Hyperlipoproteinemia type 5: Difference between revisions
| Line 13: | Line 13: | ||
== Classification == | == Classification == | ||
=== Classification by Severity of | === Classification by Severity of Triglycerides === | ||
Hypertriglyceridemia may be classified according to the concentration of [[triglycerides]] on the [[lipid profile]]. More marked elevations are usually seen in cases of hypertriglyceridemia resulting from secondary causes.<ref name="pmid12485966">{{cite journal| author=National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)| title=Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. | journal=Circulation | year= 2002 | volume= 106 | issue= 25 | pages= 3143-421 | pmid=12485966 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12485966 }} </ref> | Hypertriglyceridemia may be classified according to the concentration of [[triglycerides]] on the [[lipid profile]]. More marked elevations are usually seen in cases of hypertriglyceridemia resulting from secondary causes.<ref name="pmid12485966">{{cite journal| author=National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)| title=Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. | journal=Circulation | year= 2002 | volume= 106 | issue= 25 | pages= 3143-421 | pmid=12485966 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12485966 }} </ref> | ||
Revision as of 20:55, 28 November 2016
|
Hyperlipoproteinemia Microchapters |
|
ACC/AHA Guideline Recommendations |
|
Intensity of statin therapy in primary and secondary prevention |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ;Associate Editor(s)-in-Chief: Shivani Chaparala M.B.B.S [2] Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [3]
Synonyms and keywords: : Hyperchylomicronemia, Late-Onset Hyperchylomicronemia With Hyperprebetalipoproteinemia, Familial mixed hyperlipidemia, Type V hyperlipemia, Hyperlipidemia type V, Type 5 hyperlipoproteinemia, Type 5 hyperlipemia, Type 5 HLP, Type V HLP, Combined fat and carbohydrate Induced hyperlipidemia, Mixed hypertriglyceridemia, Endogenous hypertriglyceridemia.
Overview
Type 5 Hyperlipoproteinemia (HLP V) is a rare disorder of lipo-protein metabolism characterized by fasting chylomicronemia and elevated levels of cholesterol in the very low density (VLD) lipoprotein fraction. The triglyceride(TG) levels are invariably greater than 1000mg/dl thereby increasing the risk of pancreatitis.It has been postulated that HLP V is the result of a defective clearance of TG-rich lipoproteins(VLDLs and Chylomicrons),although lipoprotein lipase is not absent. Another suggested mechanism is of VLDL TG's overproduction. Some patients seem to have "Primary" HLP V which usually appears first in adulthood,this phenotype is often associated with secondary factors,almost always Diabetes Mellitus.May be associated with Eruptive Xanthomas and Hyperuricemia. The primary goal of therapy is to reduce the TG level to <500mg/dl for the intent of reducing the risk of pancreatitis.
Historical Perspective
- In 1967, Dr. Fredrickson classified lipoprotein disorders using paperelectrophoresis.[1]
Classification
Classification by Severity of Triglycerides
Hypertriglyceridemia may be classified according to the concentration of triglycerides on the lipid profile. More marked elevations are usually seen in cases of hypertriglyceridemia resulting from secondary causes.[2]
- Normal triglycerides: <150 mg/dL
- Borderline-high triglycerides: 150-199 mg/dL
- High triglycerides: 200-499 mg/dL
- Very high triglycerides: >500 mg/dL
To view the ATPIII guidelines for classification of triglyceride levels click here.
Pathophysiology
The two main sources of plasma triglycerides (also known as triacylglycerol) are exogenous (i.e., from dietary fat) and carried in chylomicrons, and endogenous (from the liver) and carried in very-low-density lipoprotein (VLDL) particles. In capillaries within fat and muscle tissue, these lipoproteins and chylomicrons are hydrolyzed by lipoprotein lipase into free fatty acids. After a meal, over 90% of the circulating triglycerides originate in the intestine and are secreted in chylomicrons, whereas during periods of fasting, endogenous triglycerides secreted by the liver as VLDL predominate. The increase in plasma of triglyceride-rich lipoproteins results from increased production from the liver and intestine (by means of upregulated synthetic and secretory pathways) or through decreased peripheral catabolism (mainly from reduced lipoprotein lipase activity).
