Esophageal cancer pathophysiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
==Pathophysiology== | ==Pathophysiology== | ||
The [[esophagus]] is lined by nonkeratinized stratified [[Squamous epithelium|squamous]] [[epithelium]]. This lining is maintained as long as there are no stressors leading to a [[Metaplasia|metaplastic]] change. | *The [[esophagus]] is lined by nonkeratinized stratified [[Squamous epithelium|squamous]] [[epithelium]]. | ||
*This lining is maintained as long as there are no stressors leading to a [[Metaplasia|metaplastic]] change. | |||
===Esophageal Squamous Cell Carcinoma=== | |||
*The risk factors for esophageal squamous cell carcinoma include smoking and alcohol.<ref name="pmid24834141">{{cite journal |vauthors=Napier KJ, Scheerer M, Misra S |title=Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities |journal=World J Gastrointest Oncol |volume=6 |issue=5 |pages=112–20 |year=2014 |pmid=24834141 |pmc=4021327 |doi=10.4251/wjgo.v6.i5.112 |url=}}</ref><ref name="pmid22320939">{{cite journal |vauthors=Mao WM, Zheng WH, Ling ZQ |title=Epidemiologic risk factors for esophageal cancer development |journal=Asian Pac. J. Cancer Prev. |volume=12 |issue=10 |pages=2461–6 |year=2011 |pmid=22320939 |doi= |url=}}</ref> | |||
*Alcohol is able to dissolve fat soluble compounds. | |||
*When alcohol and tabacco are combined they have a synergistic effect and the risk for squamous cell esophageal cancer is higher. | |||
*Tabacco carcinogens such as aromatic amines, nitrosamines and polycyclic hydrocarbons are, therefore, able to penetrate the esophageal epithelium deeper when in the presence of alcohol. | |||
*Alcohol is also able to decrease the metabolic activities of epithelial cells by damaging DNA. | |||
*When the cellular DNA is damaged, the cell can not undergo detoxification and cannot protect itself from oxidative damage. | |||
*Oxidation leads to inflammation of the squamous epithelium. | |||
*Continuous irritation of the epithelium leads to dysplasia and in situ malignant transformation. | |||
===Esophageal Adenocarcinoma=== | |||
*The risk factors of adenocarcinoma of the esophagus include gastroesophageal reflux disease and obesity.<ref name="pmid8578231">{{cite journal |vauthors=Tilanus HW |title=Changing patterns in the treatment of carcinoma of the esophagus |journal=Scand. J. Gastroenterol. Suppl. |volume=212 |issue= |pages=38–42 |year=1995 |pmid=8578231 |doi= |url=}}</ref><ref name="pmid10233832">{{cite journal |vauthors=Jankowski JA, Wright NA, Meltzer SJ, Triadafilopoulos G, Geboes K, Casson AG, Kerr D, Young LS |title=Molecular evolution of the metaplasia-dysplasia-adenocarcinoma sequence in the esophagus |journal=Am. J. Pathol. |volume=154 |issue=4 |pages=965–73 |year=1999 |pmid=10233832 |pmc=1866556 |doi=10.1016/S0002-9440(10)65346-1 |url=}}</ref><ref name="pmid16299787">{{cite journal |vauthors=Koppert LB, Wijnhoven BP, van Dekken H, Tilanus HW, Dinjens WN |title=The molecular biology of esophageal adenocarcinoma |journal=J Surg Oncol |volume=92 |issue=3 |pages=169–90 |year=2005 |pmid=16299787 |doi=10.1002/jso.20359 |url=}}</ref><ref name="pmid8998117">{{cite journal |vauthors=Ireland AP, Clark GW, DeMeester TR |title=Barrett's esophagus. The significance of p53 in clinical practice |journal=Ann. Surg. |volume=225 |issue=1 |pages=17–30 |year=1997 |pmid=8998117 |pmc=1190601 |doi= |url=}}</ref><ref name="pmid23500888">{{cite journal |vauthors=Nieman KM, Romero IL, Van Houten B, Lengyel E |title=Adipose tissue and adipocytes support tumorigenesis and metastasis |journal=Biochim. Biophys. Acta |volume=1831 |issue=10 |pages=1533–41 |year=2013 |pmid=23500888 |pmc=3742583 |doi=10.1016/j.bbalip.2013.02.010 |url=}}</ref> | |||
*The chronic reflux of gastric acid and bile at the gastroesophageal junction leads to the irritation of squamous epithelium lining the esophagus. | |||
*Chronic irritation leads to metaplasia of esophagus. | |||
*The lining of the esophagus changes from non-keratinized stratified [[Squamous epithelium|squamous]] [[epithelium]] to columnar epithelium. | |||
*This condition is called Barrett's esophagus. | |||
*The progression of Barrett metaplasia to adenocarcinoma is associated with several changes in gene structure, gene expression, and protein structure. | |||
*Mutations in PT53 genes and P16 genes along with cell cycle abnormalities and aneuploidy have all been associated with esophageal adenocarcinoma. | |||
*In addition, obesity is implicated in the development of esophageal adenocarcinoma. | |||
*Patients with central obesity tend to have hypertrophied adipocytes and inflammatory cells within their fat deposits. | |||
*This creates a microenvironment within the adipocyte that promotes tumor development through the release of adipokines and cytokines. | |||
*Adipocytes are also able to provide energy to support the tumor's growth. | |||
==Pathology== | ==Pathology== | ||
Revision as of 19:22, 20 December 2017
|
Esophageal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Esophageal cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Esophageal cancer pathophysiology |
|
Risk calculators and risk factors for Esophageal cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Hadeel Maksoud M.D.[2]
Overview
The pathophysiology of esophageal cancer depends on the histological subtype, whether squamous cell carcinoma or adenocarcinoma.
