Glaucoma: Difference between revisions
No edit summary |
|||
| Line 16: | Line 16: | ||
{{Glaucoma}} | {{Glaucoma}} | ||
{{CMG}} | {{CMG}} | ||
==Origin of the word "glaucoma" and history of its discovery== | ==Origin of the word "glaucoma" and history of its discovery== | ||
Revision as of 21:05, 22 August 2012
For patient information click here
| Glaucoma | |
 | |
|---|---|
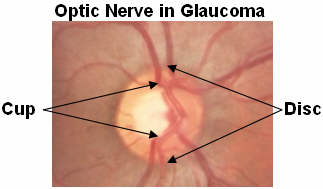
| The pink rim of disc contains nerve fibers. The white cup is a pit with no nerve fibers. As glaucoma advances, the cup enlarges until it occupies most of the disc area. Courtesy AgingEye Times | |
| ICD-10 | H40-H42 |
| ICD-9 | 365 |
| DiseasesDB | 5226 |
| MeSH | D005901 |
|
Glaucoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glaucoma On the Web |
|
American Roentgen Ray Society Images of Glaucoma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]
Origin of the word "glaucoma" and history of its discovery
In the Hippocratic Aphorisms the term glaucoma was used to describe blindness in the elderly with a glazed appearance of the pupil. The implied meaning is that of a clouded or blue-green hue of the cornea in end stage forms that may result in corneal edema and/or coinciding cataract. The Hippocratic writings make no clear distinction between cataract and glaucoma. Both Classical and Alexandrian Greeks did not recognize the specific disease which we now call glaucoma. Homer's glauk-opis Athene could be a "bright-eyed" or a "greyeyed" goddess. Gk. for "owl" was glauk- from its bright, staring eyes.
The definition of glaucoma has changed drastically since its introduction around the time of Hippocrates in approximately 400 BC. The first recognition of a disease associated with a rise in intraocular pressure and thus corresponding to what is now known as glaucoma occurred in the Arabian writings, “Book of Hippocratic treatment”, of At-Tabari (10th century). In European writings, it was Richard Bannister (1622), an English oculist and author of the first book of ophthalmology in English, who recognized glaucoma as a disease with four features: increased intraocular pressure, long duration of the disease, the absence of perception of light and the presence of a fixed pupil. However, throughout the 18th century the term glaucoma was still merely a label applied to an inflamed eye wherein the pupil appeared greenish-blue and the visual prognosis was bad, but the tension of the eye was not stressed.
It was only after the careful description by Antoine-Pierre Demours (1818) that the central concept of a rise in intraocular pressure became fully established. G.J. Guthrie (1823) and William McKenzie, a Scottish clinician (1835) confirmed these findings. Donders (1862) described an incapacitating increased eye tension occurring without any inflammatory symptoms as "simple glaucoma". In 1973 Drance provided for the first time the definition of glaucoma as an optic neuropathy caused by increased intraocular pressure and other associated risk factors.
Classification of glaucoma
Glaucoma has been classified into specific types:[1]
Primary glaucoma and its variants (H40.1-H40.2)
- Primary glaucoma
- Primary open-angle glaucoma, also known as chronic open-angle glaucoma, chronic simple glaucoma, glaucoma simplex
- Low-tension glaucoma
- Primary angle-closure glaucoma, also known as primary closed-angle glaucoma, narrow-angle glaucoma, iris-block glaucoma, acute congestive glaucoma
- Variants of primary glaucoma
- Pigmentary glaucoma
- Exfoliation glaucoma, also known as pseudoexfoliative glaucoma or glaucoma capsulare
Developmental glaucoma (Q15.0)
- Developmental glaucoma
- Primary congenital glaucoma
- Infantile glaucoma
- Glaucoma associated with hereditary of familial diseases
Secondary glaucoma (H40.3-H40.6)
- Secondary glaucoma
- Inflammatory glaucoma
- Uveitis of all types
- Fuchs heterochromic iridocyclitis
- Phacogenic glaucoma
- Angle-closure glaucoma with mature cataract
- Phacoanaphylactic glaucoma secondary to rupture of lens capsule
- Phacolytic glaucoma due to phacotoxic meshwork blockage
- Subluxation of lens
- Glaucoma secondary to intraocular hemorrhage
- Hyphema
- Hemolytic glaucoma, also known as erythroclastic glaucoma
- Traumatic glaucoma
- Angle recession glaucoma: Traumatic recession on anterior chamber angle
- Postsurgical glaucoma
- Aphakic pupillary block
- Ciliary block glaucoma
- Neovascular glaucoma
- Drug-induced glaucoma
- Corticosteroid induced glaucoma
- Alpha-chymotrypsin glaucoma. Postoperative ocular hypertension from use of alpha chymotrypsin.
