertigo and the other symptoms and signs | ||
# Possible - Definitive vertigo with no associated hearing loss | # Possible - Definitive vertigo with no associated hearing loss | ||
==Cause== | ==Cause== | ||
It has also been proposed that Ménière's symptoms | * Physiological -The exact cause of Ménière's disease is not known, but it is believed to be related to ''endolymphatic hydrops'' or excessive fluid in the inner ear. Several theories describing the causative mechanism have been proposed and documented, One such theory includes the decreased absorption or the increased production of the endolymph within the endolymphatic sac. This in-turn contributes to the swelling of the [[endolymphatic sac]] or other tissues in the [[vestibular system]] of the inner ear, a system responsible for the body's sense of balance which is disrupted a s a result of this pathology. | ||
* Anatomical - Longitudinal blockage in the structures responsible for the drainage of the endolymph causing an increase in the hydrostatic pressure within the endolymphatic sac was another theory that was proposed to describe the possible structural cause behind the disease. | |||
* Head trauma | |||
* Infectious - It has also been proposed that Ménière's symptoms could be the result of damage caused by a the large family of DNA virus, [[herpesviridae]]. [[Herpesviridae]] is prevalent in the dormant state in a majority of the population. It is suggested that the virus is reactivated when the immune system is depressed due to stressors such as trauma, infection or surgery (under general anaesthesia). Morphological changes to the inner ear of Ménière's sufferers has been found and is likely considered to have resulted from attack by the [[herpes simplex virus|herpes simplex virus.]] Symptoms then develop as the virus degrades the structure of the inner ear. Another consideration of utmost importance is that the different strains of herpes virus have different characteristics and in-turn different pathophysiological effects on the inner ear sensory organ system. | |||
* Middle ear and Upper Respiratory Tract Infections. | |||
* Medications - Aspirin use | |||
* Substance use - Tobacco and alcohol use | |||
* Electrolyte imbalance - Excessive levels of [[potassium]] in the body (usually caused by the consumption of potassium rich foods)can also exacerbate these symptoms. | |||
==Symptoms== | ==Symptoms== | ||
The symptoms of Ménière's are variable; not all sufferers experience the same symptoms. However, so-called "classic Ménière's" is considered to comprise the following four symptoms: | The symptoms of Ménière's are variable; not all sufferers experience the same symptoms. However, so-called "classic Ménière's" is considered to comprise of the following four symptoms: | ||
# Periodic episodes of rotary [[Vertigo (medical)|vertigo]] (the abnormal sensation of movement) or dizziness. | |||
# Fluctuating, progressive, unilateral (in one [[ear]]) or bilateral (in both ears) [[hearing loss]], sensorineural in origin and often initially in the low frequency ranges. | |||
# Unilateral or bilateral [[tinnitus]] (the perception of noises, often ringing, roaring, or whooshing), sometimes variable. | |||
# A sensation of fullness or pressure in one or both ears. | |||
* Ménière's often begins with one symptom, and gradually progresses. A diagnosis may be made in the absence of all four classic symptoms. However, having several symptoms at once is more conclusive than having every individual symptom associated with the disease at a separate time. | |||
* Attacks of vertigo can be severe, incapacitating, and unpredictable. In some patients, attacks of vertigo can last for hours or days, and may be accompanied by an increase in the loudness of tinnitus and temporary, albeit significant, hearing loss in the affected ear(s). Hearing may improve after an attack, but often becomes progressively worse. Vertigo attacks are sometimes accompanied by [[nausea]], [[vomiting]], and [[sweating]]. | |||
* Some sufferers experience what are informally known as "drop attacks"— sudden, severe attacks of dizziness or vertigo that causes the sufferers, if not seated, to fall. Patients may also experience the feeling of being pushed or pulled (Pulsion). Some patients may find it impossible to get up for some time, until the attack passes or medication takes its effect. There is also the associated risk of injury with falls | |||
Other symptoms include so-called "[[brain fog]]" (temporary loss of | * In addition to hearing loss, sounds can seem tinny or distorted, and patients can experience an unusual increased sensitivity to noises (hyperacusis). Some sufferers also experience [[nystagmus]], or uncontrollable rhythmical and jerky eye movements, usually in the horizontal plane, reflecting an essential role of the balance system in coordinating eye movements. | ||
* Other symptoms include the so-called "[[brain fog]]" (temporary short term loss of memory, forgetfulness, and confusion), exhaustion and drowsiness, headaches, vision problems, and depression, the latter symptoms are commonly associated with other chronic conditions | |||
*Women may experience an increase in the frequency of episodes during pregnancy and menstruation, the most likely reasoning behind this exacerbation is the increased fluid retention seen with these conditions. | |||
==Differential Diagnosis== | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diseases | |||
| colspan="5" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Clinical manifestations''' | |||
! colspan="2" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Para-clinical findings | |||
| colspan="1" rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Gold standard''' | |||
! rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Additional findings | |||
|- | |||
| colspan="4" rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Symptoms''' | |||
! rowspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Physical examination | |||
|- | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Lab Findings | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Imaging | |||
|- | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Acute onset | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Recurrency | |||
! colspan="1" rowspan="1" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Nystagmus | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Hearing problems | |||
|- | |||
| colspan="10" style="background: #7d7d7d; color: #FFFFFF; text-align: center;" |'''Peripheral''' | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Benign paroxysmal positional vertigo|BPPV]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* + [[Dix-Hallpike test|Dix-Hallpike maneuver]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Dix-Hallpike test|Dix-Hallpike maneuver]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May be associated with [[nausea]], [[vomiting]], and [[Gait abnormality|gait instability]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Vestibular neuronitis|Vestibular neuritis]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + /− | |||
(unilateral) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* + Head thrust test | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May be associated with [[nausea]], [[vomiting]], [[Gait abnormality|gait instability]] | |||
*Triggered by viral [[upper respiratory infection|upper respiratory tract infection]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ramsay Hunt syndrome type II|HSV oticus]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* loss of tastein the front two-thirds of the [[tongue]] | |||
* [[Acute facial nerve paralysis]] | |||
* [[Vesicles]] in the [[ear canal]], the [[tongue]], and/or [[hard palate]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + [[Varicella zoster virus|VZV]] antibody titres | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[Magnetic resonance imaging|MRI]] with [[gadolinium]] contrast may show enhancement of the [[facial nerve]] and [[vestibulocochlear nerve]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May be associated with [[otalgia]], [[dry mouth]] and [[dry eyes]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ménière's disease|Meniere disease]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + (Progressive) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Sensorineural hearing loss]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] may show small or invisible [[vestibular aqueduct]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
*Ruling out other CNS and ear pathologies. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May be associated with [[Nausea and vomiting|nausea]], [[Nausea and vomiting|vomiting]], and [[tinnitus]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Labyrinthine concussion<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[high frequency hearing loss]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] may show evidence of [[head trauma]] or [[temporal bone]] [[fracture]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Follows blunt [[head trauma]] | |||
* May be associated with [[dizziness]] or [[tinnitus]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Perilymphatic fistula]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Tullio phenomenon]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[CT scan]] may show fluid around the round window recess | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]]/[[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Complication of [[stapedectomy]], [[head injury]], or heavy lifting | |||
* It may be provoked by activities such as [[Sneeze|sneezing]], lifting, straining, [[Cough|coughing]], and loud sounds. (Tullio phenomenon) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Semicircular canal | |||
dehiscence syndrome<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
(air-bone gaps on audiometry) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Tullio phenomenon]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[CT scan]] may show defect in the arcuate eminence of the [[superior semicircular canal]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]]/[[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may be provoked by [[Valsalva maneuver]], [[Cough|coughing]], and [[Sneeze|sneezing]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Vestibular paroxysmia<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
(Induced by [[hyperventilation]]) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Impaired [[Caloric reflex test|caloric testing]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[MRI]] may show evidence of [[vestibulocochlear nerve]] compression | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
*Imaging | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may be provoked by head turning | |||
* Responds well to treatment with [[carbamazepine]] or [[oxcarbazepine]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Cogan syndrome]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | − | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Interstitial keratitis]] | |||
* [[Oscillopsia]] | |||
* Absent [[vestibular function]] on [[Caloric reflex test|caloric test]] | |||