Pathogenesis
The pathogenesis of type V is not fully understood. However; VLDL appears to be the most affected lipoprotein fraction in type V and there is three-fold increase in synthesis rate as well as decreased fractional catabolism of VLDL.The molecular basis for Type V HLP is not clearly understood.Apolipoprotein E mutation type V hyperlipoproteinaemia is associated predominantly with TG-rich lipoproteins (chylomicrons and VLDL) and has also been detected on HDL particles.Mutations in the APOA5 gene, leading to truncated apolipoprotein A-V devoid of lipid-binding domains located in the carboxy-terminal end of the protein, if present in the homozygous state, are expected to cause severe type V hyperlipidemia in patients with no mutations in LPL or APOC2 genes.[3] If present in the heterozygous state, these mutations predispose to hypertriglyceridemia in combination with other genetic factors or pathological conditions.The absence of manifestations until middle age, suggest that the cause of type V hyperlipoproteinemia(HLP) is multifactorial including a combination of environmental, hormonal and genetic factors.[3] In patients with type V HLP, the presence of underlying diseases or contributing factors such as Diabetes and alcohol abuse is confirm in ~67% of patients and the remaining patients usually show type IV HLP and have hypertriglyceridemia in the family.Transiently impaired LPL activity with no defect in LPL enzyme induced severe hypertriglyceridemia in infants. The transient occurrence of inhibitor(s) for LPL was proposed.[3]
Genetics
Precise genetic patterns have not been determined for type V HLP and it has been suggested that type V may be due to number of genetic defects. Among them, the apo E and its isoforms may have an important clinical significance in type V HLP and may affect the catabolism of triglyceride rich lipoproteins. The presence of apo E4 allele may be the genetic factor that predisposes to the development of type V due to delayed lipoprotein clearance.
Associated Conditions
- diabetes mellitus
- alcohol abuse
- glycogen storage disease type I
- Hyperuricemia
- Pancreatitis
- xanthomatosis.
Causes
Type V hyperlipoproteinemia is more complicated and more closely related to acquired environmental factors. It rarely shows familial occurrence, but its inheritance is variable. Therefore, type V HLP is usually considered to be triggered by acquired environmental factors in individuals with some congenital susceptibility to altered triglyceride metabolism (genetic factors). While the involved environmental factors vary, involvement of heavy drinking, type 2 Diabetes, hormonal therapy and medications are frequently observed.[3]
Causes by Pathophysiology
| Congenital (Genetic) Factors | Acquired (Environmental) Factors |
|---|---|
|
Differentiating HLP type 5 from other Hyperlipoproteinemias with raised triglycerides
HLP type 5 must be differentiated from other diseases that cause abnormal increase in triglycerides in the blood.
- Familial hyperchylomicronemia
- Familial hypercholesterolemia/ Familial combined hyperlipidemia
- Dysbetalipoprotenemia
- Primary hypertriglyceridemia/ Primary hypertriglyceridemia
- Drugs Causing high triglyceride levels:[4]
- Atypical antipsychotic drugs(Fluperlapine, Clozapine, Olanzapine), Beta-blockers (especially non-beta 1-selective), Bile acid sequestrants, Cyclophosphamide, Glucocorticoids, Immunosuppressive drugs (Cyclosporine, Sirolimus), Interferon, L-asparaginase, Oral estrogens, Protease inhibitors, Raloxifene, Retinoids, Rosiglitazone, Tamoxifen, Thiazide diuretics.
Epidemiology and Demographics
Prevalence/Incidence
It is difficult to accurately estimate the prevalence of HLP V in the general population, but a survey of about 40,000 people by the Lipid Research Clinic reported the frequency of individuals with a plasma TG level of 2,000 mg/dl or higher to be about 0.018%
Age
Average triglyceride levels in type V hyperlipoproteinemia were lower for women than for men before age 50.[5]
Gender
Race
In Western population, LPL gene abnormalities were observed in 10% of patients with type V HLP.
Risk Factors
- Family history of dyslipoproteinemia
- Diabetes
- Alcohol abuse
- Obesity
Screening
Natural History, Complications and Prognosis
Natural History
Mixed hyperlipidemia—a common disorder that becomes more prevalent with increasing age.A history of acute pancreatitis was observed in about 17% of the patients, demonstrating that hyperlipidemia is frequently complicated by pancreatitis also in Japanese, in whom the fat intake is lower than in Western people, and stressing the importance of its prevention and management.
Complications
Prognosis
The prognosis is uncertain due to the risk of Pancreatitis.Increased fat intake may cause recurrent bouts of illness possibly leading to pseudocyst formation,hemorrhage and death.