- Glaucoma of miscellaneous origin
- Associated with intraocular tumors
- Associated with retinal deatchments
- Secondary to severe chemical burns of the eye
- Associated with essential iris atrophy
Absolute glaucoma (H44.5)
- Absolute glaucoma
Risk factors
People with a family history of glaucoma have about a six percent chance of developing glaucoma. Diabetics and African Americans are three times more likely than caucasians to develop primary open angle glaucoma. Asians are susceptible to angle-closure glaucoma, and Inuit have a twenty to forty times higher risk than caucasians of developing primary angle closure glaucoma. Women are three times more likely than men to develop acute angle-closure glaucoma due to their shallower anterior chambers. Use of steroids can also cause glaucoma.
There is increasing evidence of ocular blood flow to be involved in the pathogenesis of glaucoma. Current data indicate that fluctuations in blood flow are more harmful in glaucomatous optic neuropathy than steady reductions. Unstable blood pressure and dips are linked to optic nerve head damage and correlate with visual field deterioration.
A number of studies also suggest that there is a correlation, not necessarily causal, between glaucoma and systemic hypertension (i.e. high blood pressure). In normal tension glaucoma, nocturnal hypotension may play a significant role. On the other hand there is no clear evidence that vitamin deficiencies cause glaucoma in humans, nor that oral vitamin supplementation is useful in glaucoma treatment (Surv Ophthalmol 46:43-55, 2001).
Those at risk for glaucoma are advised to have a dilated eye examination at least once a year.[2]
Diagnosis
Physical Examination
Skin
There may be a grey discoloration of the nail beds.
Eyes
-
0.5 to 0.9 cup-to-disk ratio. Increase seen with open angle glaucoma.[3]
-
Glaucoma[4]
-
A normal range of vision. Courtesy NIH National Eye Institute
-
The same view with advanced vision loss from glaucoma.
Screening for glaucoma is usually performed as part of a comprehensive eye examination performed by ophthalmologists and optometrists. Assessment for glaucoma consists of two branches of tests: structural and functional. Structural analysis investigates glaucomatous changes in the eye's anatomical and physiological properties, whereas functional analysis involves psychometric testing to evaluate how glaucomatous disease has affected the eye's ability to function normally. Specific examples are as follows:
Structural tests
- Tonometry: measuring the intraocular pressure and comparing with both population norms and with subsequent measurements over time. The Goldmann Applanation Tonometer[5] is one example.
- Fundoscopy: stereoscopically viewing the optic nerve head and the retina, looking for characteristic glaucomatous signs and for changes in appearance over time. One important observation is the optic nerve's "cup-disc ratio". Fundus photos (stereoscopic or mono) may be taken to aid the clinician. The 3Dx Digital[6] stereoscopic camera is one example.
- Pachymetry: using a variety of modalities to measure the thickness of the cornea, as a thin cornea is a risk factor for glaucoma.[7][8][9] Corneal pachymetry can also be used to calibrate the measured intraocular pressure for the patient's corneal thickness, as a thicker cornea tends to yield higher intraocular pressure readings.[10][11] The Tomey SP3000 [12] is one example.
- Scanning laser ophthalmoscopy: using a scanning laser to quantify the appearance of the optic nerve head. The Heidelberg Retinal Tomographer (HRT) [13] is one example.
- Scanning laser polarimetry: using polarised light to measure the thickness of the retinal nerve fiber layer. The GDx-VCC [14] is one example.
- Optical coherence tomography: using interferometry to obtain cross-sectional views of the retina and optic nerve head and to measure the thickness of the retinal nerve fiber layer. The Stratus OCT [15] is one example.
For the latter three the quantified results are then statistically compared to age-matched population norms, and to subsequent scans of the same patient over time.
