COVID-19-associated heart failure: Difference between revisions
| Line 280: | Line 280: | ||
* [[ Echocardiography]] is not recommended routinely in [[COVID-19]] [[ patients]]. However, [[Echocardiography]] may be useful in selected [[COVID-19]] [[patients]] (about 16% ) who have high level of [[D-dimer]] and [[troponin]] level for measurement of [[plmonary arterial pressure]], [[cardiac thrombus]],[[right ventricular function]].<ref name="pmid32963823">{{cite journal |vauthors=Benyounes N, Van Der Vynckt C, Tibi S, Iglesias A, Salomon L, Gout O, Tibi T |title=Echocardiography in Confirmed and Highly Suspected Symptomatic COVID-19 Patients and Its Impact on Treatment Change |journal=Cardiol Res Pract |volume=2020 |issue= |pages=4348598 |date=2020 |pmid=32963823 |pmc=7495215 |doi=10.1155/2020/4348598 |url=}}</ref> | * [[ Echocardiography]] is not recommended routinely in [[COVID-19]] [[ patients]]. However, [[Echocardiography]] may be useful in selected [[COVID-19]] [[patients]] (about 16% ) who have high level of [[D-dimer]] and [[troponin]] level for measurement of [[plmonary arterial pressure]], [[cardiac thrombus]],[[right ventricular function]].<ref name="pmid32963823">{{cite journal |vauthors=Benyounes N, Van Der Vynckt C, Tibi S, Iglesias A, Salomon L, Gout O, Tibi T |title=Echocardiography in Confirmed and Highly Suspected Symptomatic COVID-19 Patients and Its Impact on Treatment Change |journal=Cardiol Res Pract |volume=2020 |issue= |pages=4348598 |date=2020 |pmid=32963823 |pmc=7495215 |doi=10.1155/2020/4348598 |url=}}</ref> | ||
* Among [[COVID-19]] [[patients]] with underlying [[cardiovascular disease]], [[left ventricular function]] commonly was normal. However, presence of [[right ventricular dilation]] and [[dysfunction]] were associated with poor outcome in such situation. | * Among [[COVID-19]] [[patients]] with underlying [[cardiovascular disease]], [[left ventricular function]] commonly was normal. However, presence of [[right ventricular dilation]] and [[dysfunction]] were associated with poor outcome in such situation.<ref name="pmid33796573">{{cite journal |vauthors=Li Y, Fang L, Zhu S, Xie Y, Wang B, He L, Zhang D, Zhang Y, Yuan H, Wu C, Li H, Sun W, Zhang Y, Li M, Cui L, Cai Y, Wang J, Yang Y, Lv Q, Zhang L, Johri AM, Xie M |title=Echocardiographic Characteristics and Outcome in Patients With COVID-19 Infection and Underlying Cardiovascular Disease |journal=Front Cardiovasc Med |volume=8 |issue= |pages=642973 |date=2021 |pmid=33796573 |pmc=8008078 |doi=10.3389/fcvm.2021.642973 |url=}}</ref> | ||
===CT scan=== | ===CT scan=== | ||
Revision as of 07:27, 11 November 2021
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mitra Chitsazan, M.D.[2]Mandana Chitsazan, M.D. [3]
Synonyms and keywords: Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, 2019-nCoV, 2019 novel coronavirus, heart failure, acute heart failure, de Novo acute heart failure, chronic heart failure, acute decompensated heart failure, HFrEF, HFpEF, heart failure with reduced ejection fraction, heart failure with a preserved ejection fraction
Overview
Corona virus disease 2019 COVID-19 caused by a novel enveloped, positively stranded RNA leading to not only respiratory disease, but also multiorgan envolvement. Cardiac complication is one of the manifestation of COVID-19 infection and patients may present with heart failure disease as a consequence of COVID-19 or exacerbation of underlying heart failure disease. History of heart failure disease, regardless of left ventricular ejection fraction, may be a risk factor of severity of COVID-19 course. During the pandemic, heart failure hospitalization reduced about 45% leading to increased in-hospital mortality rates. In addition, evidence of myocardial injury ranging 10-40% in critically ill COVID-19 patients and cardiovascular complications led to increased incidence of acute or chronic heart failure disease. Few cases of myocarditis and severe left ventricular systolic dysfunction associated COVID-19 have been reported. However, studies addressed both systolic and diastolic left ventricular dysfunction, left ventricular diastolic impairnment, pulmonary hypertension, right ventricular dysfunction as the consequence of cardiac involvement in COVID-19 patients.