Diagnosis
Diagnostic Criteria
- I. Demonstration of an increase in VLDL in addition to hyperchylomicronemia.
- II. The absence of LPL deficiency, Apolipoprotein C-II deficiency, Apo E deficiency.
Definitely diagnosed if both I and II are fulfilled.
- Fasting chylomicronemia can be diagnosed by confirming the presence of chylomicrons and excess VLDL on agarose gel electrophoresis or ultracentrifugal analysis. A simple technique is to refrigerate plasma overnight and examine the specimen for a creamy supernatant from chylomicrons and a turbid VLDL-rich infranatant.This latter finding of a turbid infranatant is not seen in patients with type I hyperlipoproteinemia, in which only chylomicrons accumulate and the infranatant is clear.
History and Symptoms
- Recurrent abdominal pain
- Eruptive xanthomas
- Family history of Diabetes
Physical Examination
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
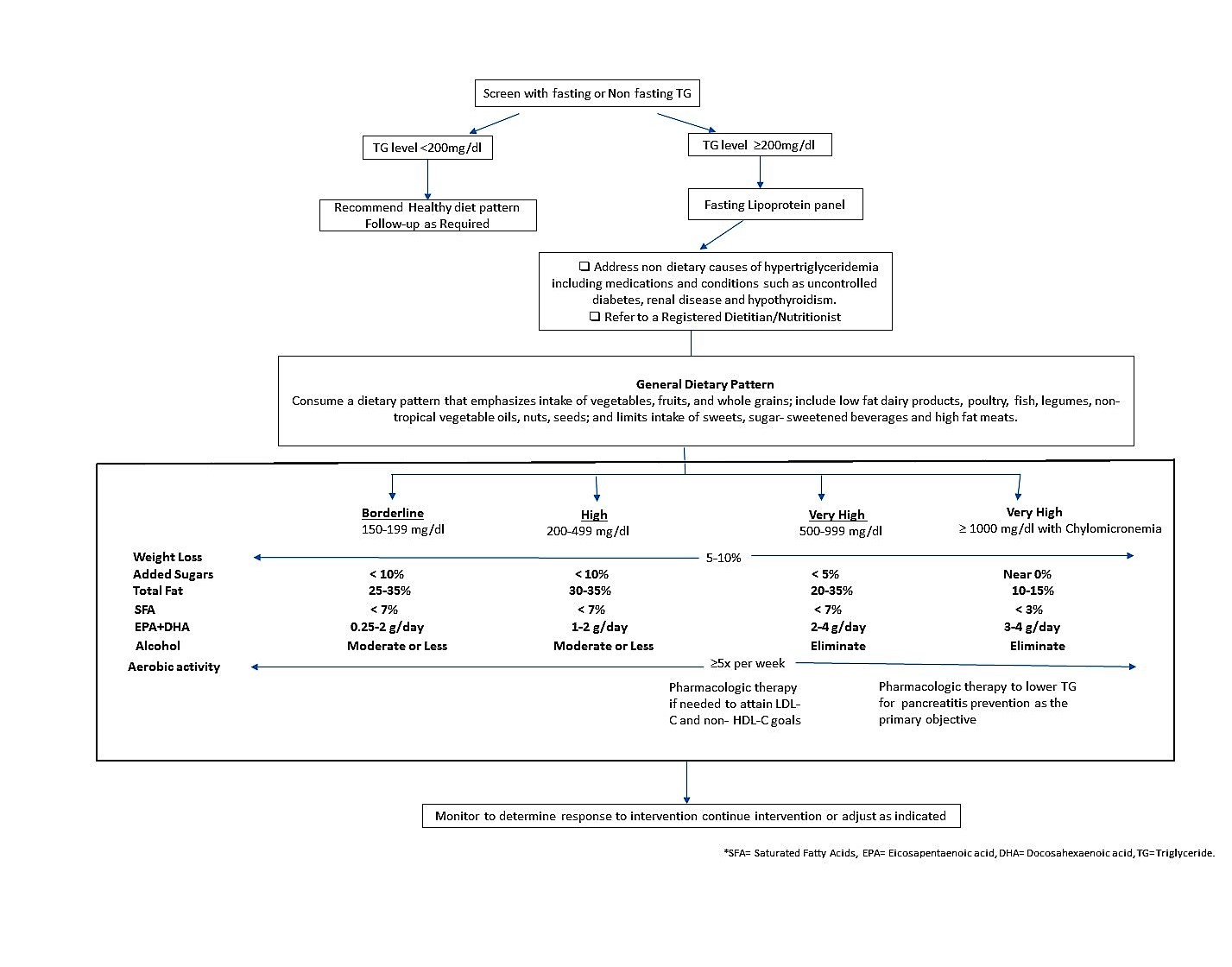
The evaluation and treatment decisions of type 5 HLP should be based on patient-centered and individual circumstances. Lifestyle therapies, such as appropriate nutrition and physical activity, are important elements of ASCVD risk reduction, with or without lipid-altering drug therapy. For patients in whom lipid-altering drug therapy is indicated, statin treatment is the primary pharmacologic modality for reducing ASCVD risk.
