Iron deficiency anemia pathophysiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Physiology=== | ===Physiology=== | ||
*Iron is needed for the synthesis of haemoglobin, new DNA synthesis and is a major component of oxidation and reduction enzymes. | *Iron is needed for the synthesis of [[Hemoglobin|haemoglobin]], new [[DNA]] synthesis and is a major component of oxidation and reduction enzymes([[Cytochrome|cytochromes]]). | ||
*In the human body, iron mainly exists as bound to protein (hemoprotein), as heme compounds (hemoglobin or myoglobin), heme enzymes, or nonheme compounds (flavin-iron enzymes, | *In the human body, iron mainly exists as bound to protein (hemoprotein), as heme compounds (hemoglobin or myoglobin), heme enzymes, or nonheme compounds (flavin-iron enzymes, [[transferrin]], and [[ferritin]]). | ||
*The body requires iron for the synthesis of its oxygen transport proteins, (hemoglobin and myoglobin), and for the formation of heme enzymes and other iron-containing enzymes involved in electron transfer and oxidation-reductions. | *The body requires iron for the synthesis of its oxygen transport proteins, ([[hemoglobin]] and [[Myoglobin|myoglobin)]], and for the formation of heme enzymes and other iron-containing enzymes involved in electron transfer and oxidation-reductions. | ||
*Human iron metabolism is controlled by various factors. | *Human iron metabolism is controlled by various factors. | ||
*60% of the body iron is found in the hemoglobin present in circulating erythrocytes, 25% is contained in | *60% of the body iron is found in the hemoglobin present in circulating [[Red blood cell|erythrocytes]], 25% is contained in transferrin and ferritin, and the remaining 15% is bound to [[myoglobin]] in muscle tissue and in a variety of enzymes involved in the oxidative metabolism and many other cell functions. | ||
*Iron is bound and transported in the body via transferrin and stored in ferritin molecules. | *Iron is bound and transported in the body via transferrin and stored in ferritin molecules. | ||
*Iron is delivered to tissues by circulating transferrin, a transporter that captures iron released into the plasma from intestinal enterocytes or reticuloendothelial macrophages. | *Iron is delivered to tissues by circulating transferrin, a transporter that captures iron released into the plasma from intestinal enterocytes or reticuloendothelial [[Macrophage|macrophages]]. | ||
*The binding of transferrin to the cell-surface transferrin receptor (TfR) 1 results in endocytosis and uptake of iron. | *The binding of transferrin to the cell-surface transferrin receptor (TfR) 1 results in [[endocytosis]] and uptake of iron. | ||
*Internalized iron is transported to mitochondria for the synthesis of heme or other iron containing enzymes. | *Internalized iron is transported to [[Mitochondrion|mitochondria]] for the synthesis of heme or other iron containing enzymes. | ||
*Excess iron is stored in cytosolic ferritin. | *Excess iron is stored in cytosolic ferritin. | ||
====Absorption of iron==== | ====Absorption of iron==== | ||
*Iron absorption occurs by the enterocytes in the duodenum and upper jejunum. | *Iron absorption occurs by the [[Enterocyte|enterocytes]] in the [[duodenum]] and upper [[jejunum]]. | ||
*Dietary iron occurs in two forms: heme and nonheme. The primary sources of heme iron are hemoglobin and myoglobin from consumption of meat, poultry, and fish, whereas nonheme iron is obtained from cereals, pulses, legumes, fruits, and vegetables. | *Dietary iron occurs in two forms: heme and nonheme. The primary sources of heme iron are hemoglobin and myoglobin from consumption of meat, poultry, and fish, whereas nonheme iron is obtained from cereals, pulses, legumes, fruits, and vegetables. | ||
*In the blood, it is transported by transferrin to the cells or the bone marrow for erythropoiesis. | *In the blood, it is transported by transferrin to the cells or the [[bone marrow]] for [[erythropoiesis]]. | ||