* [[Systemic vasculitis]] ([[Aortitis]]) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Increased [[ESR]] and [[cryoglobulins]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] may show [[calcification]] or soft tissue attenuation obliterating the intralabyrinthine fluid spaces | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may cause [[Ménière's disease|Ménière]]-like attacks | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Vestibular schwannoma]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Sensorineural hearing loss]] | |||
* + [[Rinne test]] | |||
* Lateralization of [[Weber test]] to the normal [[ear]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] we may show erosion, and widening of the [[Internal auditory meatus|internal acoustic meatus]] | |||
* T1-weighted [[MRI]] may show a hypointense mass lesion where as T-2 weighted MRI shows a hyperintense [[mass]] lesion | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Gadolinium]]-enhanced [[MRI]] scan is the definitive diagnostic test for [[Vestibular schwannoma|acoutic neuroma]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Otitis media]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Fever | |||
* Presence of effusion in the [[middle ear]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Increased [[Acute phase reactant|acute phase reactants]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Opacification of the [[middle ear]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Patient may show other [[signs]] and [[symptoms]] of [[upper respiratory infection]] such as [[cough]], [[nasal discharge]], and [[fever]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Aminoglycoside toxicity<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Oscillopsia]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May be associated with [[nausea]], [[vomiting]], and [[ataxia]] | |||
* possibly irreversible | |||
* [[Gentamicin]] is the most common one | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Recurrent vestibulopathy<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/ Physical exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* The underlying [[pathophysiology]] is unknown | |||
* Frequency of episodes may vary, possibly an episode every one to two years. | |||
* It may be associated with [[nausea]] and [[vomiting]] | |||
* It may show an overlap of symptoms with vestibular [[migraine]] | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="10" style="background: #7d7d7d; color: #FFFFFF; text-align: center;" |Central | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Vestibular migraine<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* History of [[migraine headaches]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[MRI]] may show [[White matter|white-matter]] hyper-intensities (WMHs) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* ICHD-3 criteria | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may be associated with [[anxiety]] and [[depression]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Epileptic vertigo<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* They may experience [[loss of consciousness]] and motor/sensory problems | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[EEG]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Respond well to anti-[[seizure|epileptic]] drugs | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Multiple sclerosis]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Lhermitte's sign]] | |||
* [[Spasticity]] | |||
*[[Hyperreflexia]] | |||
* [[Internuclear ophthalmoplegia]] | |||
* [[Optic neuritis]] | |||
* [[Gait disturbance]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Elevated concentration of [[CSF]] [[oligoclonal bands]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] shows brain atrophy and contrast enhanced demyelinating plaques | |||
*[[MRI scan|MRI]] showing cerebral plaques disseminating in time and space. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History and physical examination]] | |||
* [[Imaging]] | |||
* [[CSF analysis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[MS]] is twice as prevalent in women as compared to men | |||
* The onset of [[symptoms]] is mostly between the age of fifteen to forty years and rarely before the age of fifteen or after the age of sixty years | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain tumor|Brain tumors]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Papilledema]] | |||
* [[Focal neurological deficits]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Cerebral spinal fluid ([[CSF]]) may show cancerous cells | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* On [[CT scan]] most of the [[brain tumors]] appears as a hypodense mass lesions | |||
* On T1- weighted [[MRI scan|MRI]] most of the [[brain tumors]] appears as a hypointense or Isointense whereas on T2-weighted [[MRI contrast agent|MRI]] they appear as hyperintense lesions | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
* [[Biopsy forceps|Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May experience [[headache]], [[seizures]], [[Visual disturbance|visual changes]] and changes in [[personality]], [[mood]] and [[concentration]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Cerebellar infarction]]/hemorrhage | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | ++/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Limb]] [[ataxia]] | |||
* [[Gait abnormality|Gait disturbance]] | |||
* [[Dysarthria]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Based on the time interval lapsed between the onset of [[stroke]] and [[imaging]] performed there may be different presentations | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Posterior inferior cerebellar artery]] is the most common artery that causes [[vertigo]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Brain stem ischemia | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Contralateral body [[Muscle weakness|weakness]] | |||