Functional tests
- Automated perimetry: Each area in the patient's visual field is psychometrically tested to see how bright a given spot in that field must be for the patient to detect it. Thus a map can be made of the patient's sensitivity over their visual field and statistically compared to age-matched population norms and to subsequent tests of the same patient over time. Obviously the reliance on patients' response and attention is a factor in itself, one disadvantage of such subjective testing. The Medmont M700[16] is an example of standard automated perimetry, using a white spot over a white background. Newer instruments such as the Humphrey Matrix FDT[17] use frequency-doubling technology to assess the function of a smaller subset of retinal cells, revealing glaucomatous visual field damage somewhat earlier than with standard perimetry.[18][19][20][21][22]
- Visually-evoked potential: to analyse the electrical activity of the visual cortex, assessing the function of the visual system "upstream" from the measured areas on the visual cortex. This has the advantage of assessing visual function without relying on subjective patient input. The EPIC-4000[23]is one example.
Treatment
Although intraocular pressure is only one major risk factors of glaucoma, lowering it via pharmaceuticals or surgery is currently the mainstay of glaucoma treatment. In Europe, Japan, and Canada laser treatment is often the first line of therapy. In the U.S., adoption of early laser has lagged, even though prospective, multi-centered, peer-reviewed studies, since the early '90s, have shown laser to be at least as effective as topical medications in controlling intraocular pressure and preserving visual field. Some studies suggest that acupuncture can be very helpful in the treatment of Glaucoma. [24] [25]
Drugs
Intraocular pressure can be lowered with medication, usually eye drops. There are several different classes of medications to treat glaucoma with several different medications in each class.
Each of these medicines may have local and systemic side effects. Adherence to medication protocol can be confusing and expensive; if side effects occur, the patient must be willing either to tolerate these, or to communicate with the treating physician to improve the drug regimen.
Poor compliance with medications and follow-up visits is a major reason for vision loss in glaucoma patients. Patient education and communication must be ongoing to sustain successful treatment plans for this lifelong disease with no early symptoms. Ophthalmologists have debated whether glaucoma eye drops should initially be started in both eyes or in just one eye (a binocular or monocular trial), but it appears either strategy is reasonable when properly interpreted. [26]
The possible neuroprotective effects of various topical and systemic medications are also being investigated.
Commonly used medications
- Prostaglandin analogs like latanoprost (Xalatan), bimatoprost (Lumigan) and travoprost (Travatan) increase uveoscleral outflow of aqueous humor.
- Topical beta-adrenergic receptor antagonists such as timolol, levobunolol (Betagan), and betaxolol decrease aqueous humor production by the ciliary body.
- Alpha2-adrenergic agonists such as brimonidine (Alphagan) work by a dual mechanism, decreasing aqueous production and increasing uveo-scleral outflow.
- Less-selective sympathomimetics like epinephrine and dipivefrin (Propine) increase outflow of aqueous humor through trabecular meshwork and possibly through uveoscleral outflow pathway, probably by a beta2-agonist action. A two percent epinephine solution may be used topically to reduce IOP in open-angle glaucoma by reducing the production of aqueous humor by vasoconstriction of the ciliary body blood vessels.
- Miotic agents (parasympathomimetics) like pilocarpine work by contraction of the ciliary muscle, tightening the trabecular meshwork and allowing increased outflow of the aqueous humour.
- Carbonic anhydrase inhibitors like dorzolamide (Trusopt), brinzolamide (Azopt), acetazolamide (Diamox) lower secretion of aqueous humor by inhibiting carbonic anhydrase in the ciliary body.
Cannabis
Studies in the 1970s showed that marijuana, when smoked, lowers intraocular pressure.[27] In an effort to determine whether marijuana, or drugs derived from marijuana, might be effective as a glaucoma treatment, the US National Eye Institute supported research studies from 1978 to 1984. These studies demonstrated that some derivatives of marijuana lowered intraocular pressure when administered orally, intravenously, or by smoking, but not when topically applied to the eye. Many of these studies demonstrated that marijuana — or any of its components — could safely and effectively lower intraocular pressure more than a variety of drugs then on the market. In 2003, the American Academy of Ophthalmology released a position statement asserting that "no scientific evidence has been found that demonstrates increased benefits and/or diminished risks of marijuana use to treat glaucoma compared with the wide variety of pharmaceutical agents now available."[27]
The first patient in the United States federal government's Compassionate Investigational New Drug program, Robert Randall, was afflicted with glaucoma and had successfully fought charges of marijuana cultivation because it was deemed a medical necessity (U.S. v. Randall) in 1976.[28]
Surgery
Surgery is the primary therapy for those with congenital glaucoma.[29] Both laser and conventional surgeries are performed. Generally, these operations are a temporary solution, as there is no cure for glaucoma as of yet.