*Iron absorption is controlled by ferroportin which allows or does not allow iron from the mucosal cell into the plasma. | *Iron absorption is controlled by ferroportin which allows or does not allow iron from the mucosal cell into the plasma. | ||
*Iron is absorbed in Fe<sup>+2</sup> (ferric) state | *Iron is absorbed in Fe<sup>+2</sup> (ferric) state | ||
*The iron is consumed in Fe+3 (ferrous) state and is reduced to Fe+2 state by the acidic gastric pH by enzyme ferric reductase. | *The iron is consumed in Fe+3 (ferrous) state and is reduced to Fe+2 state by the acidic [[Stomach|gastric]] pH by enzyme ferric reductase. | ||
* | * | ||
*Fe+2 is absorbed by the enterocytes and exported across the basolateral membrane into the bloodstream via Fe+2 transporter ferroportin. | *Fe+2 is absorbed by the enterocytes and exported across the basolateral membrane into the bloodstream via Fe+2 transporter [[ferroportin]]. | ||
*The ferroportin-mediated efflux of Fe+2 is coupled by its reoxidation to Fe+3, catalyzed by ferroxidase hephaestin that interacts with ferroportin. | *The ferroportin-mediated efflux of Fe+2 is coupled by its reoxidation to Fe+3, catalyzed by ferroxidase hephaestin that interacts with ferroportin. | ||
*The total iron content of transferrin is dynamic and undergoes changes to sustain erythropoiesis. | *The total iron content of transferrin is dynamic and undergoes changes to sustain [[erythropoiesis]]. | ||
*Senescent RBCs are cleared by reticuloendothelial macrophages, which metabolize hemoglobin and heme, and release iron into the bloodstream. | *Senescent RBCs are cleared by reticuloendothelial macrophages, which metabolize hemoglobin and heme, and release iron into the bloodstream. | ||
*The transferrin iron pool is replenished by iron recycled from RBCs and by newly absorbed dietary iron | *The transferrin iron pool is replenished by iron recycled from RBCs and by newly absorbed dietary iron | ||
*Macrophages export Fe+2 from their plasma membrane via ferroportin, in a process coupled by reoxidation of Fe+2 to Fe+3 by ceruloplasmin and followed by the loading of Fe+3 to transferrin. | *Macrophages export Fe+2 from their plasma membrane via ferroportin, in a process coupled by reoxidation of Fe+2 to Fe+3 by [[ceruloplasmin]] and followed by the loading of Fe+3 to transferrin. | ||
====Regulation of iron homeostasis==== | ====Regulation of iron homeostasis==== | ||
*Iron balance is mainly regulated at the point of absorption. | *Iron balance is mainly regulated at the point of absorption. | ||
*Hepcidin is a circulating peptide hormone secreted by the liver that plays a central role in the regulation of iron homeostasis. | *[[Hepcidin]] is a circulating peptide [[hormone]] secreted by the liver that plays a central role in the regulation of iron homeostasis. | ||
*This hormone is produced by hepatocytes and is a negative regulator of iron entry into plasma. | *This hormone is produced by [[Hepatocyte|hepatocytes]] and is a negative regulator of iron entry into plasma. | ||
*Hepcidin acts by binding to ferroportin. | *Hepcidin acts by binding to ferroportin. | ||
*Binding of hepcidin induces ferroportin degradation. | *Binding of hepcidin induces ferroportin degradation. | ||
*The loss of ferroportin from the cell surface prevents iron entry into plasma and decreased iron levels in the body. | *The loss of ferroportin from the cell surface prevents iron entry into [[Blood plasma|plasma]] and decreased iron levels in the body. | ||
*Decreased expression of hepcidin leads to increased cell surface ferroportin and increased iron absorption. | *Decreased expression of hepcidin leads to increased cell surface ferroportin and increased iron absorption. | ||
*Plasma hepcidin levels are regulated by cytokines, plasma iron, anemia, and hypoxia. | *Plasma hepcidin levels are regulated by [[Cytokine|cytokines]], plasma iron, [[anemia]], and [[Hypoxemia|hypoxia]]. | ||
