Desmoid tumor natural history, complications, and prognosis: Difference between revisions
| (33 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Desmoid tumor}} | {{Desmoid tumor}} | ||
{{CMG}} {{AE}}{{Faizan}} | {{CMG}} {{AE}}{{S.M.}}{{Faizan}} | ||
==Overview== | ==Overview== | ||
[[Desmoid tumor|Desmoids]] can develop virtually at any site of [[body]] causing wide range of [[clinical]] [[symptoms]] depending on size and [[tumor]] location or they can cause no [[symptoms]] at all. They may be accidentally picked up on a [[scan]] or a routine [[physical examination]] done for other [[medical]] reasons. They might grow aggressively or slowly or remian stable, hence, exhibiting wide range of behaviors in different individuals. Common [[complications]] of [[desmoid tumor]] include progression to agressive [[fibromatosis]], involvement of intra-abdominal [[viscera]] that may lead to [[rupture]] of [[intestines]], compression of the [[kidneys]] or [[ureters]], [[rectal bleeding]], compression of critical [[blood vessels]] such as the mesenteric [[vessels]] and the [[Vena cavae|vena cava]], [[amputation]] and loss of significant portions of [[foregut]] [[Surgery|post-surgery]]. Five-year progression-free [[survival rate]] is 50% in [[patients]] with a primary or recurrent [[Desmoid tumor|desmoid]] who are not treated initially with [[surgery]], [[Radiotherapy|radiotherapy (RT)]], or [[systemic therapy]]. Massive and [[inoperable]] [[Desmoid tumor|desmoids]] have become an important cause of [[Morbidity & Mortality|morbidity and mortality]] in [[FAP]] [[patients]] [[Colectomy|post-colectomy]]. [[Desmoid tumor]] associated with [[FAP]] has the least favorable [[prognosis]] due to high recurrence rate. Whereas, non-[[FAP]]-associated intra-abdominal [[fibromatosis]] has a low recurrence rate after [[surgical resection]]. | |||
==Natural history== | ==Natural history== | ||
*If left untreated, desmoid tumor produces few symptoms early in the course | *[[Desmoid tumor|Desmoid tumors]] can develop at virtually any site in the [[Human body|body]]. | ||
*They can have a wide range of [[clinical]] [[symptoms]] or no [[symptoms]] at all. | |||
*Many [[Desmoid tumor|desmoid tumors]] are accidentally picked up on a [[scan]] or a routine [[Physical examination|physical exam]] done for other [[medical]] reasons. | |||
*If left untreated, [[desmoid tumor]] produces few [[symptoms]] early in the course | |||
*[[Patients]] are [[asymptomatic]] at the time of [[diagnosis]] | |||
*[[Patients]] can remain [[asymptomatic]] even after many years | |||
*[[Patients]] can have a wide range of [[symptoms]] anytime depending upon the size and location of [[tumor]] | |||
*On some occasions, [[Desmoid tumor|desmoid tumors]] can shrink or become [[quiescent]] (deep [[sleep]]) without any [[therapy]] | |||
*Some [[Desmoid tumor|desmoids]] may be stable or grow very slowly over a period of months and years | |||
*A small subset of [[Desmoid tumor|desmoid tumors]] may be aggressive and grow rapidly | |||
*Hence, [[Desmoid tumor|desmoid tumors]] exhibit wide range of behaviors varying from person to person | |||
==Complications== | ==Complications== | ||
Common complications of desmoid | Common [[complications]] of [[Desmoid tumor|desmoid tumors]] include: | ||
*Progression to aggressive fibromatosis | *Progression to [[aggressive fibromatosis]] | ||
* | *Surgical [[complications]] such as: | ||
*[[ | **[[Amputation]] | ||
**Loss of significant portions of [[foregut]] | |||
*Intra-abdomianl/[[pelvic]] [[Desmoid tumor|desmoids]] can lead to: | |||
**[[Rupture]] of [[intestines]] | |||
**Compression of the [[kidneys]] or [[ureters]] | |||
**[[Rectal bleeding]] | |||
**Compression of critical [[blood vessels]] such as the mesenteric [[vessels]] and the [[vena cava]] | |||
{| | |||
| | |||
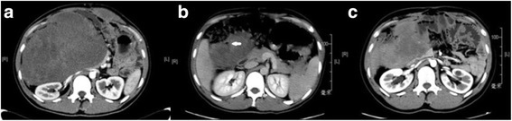
[[File:Desmoid intestine perforation.png|thumb|1200px|none|The progression of the intra-abdominal desmoid in patient 2. a CT scan before DOX/DTIC therapy showing a large mass in the abdomen and a desmoid tumor on the left abdominal wall. b CT scan of the same patient after DOX/DTIC therapy, showing tumor regression and perforation (as indicated by the white arrow, the gas was encapsulated by the tumor). c Follow-up CT scan in December 2015 [https://openi.nlm.nih.gov/detailedresult?img=PMC4932702_12957_2016_935_Fig2_HTML&query=desmoid%20tumor%20CT&it=xg&req=4&npos=2 Source: Li W. et al, Department of Oncology, Zhongshan Hospital, Fudan University, Shanghai, China]]] | |||
|} | |||
==Prognosis== | ==Prognosis== | ||