Clinical algorithm for screening and management of elevated TG[6]
Medical Therapy
When the triglyceride concentration is very high (≥500 mg/dL, and especially if ≥1000 mg/dL), the primary goal of therapy is to reduce the triglyceride level to <500 mg/dL for the intent of reducing the risk of pancreatitis.
| Triglyceride concentration | First line of therapy |
|---|---|
| ≥1000mg/dl | Triglyceride lowering agents such as ❑ Fibric acids ❑ High-dose [2 to 4 g/d] long-chain omega-3 fatty acids ❑ Nicotinic acid |
| 500-999mg/dl | ❑ Triglyceride lowering agents, ❑ Statins |
| 200-499mg/dl | Statin will generally be first-line drug therapy.If maximum tolerated statin therapy does not lower non-HDL-C below goal levels in patients with triglycerides 200 to 499 mg/dL, adding an agent that primarily lowers triglycerides may help to achieve atherogenic cholesterol goals. |
When triglycerides are between 200 and 499mg/dL, the primary targets of lipid therapy are non–HDL-C and LDL-C for the purpose of reducing ASCVD risk.
| Lipid treatment goals to reduce ASCVD risk[6] | ||
|---|---|---|
| Risk of ASCVD | Indication for drug therapy | Goal of drug therapy |
| Low ASCVD risk | Non HDL- C* level ≥190mg/dl LDL-C level ≥160mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| Moderate ASCVD risk | Non HDL- C* level ≥160mg/dl LDL-C level ≥130mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| High ASCVD risk | Non HDL- C level ≥130mg/dl LDL-C level ≥100mg/dl |
Non HDL- C level <130mg/dl LDL-C level <100mg/dl |
| Very high ASCVD risk | Non HDL- C level ≥100mg/dl LDL-C level ≥70mg/dl |
Non HDL- C level <100mg/dl LDL-C level <70mg/dl |
Non–HDL-C comprises the cholesterol carried by all atherogenic particles, including LDL, intermediatedensity lipoproteins, very low-density lipoproteins (VLDL) and VLDL remnants, chylomicron remnants, and lipoprotein.[7]
Surgery
The effect of bariatric surgery on lipid levels is variable and dependent upon the type of bariatric surgical procedure (e.g., gastric bypass, gastric sleeve, adjustable gastric banding).Gastric bypass procedures generally produce greater improvements in lipid and other metabolic parameters because of greater reductions in body fat, alterations in gut and other hormones, and improvements in inflammatory factors.[7]Bariatric surgery significantly improved multiple metabolic parameters, and reduced overall mortality.Regarding lipids, compared with conventional therapy, bariatric surgery significantly reduced the incidence of hypertriglyceridemia (defined as ≥150 mg/dL) and the incidence of low HDL-C (defined as <39 mg/dL) but no significant reduction in hypercholesterolemia (defined as ≥200 mg/dL).[8]
Primary Prevention
Secondary Prevention
- Lifestyle interventions are a key to efforts to reduce triglycerides that includes[6]
- weight loss if overweight or obese
- physical activity (≥ 150 minutes per week of moderate or higher intensity activity)
- Restriction of alcohol
- Restriction of sugar/refined carbohydrate intakes
- For patients with very high TG level (≥500 mg/dL),chylomicronemia will generally be present. For such patients, a low-fat diet (,15% of energy) may be helpful to reduce entry of new chylomicron particles into the circulation.[6]
- For patients with triglycerides <500 mg/dL, partial replacement of dietary carbohydrate (especially sugars and other refined carbohydrates) with a combination of unsaturated fats and proteins may help to reduce the triglyceride and non-HDL-C concentrations.