*Overexpression of hepcidin leads to the anemia of chronic disease, while low hepcidin production results in hereditary hemochromatosis | *Overexpression of hepcidin leads to the anemia of chronic disease, while low hepcidin production results in hereditary [[hemochromatosis]] (HFE). | ||
====Storage==== | ====Storage==== | ||
*Ferritin concentration together with that of hemosiderin reflects the body iron stores. | *Ferritin concentration together with that of [[hemosiderin]] reflects the body iron stores. | ||
*They store iron in an insoluble form and are present primarily in the liver, spleen, and bone marrow. | *They store iron in an insoluble form and are present primarily in the liver, spleen, and bone marrow. | ||
*Serum ferritin is the most convenient laboratory test to estimate iron stores. | *Serum ferritin is the most convenient laboratory test to estimate iron stores. | ||
====Factors effecting iron absorption==== | ====Factors effecting iron absorption==== | ||
*Factors that enhance iron uptake are: | *Factors that enhance iron uptake are: | ||
**Ascorbate and citrate increase iron uptake by acting as weak chelators. | **[[Vitamin C|Ascorbate]] and [[citrate]] increase iron uptake by acting as weak chelators. | ||
**Iron is readily transferred from these compounds into the mucosal lining cells. | **Iron is readily transferred from these compounds into the mucosal lining cells. | ||
*Factors inhibiting iron absorption are: | *Factors inhibiting iron absorption are: | ||
**Phytate (myo-inositol hexakisphosphate) is the main inhibitor of iron absorption. | **[[Phytic acid|Phytate]] (myo-inositol hexakisphosphate) is the main inhibitor of iron absorption. | ||
**Calcium | **[[Calcium]] | ||
**Animal proteins such as milk proteins, egg proteins, and albumin, have been shown to inhibit iron absorption. | **Animal proteins such as milk proteins, egg proteins, and [[albumin]], have been shown to inhibit iron absorption. | ||
**Proteins from soybean also decrease iron absorption. | **Proteins from [[soybean]] also decrease iron absorption. | ||
**Suppresion of | **Suppresion of [[gastric acid]] such as use of [[Antacid|antacids]] suprress iron absorption. | ||
**Lead competes with iron for the absorption and blocks its absorption by competetive inhibition. | **Lead competes with iron for the absorption and blocks its absorption by competetive inhibition. | ||
====Iron requirement==== | ====Iron requirement==== | ||
| Line 125: | Line 124: | ||
**Increased demands of iron. | **Increased demands of iron. | ||
**Impaired absorption of iron. | **Impaired absorption of iron. | ||
**Excessive loss of iron (blood loss). | **Excessive loss of iron ([[Bleeding|blood loss]]). | ||
**Increased hepcidin (chronic inflammation) | **Increased hepcidin (chronic [[inflammation]]) | ||
*Low dietary intake: | *Low dietary intake: | ||
**Iron is obtained from foods such as: | **Iron is obtained from foods such as: | ||
| Line 136: | Line 135: | ||
***eggs | ***eggs | ||
***seafood, such as clams, sardines, shrimp, and oysters | ***seafood, such as clams, sardines, shrimp, and oysters | ||
*** | ***Iron-fortified dry and instant cereals Foods high in vitamin C include: | ||
*** | ***Fruits such as oranges, grapefruits, strawberries, kiwis, guavas, papayas, pineapples, melons, and mangoes | ||
*** | ***Red and green bell peppers | ||
***Brussels sprouts | ***Brussels sprouts | ||
*** | ***Cauliflower | ||
*** | ***Tomatoes | ||
*** | ***Leafy greens | ||
**Increased demands of iron | **Increased demands of iron | ||
***Growth, the requirement of iron increases during the developmental period from infancy to adolescence and during adolescence. | ***Growth, the requirement of iron increases during the developmental period from [[Infant|infancy]] to [[adolescence]] and during adolescence. | ||
***Pregnancy, during pregnancy the demand for iron is