Desmoid tumor | *Five-year progression-free [[survival rate]] is 50% in [[patients]] with a primary or recurrent [[Desmoid tumor|desmoid]] who are not treated initially with [[surgery]], [[radiotherapy]] (RT), or [[systemic therapy]] | ||
*[[Desmoid tumor|Desmoid tumors]] have become an important cause of [[Morbidity & Mortality|morbidity and mortality]] due to increasing use of [[prophylactic]] [[colectomy]] in [[FAP]] [[patients]]<ref name="pmid9593254">{{cite journal| author=Church JM| title=Mucosal ischemia caused by desmoid tumors in patients with familial adenomatous polyposis: report of four cases. | journal=Dis Colon Rectum | year= 1998 | volume= 41 | issue= 5 | pages= 661-3 | pmid=9593254 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9593254 }} </ref><ref name="pmid9823798">{{cite journal| author=Sagar PM, Möslein G, Dozois RR| title=Management of desmoid tumors in patients after ileal pouch-anal anastomosis for familial adenomatous polyposis. | journal=Dis Colon Rectum | year= 1998 | volume= 41 | issue= 11 | pages= 1350-5; discussion 1355-6 | pmid=9823798 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9823798 }} </ref><ref name="pmid8395084">{{cite journal| author=Penna C, Tiret E, Parc R, Sfairi A, Kartheuser A, Hannoun L et al.| title=Operation and abdominal desmoid tumors in familial adenomatous polyposis. | journal=Surg Gynecol Obstet | year= 1993 | volume= 177 | issue= 3 | pages= 263-8 | pmid=8395084 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8395084 }} </ref><ref name="pmid8529453">{{cite journal| author=Kadmon M, Möslein G, Buhr HJ, Herfarth C| title=[Desmoid tumors in patients with familial adenomatous polyposis (FAP). Clinical and therapeutic observations from the Heidelberg polyposis register]. | journal=Chirurg | year= 1995 | volume= 66 | issue= 10 | pages= 997-1005 | pmid=8529453 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8529453 }} </ref><ref name="pmid2165452">{{cite journal| author=Arvanitis ML, Jagelman DG, Fazio VW, Lavery IC, McGannon E| title=Mortality in patients with familial adenomatous polyposis. | journal=Dis Colon Rectum | year= 1990 | volume= 33 | issue= 8 | pages= 639-42 | pmid=2165452 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2165452 }} </ref><ref name="pmid22323009">{{cite journal| author=Quintini C, Ward G, Shatnawei A, Xhaja X, Hashimoto K, Steiger E et al.| title=Mortality of intra-abdominal desmoid tumors in patients with familial adenomatous polyposis: a single center review of 154 patients. | journal=Ann Surg | year= 2012 | volume= 255 | issue= 3 | pages= 511-6 | pmid=22323009 | doi=10.1097/SLA.0b013e31824682d4 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22323009 }} </ref> | |||
*[[Desmoid tumor|Desmoids]] when become massive and [[inoperable]], can cause death in overall 11% of [[FAP]] patients [[Colectomy|post-colectomy surgery]] | |||
**18-31% [[mortality]] in [[patients]] having [[Desmoid tumor|desmoid]]<nowiki/>s with [[colorectal carcinoma]] | |||
**22% mortality in [[Desmoid tumor|desmoid]] [[patients]] with periampullary [[carcinomas]]<ref name="pmid19069698">{{cite journal| author=Seow-Choen F| title=The management of desmoids in patients with familial adenomatous polyposis (FAP). | journal=Acta Chir Iugosl | year= 2008 | volume= 55 | issue= 3 | pages= 83-7 | pmid=19069698 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19069698 }} </ref> | |||
*Due to gradual progression to [[Desmoid tumor|desmoids]], 60% of [[FAP]] [[patients]] remain alive for 10 years after the [[diagnosis]]<ref name="pmid22323009">{{cite journal| author=Quintini C, Ward G, Shatnawei A, Xhaja X, Hashimoto K, Steiger E et al.| title=Mortality of intra-abdominal desmoid tumors in patients with familial adenomatous polyposis: a single center review of 154 patients. | journal=Ann Surg | year= 2012 | volume= 255 | issue= 3 | pages= 511-6 | pmid=22323009 | doi=10.1097/SLA.0b013e31824682d4 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22323009 }} </ref><ref name="pmid10733118">{{cite journal| author=Soravia C, Berk T, McLeod RS, Cohen Z| title=Desmoid disease in patients with familial adenomatous polyposis. | journal=Dis Colon Rectum | year= 2000 | volume= 43 | issue= 3 | pages= 363-9 | pmid=10733118 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10733118 }} </ref><ref name="pmid9336146">{{cite journal| author=Goy BW, Lee SP, Eilber F, Dorey F, Eckardt J, Fu YS et al.