* [[Visual field]] deficits | |||
* [[Oculomotor nerve|Oculomotor]] abnormalities | |||
* [[Bulbar]] findings | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Based on the time interval lapsed between the onset of [[stroke]] and [[imaging]] performed there may be different presentations | |||
* For more information [[Ischemic stroke CT|click here]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may be associated with [[subclavian steal syndrome]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Chiari malformation]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Tachycardia]] | |||
* [[Pupillary dilatation]] | |||
* Impaired [[gag reflex]] | |||
* Impaired [[coordination]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] we may show [[hydrocephalus]], herniated [[cerebellar tonsils]], and a flattened [[spinal cord]] | |||
*[[MRI]] may show [[Cerebellar tonsil|cerebellar tonsillar]] [[herniation]], wedge shaped tonsils, syringohydromyelia, small [[posterior fossa]], obstructive [[hydrocephalus]], and [[brainstem]] anomalies | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* May present with ringing in the [[Ear|ears]] (Tinnitus) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Parkinson's disease|Parkinson]]<br> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Hypomimia]] | |||
* Cogwheel rigidity | |||
* Resting [[tremor]] | |||
* [[Gait Abnormalities|Gait problems]] | |||
* [[Bradykinesia]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |− | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
*[[CT scan]] is characterized by cortical and subcortical [[atrophy]] | |||
* [[MRI]] demonstrates a reduction in T2 relaxation time and reduced [[iron]] content in [[putamen]] and [[Globus pallidus|GPe]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History and physical examination]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Patients may present with slowness of movement ([[bradykinesia|bradykinesia),]]<nowiki/>resting [[tremor]]<nowiki/>and [[Muscle rigidity|muscle stiffness (rigidity)]]. | |||
|} | |||
'''ABBREVIATIONS''' | |||
[[VZV]]= [[Varicella zoster virus]], [[MRI]]= [[Magnetic resonance imaging]], [[ESR]]= [[Erythrocyte sedimentation rate]], [[EEG]]= [[Electroencephalogram]], [[CSF]]= [[Cerebrospinal fluid]], GPe= [[Globus pallidus|Globus pallidus externa]], ICHD= International Classification of Headache Disorders | |||
==Diagnosis== | ==Diagnosis== | ||
Many disorders have symptoms similar to Ménière's. The diagnosis is usually established by clinical findings and [[medical history]]. However, a detailed oto-neurological examination, [[audiometry]] and head [[magnetic resonance imaging]] (MRI) scan should be performed to exclude a [[tumour]] of the [[cranial nerve VIII]] (vestibulocochlear nerve) or [[superior canal dehiscence]] which would cause similar symptoms. Because there is no definitive test for Ménière's, it is only diagnosed when all other causes have been ruled out. | Many disorders have symptoms similar to Ménière's. The diagnosis is usually established by clinical findings and [[medical history]]. However, a detailed oto-neurological examination, [[audiometry]] and head [[magnetic resonance imaging]] (MRI) scan should be performed to exclude a [[tumour]] of the [[cranial nerve VIII]] (vestibulocochlear nerve) or [[superior canal dehiscence]] which would cause similar symptoms. Because there is no definitive test for Ménière's, it is only diagnosed when all other causes have been ruled out. | ||
Ménière’s disease typically starts between the ages of 20 and 50 years. Men and women are affected in equal numbers.- ''American Academy of Otolaryngology−Head and Neck Surgery'' | Ménière’s disease typically starts between the ages of 20 and 50 years. Men and women are affected in equal numbers.- ''American Academy of Otolaryngology−Head and Neck Surgery'' | ||
Ménière's typically begins between the ages of 30 and 60 and affects men slightly more than women. | Ménière's typically begins between the ages of 30 and 60 years and affects men slightly more than women. | ||
==Treatment== | ==Treatment== | ||
=== Medical Treatment === | |||
Initial treatment is targeted at relieving immediate symptoms and preventing recurrence of symptoms in the future and thus varies from patient to patient. Doctors may recommend vestibular training, methods for dealing with tinnitus, stress reduction, hearing aids to deal with hearing loss, and medication to alleviate nausea and symptoms of vertigo | |||
* Several environmental and dietary changes are thought to reduce the frequency or severity of symptom outbreaks. Most patients are advised to adopt a low-sodium diet, typically one to two grams (1000-2000mg) at first, but diets as low as 400mg are not uncommon. Patients are advised to avoid caffeine, alcohol and tobacco, all of which can aggravate symptoms of Ménière's. Some clinicians recommend avoiding [[Aspartame]]. | |||
*Very often patients are prescribed a mild diuretic to decrease the inner ear fluid build up. | |||
*Some patients also undergo allergen testing during initial evaluation as allergies have been shown to aggravate Ménière's symptoms.<ref name="Maryland" /> | |||
* Lipoflavonoid, a natural bioflavonoid that contains some of the B vitamins namely B3, B6 and B12 of the B vitamin complex is recommended for treatment of the tinnitus component of the disease by some physicians. | |||