Canaloplasty
Canaloplasty is an advanced, nonpenetrating procedure designed to enhance and restore the eye’s natural drainage system to provide sustained reduction of IOP. Canaloplasty utilizes breakthrough microcatheter technology in a simple and minimally invasive procedure. To perform a canaloplasty, a doctor will create a tiny incision to gain access to a canal in the eye. A microcatheter will circumnavigate the canal around the iris, enlarging the main drainage channel and its smaller collector channels through the injection of a sterile, gel-like material called viscoelastic. The catheter is then removed and a suture is placed within the canal and tightened. By opening the canal, the pressure inside the eye will be relieved.
Laser surgery
Laser trabeculoplasty may be used to treat open angle glaucoma. It is a temporary solution, not a cure. A 50 μm argon laser spot is aimed at the trabecular meshwork to stimulate opening of the mesh to allow more outflow of aqueous fluid. Usually, half of the angle is treated at a time. Traditional laser trabeculoplasty utilizes a thermal argon laser. The procedure is called argon laser trabeculoplasty or ALT. A newer type of laser trabeculoplasty uses a "cold" (non-thermal) laser to stimulate drainage in the trabecular meshwork. This newer procedure is call selective laser trabeculoplasty or SLT. Studies show that SLT is as effective as ALT at lowering eye pressure. In addition, SLT may be repeated three to four times, whereas ALT can usually be repeated only once.
Laser peripheral iridotomy may be used in patients susceptible to or affected by angle closure glaucoma. During laser iridotomy, laser energy is used to make a small full-thickness opening in the iris. This opening equalizes the pressure between the front and back of the iris, causing the iris to move backward. This uncovers the trabecular meshwork. In some cases of intermittent or short-term angle closure this may lower the eye pressure. Laser iridotomy reduces the risk of developing an attack of acute angle closure. In most cases it also reduces the risk of developing chronic angle closure or gradual adhesion of the iris to the trabecular meshwork.
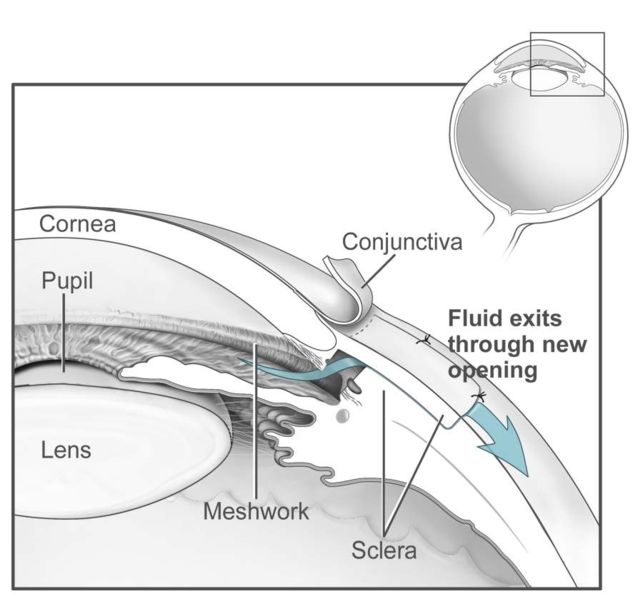
Trabeculectomy
The most common conventional surgery performed for glaucoma is the trabeculectomy. Here, a partial thickness flap is made in the scleral wall of the eye, and a window opening made under the flap to remove a portion of the trabecular meshwork. The scleral flap is then sutured loosely back in place. This allows fluid to flow out of the eye through this opening, resulting in lowered intraocular pressure and the formation of a bleb or fluid bubble on the surface of the eye. Scarring can occur around or over the flap opening, causing it to become less effective or lose effectiveness altogether. One person can have multiple surgical procedures of the same or different types.
Glaucoma drainage implants
There are also several different glaucoma drainage implants. These include the original Molteno implant (1966), the Baerveldt tube shunt, or the valved implants, such as the Ahmed glaucoma valve implant and the later generation pressure ridge Molteno implants. These are indicated for glaucoma patients not responding to maximal medical therapy, with previous failed guarded filtering surgery (trabeculectomy). The flow tube is inserted into the anterior chamber of the eye and the plate is implanted underneath the conjunctiva to allow flow of aqueous fluid out of the eye into a chamber called a bleb. The Express mini-implant is currently being used as a modification of the standard trabeculectomy technique, and is a non-valved conduit between the anterior chamber and the space under the scleral flap[30].