| title=The role of adjuvant radiotherapy in the treatment of resectable desmoid tumors. | journal=Int J Radiat Oncol Biol Phys | year= 1997 | volume= 39 | issue= 3 | pages= 659-65 | pmid=9336146 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9336146 }} </ref><ref name="pmid8946994">{{cite journal| author=Lynch HT, Fitzgibbons R| title=Surgery, desmoid tumors, and familial adenomatous polyposis: case report and literature review. | journal=Am J Gastroenterol | year= 1996 | volume= 91 | issue= 12 | pages= 2598-601 | pmid=8946994 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8946994 }} </ref><ref name="pmid18581438">{{cite journal| author=Lefevre JH, Parc Y, Kernéis S, Goasguen N, Benis M, Parc R et al.| title=Risk factors for development of desmoid tumours in familial adenomatous polyposis. | journal=Br J Surg | year= 2008 | volume= 95 | issue= 9 | pages= 1136-9 | pmid=18581438 | doi=10.1002/bjs.6241 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18581438 }} </ref><ref name="pmid23334997">{{cite journal| author=Schiessling S, Kihm M, Ganschow P, Kadmon G, Büchler MW, Kadmon M| title=Desmoid tumour biology in patients with familial adenomatous polyposis coli. | journal=Br J Surg | year= 2013 | volume= 100 | issue= 5 | pages= 694-703 | pmid=23334997 | doi=10.1002/bjs.9053 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23334997 }} </ref> | |||
*[[Pregnancy]]-associated [[Desmoid tumor|desmoid]] [[fibromatosis]] is associated with overall good [[Outcome|outcomes]] without any attributable [[obstetric]] [[complications]] | |||
*[[FAP]]-associated intra-abdominal [[fibromatosis]] has a high recurrence rate after [[surgical resection]] | |||
*Non-[[FAP]]-associated intra-abdominal [[fibromatosis]] has a low recurrence rate after [[surgical resection]]<ref name="pmid22359346">{{cite journal| author=Wilkinson MJ, Fitzgerald JE, Thomas JM, Hayes AJ, Strauss DC| title=Surgical resection for non-familial adenomatous polyposis-related intra-abdominal fibromatosis. | journal=Br J Surg | year= 2012 | volume= 99 | issue= 5 | pages= 706-13 | pmid=22359346 | doi=10.1002/bjs.8703 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22359346 }} </ref> | |||
===Recurrence of desmoid tumors=== | |||
*[[Recurrence plot|Recurrence]] rate is 20% to 77% depending on the [[Location parameter|location]], [[Extent of reaction|extent]] and [[completeness]] of the initial [[resection]] | |||
*[[Abdominal wall]] [[Desmoid tumor|desmoid tumors]] have a significantly lower recurrence rate of 20% to 30% | |||
*[[Abdominal wall]] [[Desmoid tumor|desmoids]] usually becomes evident within six months after [[excision]] or in connection with subsequent [[Gestation|gestations]] or deliveries | |||
===Prognostic stratification system for FAP-associated desmoids (Cleveland Clinic)=== | |||
*Following [[Prognostic]] stratification [[system]] for [[FAP]]-associated [[Desmoid tumor|desmoids]] was proposed after a study was done in [[Cleveland Clinic]]:<ref name="pmid22323009">{{cite journal| author=Quintini C, Ward G, Shatnawei A, Xhaja X, Hashimoto K, Steiger E et al.| title=Mortality of intra-abdominal desmoid tumors in patients with familial adenomatous polyposis: a single center review of 154 patients. | journal=Ann Surg | year= 2012 | volume= 255 | issue= 3 | pages= 511-6 | pmid=22323009 | doi=10.1097/SLA.0b013e31824682d4 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22323009 }} </ref> | |||
{| class="wikitable" | |||
|+Prognostic stratification system for FAP-associated desmoids (Cleveland Clinic) | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Tumor stage | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Characteristic features | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Five-year survival rate | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |'''Stage I''' | |||
| | |||
* [[Asymptomatic]] | |||
* <10 cm maximum [[diameter]] | |||
* Not growing | |||
|95% | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |'''Stage II''' | |||
| | |||
* Mildly [[symptomatic]] ([[sensation]] of [[mass]] or [[pain]] but no [[restriction]]) | |||
* <10 cm in maximum [[diameter]] | |||
* Not growing | |||
|100% | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |'''Stage III''' | |||
| | |||
* Moderately [[symptomatic]] ([[sensation]] of [[mass]], [[pain]], restrictive but not hospitalized) | |||
* [[Bowel]]/ureteric [[obstruction]] | |||
* 10 to 20 cm in size | |||
* Slowly growing | |||
|89% | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |'''Stage IV''' | |||
| | |||
* Severely [[symptomatic]] ([[sensation]] of [[mass]], [[pain]], restrictive and hospitalized) | |||
* [[Septic]] [[complications]] such as [[fistula]] and [[abscess]] | |||
* >20 cm in size | |||
* Rapidly growing | |||
|76% | |||
|} | |||
==Reference== | ==Reference== | ||
Latest revision as of 14:53, 16 May 2019
|
Desmoid tumor Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]Faizan Sheraz, M.D. [3]