Treatments aimed at lowering the pressure within the inner ear include [[antihistamine]]s, [[anticholinergic]]s, [[steroid]]s, and [[diuretic]]s. | * Many patients consider fluorescent light as a trigger for their symptoms. The plausibility of this can be explained by the vital role that vision plays in the overall mechanism of human balance. Avoidance of such triggers can be one such way to prevent these symptoms. | ||
* The anti herpesvirus drug Acyclovir has also been used with some success to treat Ménière's Disease.The likelihood of the effectiveness of the treatment was found to decrease with increasing duration of the disease possibly because of the overtime accumulation of viral damage to the inner ear and thus demonstrated that suppression of the virus made no significant difference to the symptoms if the exposure was present for prolonged periods. It was considered possible that long term treatment with an acyclovir (greater than six months) would be required to produce a remarkable reduction in symptomatology. Herpes viruses have the ability to remain dormant in nerve cells by a process known as [[HHV Latency Associated Transcript]]. Continued administration of the drug could prevent reactivation of the virus and allow for the possibility of an improvement in symptoms. | |||
*Treatments aimed at lowering the pressure within the inner ear include [[antihistamine]]s, [[anticholinergic]]s, [[steroid]]s, and [[diuretic]]s. A [http://www.meniett.com/ medical device] that provides transtympanic micropressure pulses is now showing some promising results and is becoming more widely used as a treatment for Ménière's..<ref name="Maryland" /> | |||
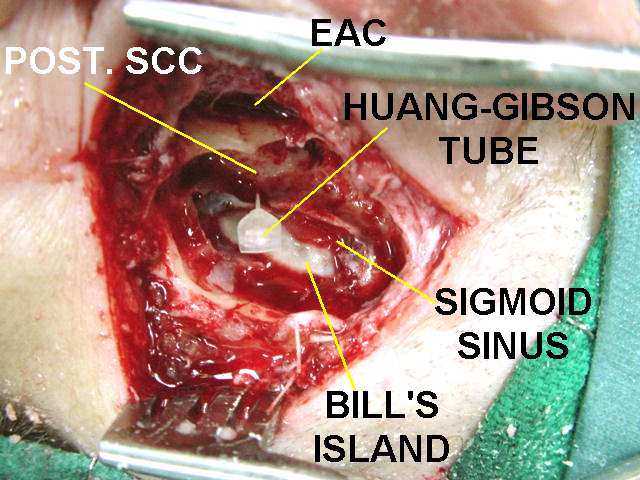
[[ | [[Image:Endolymphaticshuntlabeledgg.jpg|center|thumb|The '''endolymphatic shunt operation''' consists of opening the mastoid bone and identifying the endolymphatic sac which is located in the posterior fossa dura. To find the sac, the sigmoid sinus is denuded of its bony cover except for a small rectangle of thin bone named Bill's Island, after Dr. William House. The sigmoid sinus is then collapsed with gentle pressure and the sac exposed behind the posterior semicircular canal. The sac is then incised and a shunt tube is inserted. The picture on the right shows a Huang-Gibson tube with a one-way valve that allows fluid to seep out but not back into the sac. This procedure decreases the endolymphatic fluid pressure.]]<br /> | ||
=== Surgery === | |||
* Surgery may be recommended if medical management does not control vertigo. | |||
* Injection of steroid medication behind the eardrum, or surgery to decompress the endolymphatic sac may be used for symptom relief. Permanent surgical destruction of the balance part of the affected ear can be performed for severe or refractory cases if only one ear is affected. This can be achieved through chemical labyrinthectomy, in which a drug (such as [[gentamicin]]) that "kills" the vestibular apparatus is injected into the middle ear. The nerve responsible for the balance component of the inner ear can be cut ([[Vestibular nerve|vestibular]] [[neurectomy]]), or the inner ear itself can be surgically removed (labyrinthectomy). | |||
*These treatments eliminate vertigo, but since they are typically destructive they are implemented only as a last resort. Usually balance returns to normal after these procedures, but hearing loss may continue to progress.<ref name="Maryland" /> | |||
==Progression/Prognosis == | |||
Progression of Ménière's is unpredictable: symptoms may worsen, undergo complete resolution or remain the same. | |||
Patients with classical one or two symptoms may develop other symptoms over time. Attacks of vertigo can progressively worsen and increase in frequency over time, resulting in unemployment and the inability to drive and travel. Some patients become largely housebound. Hearing loss can become profound and more permanent. Some patients may also develop deafness in the affected ear. It is estimated that in fifty percent of the cases patients with unilateral symptoms will develop symptoms bilaterally. Tinnitus is also known to worsen over time. Some patients reported that after 8-10 years the vertigo attacks gradually became less frequent in severity; some patients reported that the symptoms disappeared completely. In some patients, symptoms of tinnitus disappear overtime and the hearing partially stabilises although typically with some permanent loss. | |||
==See also== | ==See also== | ||
| Line 111: | Line 514: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Diseases of the ear and mastoid process}} | {{Diseases of the ear and mastoid process}} | ||
{{DEFAULTSORT:Meniere's disease}} | {{DEFAULTSORT:Meniere's disease}} | ||
[[cs:Ménierova nemoc]] | [[cs:Ménierova nemoc]] | ||
[[de:Morbus Menière]] | [[de:Morbus Menière]] | ||
| Line 142: | Line 537: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Otology]] | |||
[[Category:Neurology]] | |||
[[Category:Otolaryngology]] | |||
[[Category:Overview complete]] | |||
[[Category:Disease]] | |||
<references /> | |||
Latest revision as of 22:17, 11 August 2020
| Ménière's disease | |
| ICD-10 | H81.0 |
|---|---|
| ICD-9 | 386.0 |
| OMIM | 156000 |
| DiseasesDB | 8003 |
| MedlinePlus | 000702 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sukaina Furniturewala, MBBS[2]
Overview
Ménière's disease is a disorder affecting the sensory organ within the inner ear responsible for balance and hearing. It is characterized by episodes of dizziness, tinnitus and progressive hearing loss, usually in one ear. This disturbance in the normal physiological functioning of the inner ear can be attributed to an increase in volume and pressure in the endolymph of the inner ear. The term "Ménière's" takes it origin after the French physician Prosper Ménière, who first reported that vertigo was caused by disorders of the inner ear in an article published in 1861.