Historical perspective
- In late December 2019, the novel coronavirus, SARS-CoV-2, originated in Wuhan, China. [1]
- The World Health Organization(WHO) declared the outbreak a Public Health Emergency of International Concern On January 30, 2020, [2] and a pandemic on March 12, 2020. [3]
- On March 27, 2020, Inciardi et al. reported the first case of acute myopericarditis complicated by heart failure in an otherwise healthy 53-year-old woman one week after the onset of symptoms of COVID-19. [4]
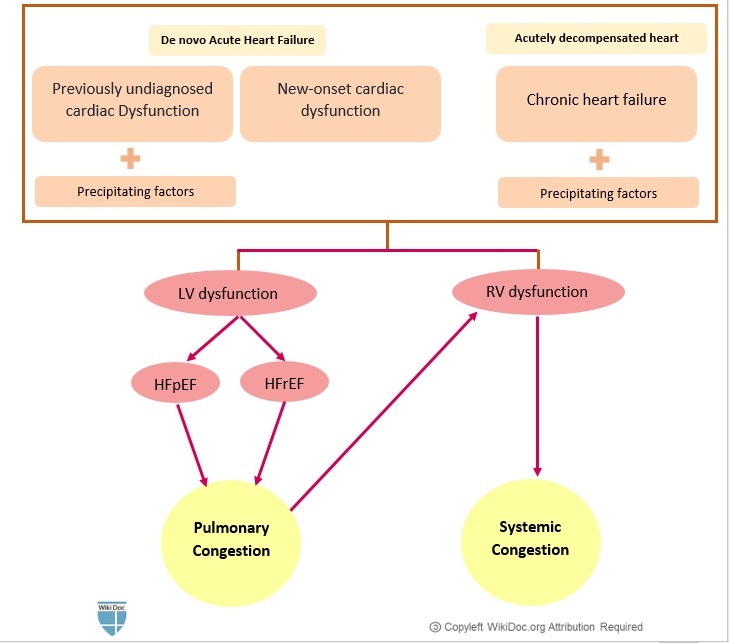
Classification
- Heart Failure (HF) during COVID-19 infection may be classified similarly to heart failure from other causes.
- In general, heart failure can be classified based on:
- The pathophysiology of heart failure:
- The duration of symptoms:
- Acute HF (AHF) vs chronic HF (CHF)
- The underlying physiology based on left ventricular ejection fraction (LVEF):
- The severity of heart failure (i.e., the New York Heart Association Class I-IV)
- The stage of congestive heart failure (i.e., AHA Class A, B, C, D)
- Acute heart failure has two forms:
- Newly-arisen (“de novo”) acute heart failure
- Acutely decompensated chronic heart failure (ADCHF)
Pathophysiology
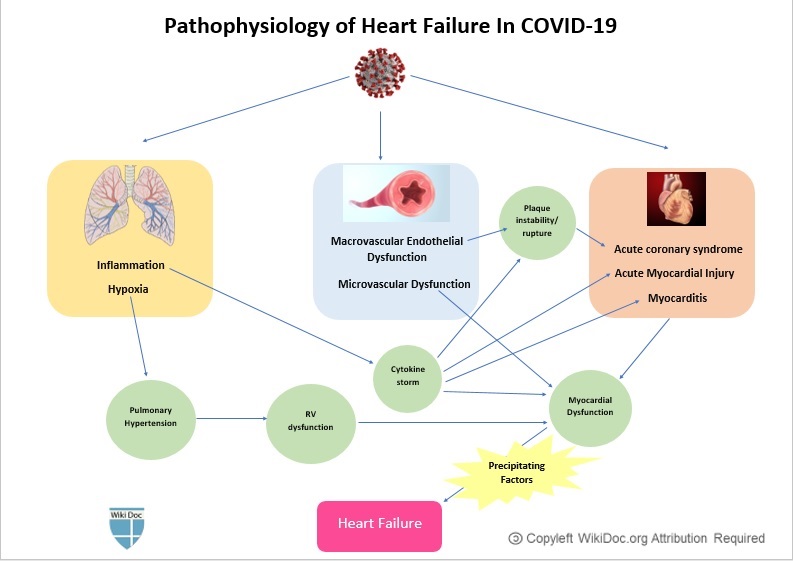
- The pathogenesis of heart failure in COVID-19 has been proposed by two mechanisms of the direct and indirect effect of COVID-19.