Overview
Desmoids can develop virtually at any site of body causing wide range of clinical symptoms depending on size and tumor location or they can cause no symptoms at all. They may be accidentally picked up on a scan or a routine physical examination done for other medical reasons. They might grow aggressively or slowly or remian stable, hence, exhibiting wide range of behaviors in different individuals. Common complications of desmoid tumor include progression to agressive fibromatosis, involvement of intra-abdominal viscera that may lead to rupture of intestines, compression of the kidneys or ureters, rectal bleeding, compression of critical blood vessels such as the mesenteric vessels and the vena cava, amputation and loss of significant portions of foregut post-surgery. Five-year progression-free survival rate is 50% in patients with a primary or recurrent desmoid who are not treated initially with surgery, radiotherapy (RT), or systemic therapy. Massive and inoperable desmoids have become an important cause of morbidity and mortality in FAP patients post-colectomy. Desmoid tumor associated with FAP has the least favorable prognosis due to high recurrence rate. Whereas, non-FAP-associated intra-abdominal fibromatosis has a low recurrence rate after surgical resection.
Natural history
- Desmoid tumors can develop at virtually any site in the body.
- They can have a wide range of clinical symptoms or no symptoms at all.
- Many desmoid tumors are accidentally picked up on a scan or a routine physical exam done for other medical reasons.
- If left untreated, desmoid tumor produces few symptoms early in the course
- Patients are asymptomatic at the time of diagnosis
- Patients can remain asymptomatic even after many years
- Patients can have a wide range of symptoms anytime depending upon the size and location of tumor
- On some occasions, desmoid tumors can shrink or become quiescent (deep sleep) without any therapy
- Some desmoids may be stable or grow very slowly over a period of months and years
- A small subset of desmoid tumors may be aggressive and grow rapidly
- Hence, desmoid tumors exhibit wide range of behaviors varying from person to person
Complications
Common complications of desmoid tumors include:
- Progression to aggressive fibromatosis
- Surgical complications such as:
- Amputation
- Loss of significant portions of foregut
- Intra-abdomianl/pelvic desmoids can lead to:
- Rupture of intestines
- Compression of the kidneys or ureters
- Rectal bleeding
- Compression of critical blood vessels such as the mesenteric vessels and the vena cava
 |
Prognosis
- Five-year progression-free survival rate is 50% in patients with a primary or recurrent desmoid who are not treated initially with surgery, radiotherapy (RT), or systemic therapy
- Desmoid tumors have become an important cause of morbidity and mortality due to increasing use of prophylactic colectomy in FAP patients[1][2][3][4][5][6]
- Desmoids when become massive and inoperable, can cause death in overall 11% of FAP patients post-colectomy surgery
- 18-31% mortality in patients having desmoids with colorectal carcinoma
- 22% mortality in desmoid patients with periampullary carcinomas[7]
- Due to gradual progression to desmoids, 60% of FAP patients remain alive for 10 years after the diagnosis[6][8][9][10][11][12]
- Pregnancy-associated desmoid fibromatosis is associated with overall good outcomes without any attributable obstetric complications
- FAP-associated intra-abdominal fibromatosis has a high recurrence rate after surgical resection
- Non-FAP-associated intra-abdominal fibromatosis has a low recurrence rate after surgical resection[13]
Recurrence of desmoid tumors
- Recurrence rate is 20% to 77% depending on the location, extent and completeness of the initial resection
- Abdominal wall desmoid tumors have a significantly lower recurrence rate of 20% to 30%
- Abdominal wall desmoids usually becomes evident within six months after excision or in connection with subsequent gestations or deliveries
Prognostic stratification system for FAP-associated desmoids (Cleveland Clinic)
- Following Prognostic stratification system for FAP-associated desmoids was proposed after a study was done in Cleveland Clinic:[6]
| Tumor stage | Characteristic features | Five-year survival rate |
|---|---|---|
| Stage I |
|
95% |
| Stage II |
|
100% |
| Stage III |
|
89% |
| Stage IV |
|
76% |
Reference
- ↑ Church JM (1998). "Mucosal ischemia caused by desmoid tumors in patients with familial adenomatous polyposis: report of four cases". Dis Colon Rectum. 41 (5): 661–3. PMID 9593254.