Historical Background
Ménière's disease had been recognized prior to 1972 but the information available on its prevalence and understanding remained rather vague. Committees at the Academy of Ophthalmology and Otolaryngology made set criteria for diagnosing Ménière's, as well as defining two sub categories of Ménière's: cochlear (without vertigo) and vestibular (without deafness).
In 1972, the academy defined criteria for diagnosing Ménière's disease as:
- Fluctuating, progressive, sensorineural deafness.
- Episodic, characteristic definitive spells of vertigo lasting 20 minutes to 24 hours without loss of consciousness and associated with the presence of vestibular nystagmus .
- Usually tinnitus.
- Attacks are characterized by periods of remission and exacerbation.
In 1985, this list changed to alter wording, such as "deafness" changed to "hearing loss associated with tinnitus, characteristic of low frequencies" and requiring more than one attack of vertigo to diagnose. Finally in 1995, the list was again altered to allow for its documentation based on various degrees of probability of having the disease:
- Certain - Definite disease with histopathological confirmation
- Definite - Requires two or more definitive episodes of vertigo with hearing loss plus tinnitus and/or aural fullness
- Probable - Only one definitive episode of vertigo and the other symptoms and signs
- Possible - Definitive vertigo with no associated hearing loss
Cause
- Physiological -The exact cause of Ménière's disease is not known, but it is believed to be related to endolymphatic hydrops or excessive fluid in the inner ear. Several theories describing the causative mechanism have been proposed and documented, One such theory includes the decreased absorption or the increased production of the endolymph within the endolymphatic sac. This in-turn contributes to the swelling of the endolymphatic sac or other tissues in the vestibular system of the inner ear, a system responsible for the body's sense of balance which is disrupted a s a result of this pathology.
- Anatomical - Longitudinal blockage in the structures responsible for the drainage of the endolymph causing an increase in the hydrostatic pressure within the endolymphatic sac was another theory that was proposed to describe the possible structural cause behind the disease.
- Head trauma
- Infectious - It has also been proposed that Ménière's symptoms could be the result of damage caused by a the large family of DNA virus, herpesviridae. Herpesviridae is prevalent in the dormant state in a majority of the population. It is suggested that the virus is reactivated when the immune system is depressed due to stressors such as trauma, infection or surgery (under general anaesthesia). Morphological changes to the inner ear of Ménière's sufferers has been found and is likely considered to have resulted from attack by the herpes simplex virus. Symptoms then develop as the virus degrades the structure of the inner ear. Another consideration of utmost importance is that the different strains of herpes virus have different characteristics and in-turn different pathophysiological effects on the inner ear sensory organ system.
- Middle ear and Upper Respiratory Tract Infections.
- Medications - Aspirin use
- Substance use - Tobacco and alcohol use
- Electrolyte imbalance - Excessive levels of potassium in the body (usually caused by the consumption of potassium rich foods)can also exacerbate these symptoms.
Symptoms
The symptoms of Ménière's are variable; not all sufferers experience the same symptoms. However, so-called "classic Ménière's" is considered to comprise of the following four symptoms:
- Periodic episodes of rotary vertigo (the abnormal sensation of movement) or dizziness.
- Fluctuating, progressive, unilateral (in one ear) or bilateral (in both ears) hearing loss, sensorineural in origin and often initially in the low frequency ranges.
- Unilateral or bilateral tinnitus (the perception of noises, often ringing, roaring, or whooshing), sometimes variable.