- The first-generation Molteno and other non-valved implants sometimes require the ligation of the tube until the bleb formed is mildly fibrosed and water-tight[31]This is done to reduce postoperative hypotony -- sudden drops in postoperative intraocular pressure (IOP).
- Valved implants such as the Ahmed glaucoma valve attempt to control postoperative hypotony by using a mechanical valve. Studies show that in severe cases of glaucoma, double plate Molteno implants are associated with lower mean IOP in the long term compared to the Ahmed glaucoma valve [32]
- Second and third generation Molteno implants incorporate a biological valve and studies show considerable improvement in postoperative outcome over the older style Ahmed and Molteno implants.
The ongoing scarring over the conjunctival dissipation segment of the shunt may become too thick for the aqueous humor to filter through. This may require preventive measures using anti-fibrotic medication like 5-fluorouracil (5-FU) or mitomycin-C (during the procedure), or additional surgery.
Major studies
- Advanced Glaucoma Intervention Study (AGIS) - large American National Eye Institute (NEI) sponsored study designed "to assess the long-range outcomes of sequences of interventions involving trabeculectomy and argon laser trabeculoplasty in eyes that have failed initial medical treatment for glaucoma." It recommends different treatments based on race.
- Early Manifest Glaucoma Trial (EMGT) -Another NEI study found that immediately treating people who have early stage glaucoma can delay progression of the disease.
- Ocular Hypertension Treatment Study (OHTS) -NEI study findings: "...Topical ocular hypotensive medication was effective in delaying or preventing onset of Primary Open Angle Glaucoma (POAG) in individuals with elevated Intraocular Pressure (IOP). Although this does not imply that all patients with borderline or elevated IOP should receive medication, clinicians should consider initiating treatment for individuals with ocular hypertension who are at moderate or high risk for developing POAG."
- Blue Mountains Eye Study "The Blue Mountains Eye Study was the first large population-based assessment of visual impairment and common eye diseases of a representative older Australian community sample." Risk factors for glaucoma and other eye disease were determined.
See also
- List of eye diseases and disorders
- Ocular hypertension
- Glaucoma valves
- Mansour F. Armaly
- Laszlo Z. Bito
- Charles D. Phelps
- American Glaucoma Society
References
- ↑ Paton D, Craig JA. "Glaucomas. Diagnosis and management." Clin Symp. 1976;28(2):1-47. PMID 1053095.
- ↑ National Institutes of Health
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/
- ↑ Haag-Streit Tonometers: Goldmann Tonometer
- ↑ Nidek Technology America, Inc., Greensboro NC, USA Nidek "3Dx Digital" Stereo Fundus Camera
- ↑ Herndon L, Weizer J, Stinnett S (2004) Central Corneal Thickness as a Risk Factor for Advanced Glaucoma Damage. Arch Ophthalmol 122(1):17-21
- ↑ Jonas J, Stroux A, Velten I, Juenemann A, Martus P, Budde W (2005) Central Corneal Thickness Correlated with Glaucoma Damage and Rate of Progression. Investigative Ophthalmology and Visual Science. 46:1269-1274
- ↑ Medeiros F, Sample P, Zangwill L, Bowd C, Aihara M, Weinreb R (2003) Corneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous optic neuropathy. American Journal of Ophthalmology 136(5):805-813
- ↑ Doughty M, Zaman M (2000) Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol 44(5):367-408
- ↑ Shah S, Chatterjee A, Mathai M, Kelly S, Kwartz J, Henson D, McLeod D (1999) Relationship between corneal thickness and measured intraocular pressure in a general ophthalmology clinic. Ophthalmology 106(11):2154-60
- ↑ CBD Ophthalmic/Tomey, Arizona USA SP3000