- ↑ Sagar PM, Möslein G, Dozois RR (1998). "Management of desmoid tumors in patients after ileal pouch-anal anastomosis for familial adenomatous polyposis". Dis Colon Rectum. 41 (11): 1350–5, discussion 1355-6. PMID 9823798.
- ↑ Penna C, Tiret E, Parc R, Sfairi A, Kartheuser A, Hannoun L; et al. (1993). "Operation and abdominal desmoid tumors in familial adenomatous polyposis". Surg Gynecol Obstet. 177 (3): 263–8. PMID 8395084.
- ↑ Kadmon M, Möslein G, Buhr HJ, Herfarth C (1995). "[Desmoid tumors in patients with familial adenomatous polyposis (FAP). Clinical and therapeutic observations from the Heidelberg polyposis register]". Chirurg. 66 (10): 997–1005. PMID 8529453.
- ↑ Arvanitis ML, Jagelman DG, Fazio VW, Lavery IC, McGannon E (1990). "Mortality in patients with familial adenomatous polyposis". Dis Colon Rectum. 33 (8): 639–42. PMID 2165452.
- ↑ 6.0 6.1 6.2 Quintini C, Ward G, Shatnawei A, Xhaja X, Hashimoto K, Steiger E; et al. (2012). "Mortality of intra-abdominal desmoid tumors in patients with familial adenomatous polyposis: a single center review of 154 patients". Ann Surg. 255 (3): 511–6. doi:10.1097/SLA.0b013e31824682d4. PMID 22323009.
- ↑ Seow-Choen F (2008). "The management of desmoids in patients with familial adenomatous polyposis (FAP)". Acta Chir Iugosl. 55 (3): 83–7. PMID 19069698.
- ↑ Soravia C, Berk T, McLeod RS, Cohen Z (2000). "Desmoid disease in patients with familial adenomatous polyposis". Dis Colon Rectum. 43 (3): 363–9. PMID 10733118.
- ↑ Goy BW, Lee SP, Eilber F, Dorey F, Eckardt J, Fu YS; et al. (1997). "The role of adjuvant radiotherapy in the treatment of resectable desmoid tumors". Int J Radiat Oncol Biol Phys. 39 (3): 659–65. PMID 9336146.
- ↑ Lynch HT, Fitzgibbons R (1996). "Surgery, desmoid tumors, and familial adenomatous polyposis: case report and literature review". Am J Gastroenterol. 91 (12): 2598–601. PMID 8946994.
- ↑ Lefevre JH, Parc Y, Kernéis S, Goasguen N, Benis M, Parc R; et al. (2008). "Risk factors for development of desmoid tumours in familial adenomatous polyposis". Br J Surg. 95 (9): 1136–9. doi:10.1002/bjs.6241. PMID 18581438.
- ↑ Schiessling S, Kihm M, Ganschow P, Kadmon G, Büchler MW, Kadmon M (2013). "Desmoid tumour biology in patients with familial adenomatous polyposis coli". Br J Surg. 100 (5): 694–703. doi:10.1002/bjs.9053. PMID 23334997.
- ↑ Wilkinson MJ, Fitzgerald JE, Thomas JM, Hayes AJ, Strauss DC (2012). "Surgical resection for non-familial adenomatous polyposis-related intra-abdominal fibromatosis". Br J Surg. 99 (5): 706–13. doi:10.1002/bjs.8703. PMID 22359346.