- A sensation of fullness or pressure in one or both ears.
- Ménière's often begins with one symptom, and gradually progresses. A diagnosis may be made in the absence of all four classic symptoms. However, having several symptoms at once is more conclusive than having every individual symptom associated with the disease at a separate time.
- Attacks of vertigo can be severe, incapacitating, and unpredictable. In some patients, attacks of vertigo can last for hours or days, and may be accompanied by an increase in the loudness of tinnitus and temporary, albeit significant, hearing loss in the affected ear(s). Hearing may improve after an attack, but often becomes progressively worse. Vertigo attacks are sometimes accompanied by nausea, vomiting, and sweating.
- Some sufferers experience what are informally known as "drop attacks"— sudden, severe attacks of dizziness or vertigo that causes the sufferers, if not seated, to fall. Patients may also experience the feeling of being pushed or pulled (Pulsion). Some patients may find it impossible to get up for some time, until the attack passes or medication takes its effect. There is also the associated risk of injury with falls
- In addition to hearing loss, sounds can seem tinny or distorted, and patients can experience an unusual increased sensitivity to noises (hyperacusis). Some sufferers also experience nystagmus, or uncontrollable rhythmical and jerky eye movements, usually in the horizontal plane, reflecting an essential role of the balance system in coordinating eye movements.
- Other symptoms include the so-called "brain fog" (temporary short term loss of memory, forgetfulness, and confusion), exhaustion and drowsiness, headaches, vision problems, and depression, the latter symptoms are commonly associated with other chronic conditions
- Women may experience an increase in the frequency of episodes during pregnancy and menstruation, the most likely reasoning behind this exacerbation is the increased fluid retention seen with these conditions.
Differential Diagnosis
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard | Additional findings | |||||
|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | ||||||||
| Lab Findings | Imaging | ||||||||
| Acute onset | Recurrency | Nystagmus | Hearing problems | ||||||
| Peripheral | |||||||||
| BPPV |
+ | + | +/− | − | − | − |
| ||
| Vestibular neuritis |
+ | +/− | + /−
(unilateral) |
− |
|
− | − |
| |
| HSV oticus |
+ | +/− | − | +/− |
|
+ VZV antibody titres |
|
||
| Meniere disease |
+/− | + | +/− | + (Progressive) | − |
|
|
||
| Labyrinthine concussion |
+ | − | − | + | − |
|
| ||
| Perilymphatic fistula |
+/− | + | − | + | − |
|
| ||
| Semicircular canal
dehiscence syndrome |
+/− | + | − | +
(air-bone gaps on audiometry) |
− |
|
| ||
| Vestibular paroxysmia |
+ | + | +/−
(Induced by hyperventilation) |
− |
|
− |
|
|
|
| Cogan syndrome |
− | + | +/− | + | Increased ESR and cryoglobulins |
|
| ||
| Vestibular schwannoma |
− | + | +/− | + |
|
− |
|
| |
| Otitis media |
+ | − | − | +/− |
|
Increased acute phase reactants |
|
| |
| Aminoglycoside toxicity |
+ | − | − | + | − | − |
| ||
| Recurrent vestibulopathy |
+ | − | − | − | − | − | − |
| |
| Central | |||||||||
| Vestibular migraine |
– | + | +/− | +/− |
|
− |
|
|
|
| Epileptic vertigo |
− | + | +/− | − |
|
− | − |
| |
| Multiple sclerosis |
− | + | +/− | − | Elevated concentration of CSF oligoclonal bands | ||||
| Brain tumors |
+/− | + | + | + | Cerebral spinal fluid (CSF) may show cancerous cells |
|
| ||
| Cerebellar infarction/hemorrhage | + | − | ++/− | − | − |
| |||
| Brain stem ischemia | + | − | +/− | − |
|
− |
|
| |
| Chiari malformation |
− | + | + | − |
|
− |
|
| |
| Parkinson |
− | + | − | − | − |
| |||
ABBREVIATIONS
VZV= Varicella zoster virus, MRI= Magnetic resonance imaging, ESR= Erythrocyte sedimentation rate, EEG= Electroencephalogram, CSF= Cerebrospinal fluid, GPe= Globus pallidus externa, ICHD= International Classification of Headache Disorders
Diagnosis
Many disorders have symptoms similar to Ménière's. The diagnosis is usually established by clinical findings and medical history. However, a detailed oto-neurological examination, audiometry and head magnetic resonance imaging (MRI) scan should be performed to exclude a tumour of the cranial nerve VIII (vestibulocochlear nerve) or superior canal dehiscence which would cause similar symptoms. Because there is no definitive test for Ménière's, it is only diagnosed when all other causes have been ruled out.