- ↑ Heidelberg Engineering GmbH, Dossenheim, Germany Heidelberg Engineering: HRT3 Glaucoma
- ↑ Laser Diagnostic Technologies, Inc., San Diego, CA Carl Zeiss Meditec: GDx
- ↑ Humphrey Instruments, Dublin, CA Carl Zeiss Meditec: Stratus OCT
- ↑ Medmont International, Pty Ltd, Victoria, Australia M700 Overview
- ↑ Welch Allyn Inc, New York, USA. Welch Allyn Site Map, Carl Zeiss Meditec Carl Zeiss launches new Humphrey Matrix
- ↑ Ferreras A, Polo V, Larrosa J, Pablo L, Pajarin A, Pueyo V, Honrubia F (2007) Can frequency-doubling technology and short-wavelength automated perimetries detect visual field defects before standard automated perimetry in patients with preperimetric glaucoma? J Glaucoma 16(4):372-83
- ↑ Wadood A, Azuara-Blanco A, Aspinall P, Taguri A, King A (2002) Sensitivity and specificity of frequency-doubling technology, tendency-oriented perimetry, and Humphrey Swedish interactive threshold algorithm-fast perimetry in a glaucoma practice. Am J Ophthalmol 133(3):327-32
- ↑ Kalaboukhova L, Lindblom B (2003) Frequency doubling technology and high-pass resolution perimetry in glaucoma and ocular hypertension. Acta Ophthalmol Scand 81(3):247-52
- ↑ Akiko N, Kyoko M, Mikio N, Naoyuki T, Tomoko U, Hiroshi O, Kiichiro Y (2004) Ability of Frequency Doubling Technology to Detect Early Glaucomatous Visual Field Changes. Folia Ophthalmologica Japonica 55(1):22-26
- ↑ Cello K, Nelson-Quigg J, Johnson C (2000) Frequency doubling technology perimetry for detection of glaucomatous visual field loss. Am J Ophthalmol 129(3):314-22
- ↑ LPC Technologies Inc, Gaithursburg, MD EPIC-4000 EPIC-4000 Stand-alone Visual Electrodiagnostic Testing System
- ↑ Clinical application of acupuncture in ophthalmology. Dabov S; Goutoranov G; Ivanova R; Petkova N Acupunct Electrother Res 1985, 10 (1-2) p79-93
- ↑ New Peer Reviewed Study treating open angle glaucoma with acupuncture, [1]
- ↑ Interpretation of uniocular and binocular trials of glaucoma medications: an observational case series, [2]
- ↑ 27.0 27.1 American Academy of Ophthalmology. Complementary Therapy Assessment: Marijuana in the Treatment of Glaucoma. Retrieved August 2, 2006.
- ↑ http://blogs.salon.com/0002762/stories/2005/02/18/irvRosenbergAndTheCompassi.html
- ↑ "Glaucoma, Congenital: GLC3 Buphthalmos." OMIM - Online Mendelian Inheritance in Man. Accessed October 17, 2006.
- ↑ Maris PJ, Jr., Ishida K, Netland PA. Comparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under scleral flap. J Glaucoma 2007 January;16(1):14-9
- ↑ Molteno AC, Polkinghorne PJ, Bowbyes JA. The vicryl tie technique for inserting a draining implant in the treatment of secondary glaucoma. Aust N Z J Ophthalmol. 1986 Nov;14(4):343-54 [3]
- ↑ Ayyala RS, Zurakowski D et al. Comparison of double-plate Molteno and Ahmed glaucoma valve in patients with advanced uncontrolled glaucoma. Ophthalmic Surg Lasers. 2002 Mar-Apr;33(2):94-101.[4].
External links
- International Glaucoma Association A charity for people with glaucoma.
- Glaucoma Resource Guide from the National Eye Institute (NEI).
- Global Association of International Glaucoma Societies - featuring a hymn about the successful treatment of glaucoma
- Glaucoma Research Foundation
- "Glaucoma - What is Glaucoma?". NLM. Retrieved 2007-04-21. video
- Nonprofit Foundation for Glaucoma
- National Glaucoma Research
- DJO | Digital Journal of Ophthalmology
- Lions Eye Institute, Perth, Australia
- Improving Glaucoma Naturally
ca:Glaucoma da:Grøn stær de:Glaukom eo:Glaŭkomo hr:Glaukom it:Glaucoma (medicina) he:גלאוקומה ms:Glaukoma nl:Glaucoom no:Glaukom sr:Глауком fi:Glaukooma sv:Glaukom
![0.5 to 0.9 cup-to-disk ratio. Increase seen with open angle glaucoma.[3]](/images/f/f0/Cup-to-disk_ratio.jpg)
![Glaucoma[4]](/images/d/db/Glaucoma.jpg)