increased. | ***[[Pregnancy]], during pregnancy the demand for iron is increased. | ||
**Impaired absorption of iron: | **Impaired absorption of iron: | ||
***[[Malabsorption]] | ***[[Malabsorption]] | ||
***Deficiency of vitamin C in diet. | ***Deficiency of vitamin C in diet. | ||
**Excessive loss of iron (blood loss) | **Excessive loss of iron (blood loss) | ||
***The only means of | ***The only means of excretion for iron is through blood loss. | ||
***Any source of external and internal bleeding can cause iron deficiency depending on the blood loss. | ***Any source of external and internal bleeding can cause iron deficiency depending on the blood loss. | ||
**Increased hepcidin | **Increased hepcidin | ||
***In chonric inflammatory conditions, the levels of hepcidin increase. | ***In chonric [[Inflammation|inflammatory]] conditions, the levels of hepcidin increase. | ||
***Increased hepcidin causes ferriportin degeneration and impaired iron absorption. | ***Increased hepcidin causes ferriportin degeneration and impaired iron absorption. | ||
*Iron is required for haemoglobin synthesis, so deficiency of iron leads to depletion of haemoglobin. | *Iron is required for [[Hemoglobin|haemoglobin]] synthesis, so deficiency of iron leads to depletion of haemoglobin. | ||
*Decrease in haemoglobin leads to anemia. | *Decrease in haemoglobin leads to [[anemia]]. | ||
*Due to low haemoglobin, oxygen is not tranported effectively to cells and results in hypoxia. | *Due to low haemoglobin, oxygen is not tranported effectively to cells and results in [[hypoxia]]. | ||
{| class="wikitable" | {| class="wikitable" | ||
!Population | !Population | ||
Revision as of 15:13, 5 September 2018
|
Iron deficiency anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Iron deficiency anemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Iron deficiency anemia pathophysiology |
|
Risk calculators and risk factors for Iron deficiency anemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Please help WikiDoc by adding content here. It's easy! Click here to learn about editing.
Overview
Pathophysiology
Physiology
- Iron is needed for the synthesis of haemoglobin, new DNA synthesis and is a major component of oxidation and reduction enzymes(cytochromes).
- In the human body, iron mainly exists as bound to protein (hemoprotein), as heme compounds (hemoglobin or myoglobin), heme enzymes, or nonheme compounds (flavin-iron enzymes, transferrin, and ferritin).
- The body requires iron for the synthesis of its oxygen transport proteins, (hemoglobin and myoglobin), and for the formation of heme enzymes and other iron-containing enzymes involved in electron transfer and oxidation-reductions.
- Human iron metabolism is controlled by various factors.
- 60% of the body iron is found in the hemoglobin present in circulating erythrocytes, 25% is contained in transferrin and ferritin, and the remaining 15% is bound to myoglobin in muscle tissue and in a variety of enzymes involved in the oxidative metabolism and many other cell functions.
- Iron is bound and transported in the body via transferrin and stored in ferritin molecules.
- Iron is delivered to tissues by circulating transferrin, a transporter that captures iron released into the plasma from intestinal enterocytes or reticuloendothelial macrophages.
- The binding of transferrin to the cell-surface transferrin receptor (TfR) 1 results in endocytosis and uptake of iron.
- Internalized iron is transported to mitochondria for the synthesis of heme or other iron containing enzymes.
- Excess iron is stored in cytosolic ferritin.
Absorption of iron
- Iron absorption occurs by the enterocytes in the duodenum and upper jejunum.
- Dietary iron occurs in two forms: heme and nonheme. The primary sources of heme iron are hemoglobin and myoglobin from consumption of meat, poultry, and fish, whereas nonheme iron is obtained from cereals, pulses, legumes, fruits, and vegetables.