Ménière’s disease typically starts between the ages of 20 and 50 years. Men and women are affected in equal numbers.- American Academy of Otolaryngology−Head and Neck Surgery
Ménière's typically begins between the ages of 30 and 60 years and affects men slightly more than women.
Treatment
Medical Treatment
Initial treatment is targeted at relieving immediate symptoms and preventing recurrence of symptoms in the future and thus varies from patient to patient. Doctors may recommend vestibular training, methods for dealing with tinnitus, stress reduction, hearing aids to deal with hearing loss, and medication to alleviate nausea and symptoms of vertigo
- Several environmental and dietary changes are thought to reduce the frequency or severity of symptom outbreaks. Most patients are advised to adopt a low-sodium diet, typically one to two grams (1000-2000mg) at first, but diets as low as 400mg are not uncommon. Patients are advised to avoid caffeine, alcohol and tobacco, all of which can aggravate symptoms of Ménière's. Some clinicians recommend avoiding Aspartame.
- Very often patients are prescribed a mild diuretic to decrease the inner ear fluid build up.
- Some patients also undergo allergen testing during initial evaluation as allergies have been shown to aggravate Ménière's symptoms.[1]
- Lipoflavonoid, a natural bioflavonoid that contains some of the B vitamins namely B3, B6 and B12 of the B vitamin complex is recommended for treatment of the tinnitus component of the disease by some physicians.
- Many patients consider fluorescent light as a trigger for their symptoms. The plausibility of this can be explained by the vital role that vision plays in the overall mechanism of human balance. Avoidance of such triggers can be one such way to prevent these symptoms.
- The anti herpesvirus drug Acyclovir has also been used with some success to treat Ménière's Disease.The likelihood of the effectiveness of the treatment was found to decrease with increasing duration of the disease possibly because of the overtime accumulation of viral damage to the inner ear and thus demonstrated that suppression of the virus made no significant difference to the symptoms if the exposure was present for prolonged periods. It was considered possible that long term treatment with an acyclovir (greater than six months) would be required to produce a remarkable reduction in symptomatology. Herpes viruses have the ability to remain dormant in nerve cells by a process known as HHV Latency Associated Transcript. Continued administration of the drug could prevent reactivation of the virus and allow for the possibility of an improvement in symptoms.
- Treatments aimed at lowering the pressure within the inner ear include antihistamines, anticholinergics, steroids, and diuretics. A medical device that provides transtympanic micropressure pulses is now showing some promising results and is becoming more widely used as a treatment for Ménière's..[1]
Surgery
- Surgery may be recommended if medical management does not control vertigo.
- Injection of steroid medication behind the eardrum, or surgery to decompress the endolymphatic sac may be used for symptom relief. Permanent surgical destruction of the balance part of the affected ear can be performed for severe or refractory cases if only one ear is affected. This can be achieved through chemical labyrinthectomy, in which a drug (such as gentamicin) that "kills" the vestibular apparatus is injected into the middle ear. The nerve responsible for the balance component of the inner ear can be cut (vestibular neurectomy), or the inner ear itself can be surgically removed (labyrinthectomy).
- These treatments eliminate vertigo, but since they are typically destructive they are implemented only as a last resort. Usually balance returns to normal after these procedures, but hearing loss may continue to progress.[1]
Progression/Prognosis
Progression of Ménière's is unpredictable: symptoms may worsen, undergo complete resolution or remain the same.
Patients with classical one or two symptoms may develop other symptoms over time. Attacks of vertigo can progressively worsen and increase in frequency over time, resulting in unemployment and the inability to drive and travel. Some patients become largely housebound. Hearing loss can become profound and more permanent. Some patients may also develop deafness in the affected ear. It is estimated that in fifty percent of the cases patients with unilateral symptoms will develop symptoms bilaterally. Tinnitus is also known to worsen over time. Some patients reported that after 8-10 years the vertigo attacks gradually became less frequent in severity; some patients reported that the symptoms disappeared completely. In some patients, symptoms of tinnitus disappear overtime and the hearing partially stabilises although typically with some permanent loss.
See also
References
Template:Diseases of the ear and mastoid process
cs:Ménierova nemoc
de:Morbus Menière
hr:Ménièreova bolest
it:Sindrome di Ménière
he:מחלת מנייר
nl:Ziekte van Ménière
no:Ménières sykdom
fi:Ménièren tauti
sv:Ménières sjukdom
Template:SIB