Pathophysiology
- The esophagus is lined by nonkeratinized stratified squamous epithelium.
- This lining is maintained as long as there are no stressors leading to a metaplastic change.
Esophageal Squamous Cell Carcinoma
- The risk factors for esophageal squamous cell carcinoma include smoking and alcohol.[1][2]
- Alcohol is able to dissolve fat soluble compounds.
- When alcohol and tabacco are combined they have a synergistic effect and the risk for squamous cell esophageal cancer is higher.
- Tabacco carcinogens such as aromatic amines, nitrosamines and polycyclic hydrocarbons are, therefore, able to penetrate the esophageal epithelium deeper when in the presence of alcohol.
- Alcohol is also able to decrease the metabolic activities of epithelial cells by damaging DNA.
- When the cellular DNA is damaged, the cell can not undergo detoxification and cannot protect itself from oxidative damage.
- Oxidation leads to inflammation of the squamous epithelium.
- Continuous irritation of the epithelium leads to dysplasia and in situ malignant transformation.
Esophageal Adenocarcinoma
- The risk factors of adenocarcinoma of the esophagus include gastroesophageal reflux disease and obesity.[3][4][5][6][7]
- The chronic reflux of gastric acid and bile at the gastroesophageal junction leads to the irritation of squamous epithelium lining the esophagus.
- Chronic irritation leads to metaplasia of esophagus.
- The lining of the esophagus changes from non-keratinized stratified squamous epithelium to columnar epithelium.
- This condition is called Barrett's esophagus.
- The progression of Barrett metaplasia to adenocarcinoma is associated with several changes in gene structure, gene expression, and protein structure.
- Mutations in PT53 genes and P16 genes along with cell cycle abnormalities and aneuploidy have all been associated with esophageal adenocarcinoma.
- In addition, obesity is implicated in the development of esophageal adenocarcinoma.
- Patients with central obesity tend to have hypertrophied adipocytes and inflammatory cells within their fat deposits.
- This creates a microenvironment within the adipocyte that promotes tumor development through the release of adipokines and cytokines.
- Adipocytes are also able to provide energy to support the tumor's growth.
Pathology
Gross pathology
Squamous cell carcinoma or adenocarcinoma of the esophagus may appear as:[8]
- Flat and irregular plaque
- Polypoid lesion
- Ulcerating, fungating mass.
- Location:
- Squamous cell carcinoma is usually found in the mid-third of the esophagus.
- Adenocarcinoma is usually found in the lower third of the esophagus near the gastric opening.
- Location:
Microscopic pathology
Nuclear atypia of malignancy:
- Found in both types:
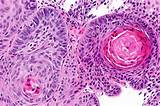
Squamous cell carcinoma:
- Atypical squamous cells invade the basement membrane [9]
- Cytology of squamous cells:
- Eccentric nucleus
- High mitotic activity
- Eosinophilic cytoplasm
- Squamous whorls or keratin pearls
- Cytology of squamous cells:
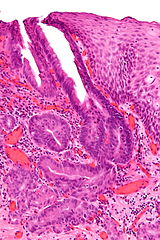
Adenocarcinoma
- Atypical adenomatous cells show:
- Invading cell clusters or glands[10]
- Cribriforming
- Desmoplasia
- Invasion into submucosa
References
- ↑ Napier KJ, Scheerer M, Misra S (2014). "Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities". World J Gastrointest Oncol. 6 (5): 112–20. doi:10.4251/wjgo.v6.i5.112. PMC 4021327. PMID 24834141.
- ↑ Mao WM, Zheng WH, Ling ZQ (2011). "Epidemiologic risk factors for esophageal cancer development". Asian Pac. J. Cancer Prev. 12 (10): 2461–6. PMID 22320939.
- ↑ Tilanus HW (1995). "Changing patterns in the treatment of carcinoma of the esophagus". Scand. J. Gastroenterol. Suppl. 212: 38–42. PMID 8578231.
- ↑ Jankowski JA, Wright NA, Meltzer SJ, Triadafilopoulos G, Geboes K, Casson AG, Kerr D, Young LS (1999). "Molecular evolution of the metaplasia-dysplasia-adenocarcinoma sequence in the esophagus". Am. J. Pathol. 154 (4): 965–73. doi:10.1016/S0002-9440(10)65346-1. PMC 1866556. PMID 10233832.
- ↑ Koppert LB, Wijnhoven BP, van Dekken H, Tilanus HW, Dinjens WN (2005). "The molecular biology of esophageal adenocarcinoma". J Surg Oncol. 92 (3): 169–90. doi:10.1002/jso.20359. PMID 16299787.
- ↑ Ireland AP, Clark GW, DeMeester TR (1997). "Barrett's esophagus. The significance of p53 in clinical practice". Ann. Surg. 225 (1): 17–30. PMC 1190601. PMID 8998117.
- ↑ Nieman KM, Romero IL, Van Houten B, Lengyel E (2013). "Adipose tissue and adipocytes support tumorigenesis and metastasis". Biochim. Biophys. Acta. 1831 (10): 1533–41. doi:10.1016/j.bbalip.2013.02.010. PMC 3742583. PMID 23500888.
- ↑ Sugarbaker, David (2015). Adult chest surgery. New York: McGraw-Hill Education. ISBN 0071781897.
- ↑ "Squamous cell carcinoma of the esophagus".
- ↑ "Esophageal adenocarcinoma".