- In the blood, it is transported by transferrin to the cells or the bone marrow for erythropoiesis.
- Iron absorption is controlled by ferroportin which allows or does not allow iron from the mucosal cell into the plasma.
- Iron is absorbed in Fe+2 (ferric) state
- The iron is consumed in Fe+3 (ferrous) state and is reduced to Fe+2 state by the acidic gastric pH by enzyme ferric reductase.
- Fe+2 is absorbed by the enterocytes and exported across the basolateral membrane into the bloodstream via Fe+2 transporter ferroportin.
- The ferroportin-mediated efflux of Fe+2 is coupled by its reoxidation to Fe+3, catalyzed by ferroxidase hephaestin that interacts with ferroportin.
- The total iron content of transferrin is dynamic and undergoes changes to sustain erythropoiesis.
- Senescent RBCs are cleared by reticuloendothelial macrophages, which metabolize hemoglobin and heme, and release iron into the bloodstream.
- The transferrin iron pool is replenished by iron recycled from RBCs and by newly absorbed dietary iron
- Macrophages export Fe+2 from their plasma membrane via ferroportin, in a process coupled by reoxidation of Fe+2 to Fe+3 by ceruloplasmin and followed by the loading of Fe+3 to transferrin.
Regulation of iron homeostasis
- Iron balance is mainly regulated at the point of absorption.
- Hepcidin is a circulating peptide hormone secreted by the liver that plays a central role in the regulation of iron homeostasis.
- This hormone is produced by hepatocytes and is a negative regulator of iron entry into plasma.
- Hepcidin acts by binding to ferroportin.
- Binding of hepcidin induces ferroportin degradation.
- The loss of ferroportin from the cell surface prevents iron entry into plasma and decreased iron levels in the body.
- Decreased expression of hepcidin leads to increased cell surface ferroportin and increased iron absorption.
- Plasma hepcidin levels are regulated by cytokines, plasma iron, anemia, and hypoxia.
- Overexpression of hepcidin leads to the anemia of chronic disease, while low hepcidin production results in hereditary hemochromatosis (HFE).
Storage
- Ferritin concentration together with that of hemosiderin reflects the body iron stores.
- They store iron in an insoluble form and are present primarily in the liver, spleen, and bone marrow.
- Serum ferritin is the most convenient laboratory test to estimate iron stores.
Factors effecting iron absorption
- Factors that enhance iron uptake are:
- Factors inhibiting iron absorption are:
- Phytate (myo-inositol hexakisphosphate) is the main inhibitor of iron absorption.
- Calcium
- Animal proteins such as milk proteins, egg proteins, and albumin, have been shown to inhibit iron absorption.
- Proteins from soybean also decrease iron absorption.
- Suppresion of gastric acid such as use of antacids suprress iron absorption.
- Lead competes with iron for the absorption and blocks its absorption by competetive inhibition.
Iron requirement
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 0.27 mg* | 0.27 mg* | ||
| 7–12 months | 11 mg | 11 mg | ||
| 1–3 years | 7 mg | 7 mg | ||
| 4–8 years | 10 mg | 10 mg | ||
| 9–13 years | 8 mg | 8 mg | ||
| 14–18 years | 11 mg | 15 mg | 27 mg | 10 mg |
| 19–50 years | 8 mg | 18 mg | 27 mg | 9 mg |
| 51+ years | 8 mg | 8 mg |
Pathogenesis
- Iron deficiency anemia occurs when there is:
- Low dietary intake.
- Increased demands of iron.
- Impaired absorption of iron.
- Excessive loss of iron (blood loss).