References
[9] [10] [11] [3] [12] [13] [14] [13] [15] [16] [[[17]]] [18]
- ↑ Culliton BJ (1987) Fredrickson's bitter end at Hughes. Science 236 (4807):1417-8. PMID: 3296193
- ↑ National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002). "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report". Circulation. 106 (25): 3143–421. PMID 12485966.
- ↑ 3.0 3.1 3.2 3.3 3.4 Gotoda T, Shirai K, Ohta T, Kobayashi J, Yokoyama S, Oikawa S et al. (2012) Diagnosis and management of type I and type V hyperlipoproteinemia. J Atheroscler Thromb 19 (1):1-12. PMID: 22129523
- ↑ Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH et al. (2014) National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 - executive summary. J Clin Lipidol 8 (5):473-88. DOI:10.1016/j.jacl.2014.07.007 PMID: 25234560
- ↑ Greenberg BH, Blackwelder WC, Levy RI (1977) Primary type V hyperlipoproteinemia. A descriptive study in 32 families. Ann Intern Med 87 (5):526-34. PMID: 200162
- ↑ 6.0 6.1 6.2 6.3 Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH et al. (2015) National lipid association recommendations for patient-centered management of dyslipidemia: part 1--full report. J Clin Lipidol 9 (2):129-69. DOI:10.1016/j.jacl.2015.02.003 PMID: 25911072
- ↑ 7.0 7.1 Bays HE, Jones PH, Orringer CE, Brown WV, Jacobson TA (2016) National Lipid Association Annual Summary of Clinical Lipidology 2016. J Clin Lipidol 10 (1 Suppl):S1-43. DOI:10.1016/j.jacl.2015.08.002 PMID: 26891998
- ↑ Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H et al. (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357 (8):741-52. DOI:10.1056/NEJMoa066254 PMID: 17715408
- ↑ Park JR, Jung TS, Jung JH, Lee GW, Kim MA, Park KJ et al. (2005) A case of hypothyroidism and type 2 diabetes associated with type V hyperlipoproteinemia and eruptive xanthomas. J Korean Med Sci 20 (3):502-5. DOI:10.3346/jkms.2005.20.3.502 PMID: 15953878
- ↑ Nagasaka H, Kikuta H, Chiba H, Murano T, Harashima H, Ohtake A et al. (2003) Two cases with transient lipoprotein lipase (LPL) activity impairment: evidence for the possible involvement of an LPL inhibitor. Eur J Pediatr 162 (3):132-8. DOI:10.1007/s00431-002-1133-3 PMID: 12655414
- ↑ Calandra S, Priore Oliva C, Tarugi P, Bertolini S (2006) APOA5 and triglyceride metabolism, lesson from human APOA5 deficiency. Curr Opin Lipidol 17 (2):122-7. DOI:10.1097/01.mol.0000217892.00618.54 PMID: 16531747
- ↑ Marçais C, Verges B, Charrière S, Pruneta V, Merlin M, Billon S et al. (2005) Apoa5 Q139X truncation predisposes to late-onset hyperchylomicronemia due to lipoprotein lipase impairment. J Clin Invest 115 (10):2862-9. DOI:10.1172/JCI24471 PMID: 16200213
- ↑ 13.0 13.1 Ghiselli G, Schaefer EJ, Zech LA, Gregg RE, Brewer HB (1982) Increased prevalence of apolipoprotein E4 in type V hyperlipoproteinemia. J Clin Invest 70 (2):474-7. PMID: 7096573
- ↑ Dallongeville J (2000) Apolipoprotein E mutations, type V hyperlipoproteinaemia and diet. Br J Nutr 83 (6):573-4. PMID: 10911764
- ↑ Piolot A, Nadler F, Cavallero E, Coquard JL, Jacotot B (1996) Prevention of recurrent acute pancreatitis in patients with severe hypertriglyceridemia: value of regular plasmapheresis. Pancreas 13 (1):96-9. PMID: 8783340
- ↑ Titanji R, Paz-Guevara A (1992) Hypertriglyceridemia: severe type V hyperlipidemia in a young woman. Md Med J 41 (3):231-3. PMID: 1602929
- ↑ Stuyt PM, Stalenhoef AF, Demacker PN, van't Laar A (1982) Hyperlipoproteinemia type V and apolipoprotein E4. Lancet 2 (8304):934. PMID: 6126778
- ↑ Fallat RW, Glueck CJ (1976) Familial and acquired type V hyperlipoproteinemia. Atherosclerosis 23 (1):41-62. PMID: 1078394