- Increased hepcidin (chronic inflammation)
- Low dietary intake:
- Iron is obtained from foods such as:
- meat, such as lamb, pork, chicken, and beef
- beans
- pumpkin and squash seeds
- leafy greens, such as spinach
- raisins and other dried fruit
- eggs
- seafood, such as clams, sardines, shrimp, and oysters
- Iron-fortified dry and instant cereals Foods high in vitamin C include:
- Fruits such as oranges, grapefruits, strawberries, kiwis, guavas, papayas, pineapples, melons, and mangoes
- Red and green bell peppers
- Brussels sprouts
- Cauliflower
- Tomatoes
- Leafy greens
- Increased demands of iron
- Growth, the requirement of iron increases during the developmental period from infancy to adolescence and during adolescence.
- Pregnancy, during pregnancy the demand for iron is increased.
- Impaired absorption of iron:
- Malabsorption
- Deficiency of vitamin C in diet.
- Excessive loss of iron (blood loss)
- The only means of excretion for iron is through blood loss.
- Any source of external and internal bleeding can cause iron deficiency depending on the blood loss.
- Increased hepcidin
- In chonric inflammatory conditions, the levels of hepcidin increase.
- Increased hepcidin causes ferriportin degeneration and impaired iron absorption.
- Iron is obtained from foods such as:
- Iron is required for haemoglobin synthesis, so deficiency of iron leads to depletion of haemoglobin.
- Decrease in haemoglobin leads to anemia.
- Due to low haemoglobin, oxygen is not tranported effectively to cells and results in hypoxia.
| Population | Hb Diagnostic of anaemia (g/dL)a |
|---|---|
| Children aged 6 months to 6 years old | <11.0 |
| Children aged 6-14 years old | <12.0 |
| Adult men | <13.0 |
| Adult non-pregnant women | <12.0 |
| Adult pregnant women | <11.0 |
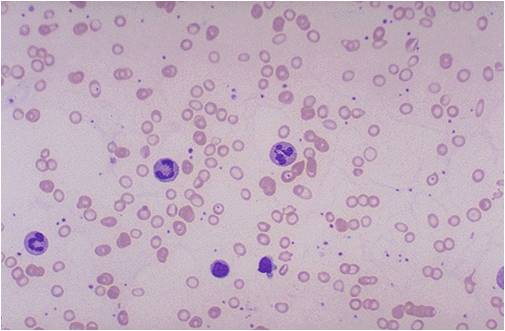
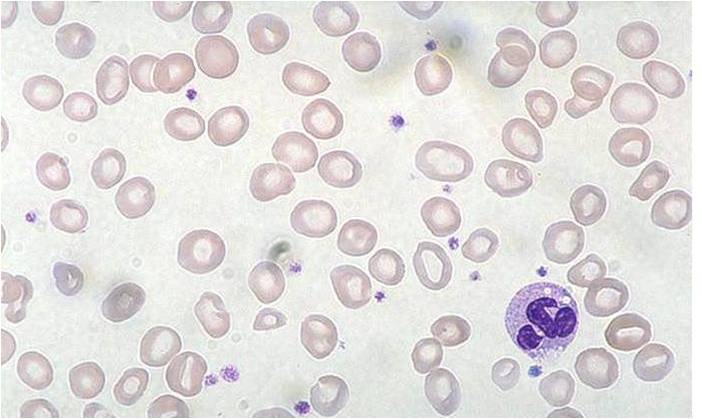
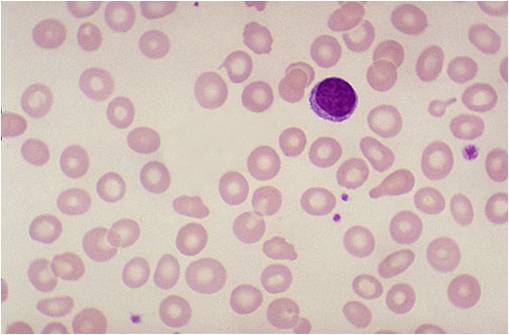
Histology
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey)
-
Iron deficiency anemia
-
Iron deficiency anemia
-
Iron deficiency anemia
Video
{{#ev:youtube|7uDbu7esZik}}
External Link
Center for disease control and prevention