- Factors related to indirect mechanisms are:
- Fever, sympathetic activity induced tachycardia and increased myocardial oxygen consumption
- Hypoxia induced oxidative stress and intracellular acidosis and mitocondrial damage and cell death[5]
- Abnormal inflammatory response was ascribed about one week after viral disease and imbalance between T helper type 1 and 2 induced hyperinflammatory response and acute lung injury and ARDS.[6]
- It is thought that release of TNF and IL1B is associated with cardiac injury and myocardial cell depression.[7]
- Cytokin storm was associated with acute heart failure and oxidative stress and inflammation.
- DIC and small vessel thrombosis as a consequence of pulmonary vascular endothelitis and cytokine storm has been seen in the course of COVID-19 infection.[8]
- Use of some medication for COVID-19 caused myocardial injury including some antiviral drugs, hydroxychloroquine and azithromycin with QT prolongation effect and increased risk of VT, Torsades de pointes and death.[9][10]
- Direct mechanism of COVID-19 on myocardium is mediated by attachment of viral spike protients to ACE2 receptor on the myocardium and increased risk of cytokine production, contractil deficit, sarcomer disarray, and cell death.
- Attachment of COVID-19 to ACE2 receptors downregulate ACE2 activity , increased production of angiotensin2 , increased proinflammatory effect, increased proliferation and vasoconstriction and fibrosis.[11]
| Common Precipitating factors in COVID-19 patients |
| Cardiac |
|
| Pressure overload |
|
| Volume overload |
|
|
| Pulmonary |
| Increased systemic metabolic demand |
| Iatrogenic |
|
|
| Others |
|
|
Causes
Acute heart failure in COVID-19 patients may be caused by: [12] [13]
- Acute myocardial injury
- Acute coronary syndromes
- Myocarditis
- Hypertensive crisis
- Arrhythmias: Tachycardia or severe bradycardia
- Stress-induced cardiomyopathy (Takotsubo cardiomyopathy)
- Circulatory failure:
- Iatrogenic
Differentiating COVID-19 associated heart failure from other Diseases
- For further information about the differential diagnosis, click here.
Epidemiology and Demographics
- The prevalence of heart failure was approximately 10,000 per 100,000 SARS-COV-2 infected patients. [14]
Age
- Heart failure commonly affects older patients with COVID-19.
Gender
- There is no data on gender predilection to heart failure in COVID-19.
Race
- There is no data on racial predilection to heart failure COVID-19.
Risk Factors
- The most common risk factors in the development of acute heart failure in COVID-19 patients are:
- Older age
- Pre-existing congestive heart failure
- Well-established risk factors of heart failure, including:
To read more on the risk factors of congestive heart failure, click here.
Screening
- There is insufficient evidence to recommend routine screening for heart failure in COVID-19 patients.
- Routine measurement of natriuretic peptides and/or cardiac troponins has not been recommended in the absence of a high index of suspicion for heart failure on the clinical grounds.
Natural History, Complications, and Prognosis
- Disease may be ranged from asymptomatic , mild symptoms (fever, dry cough, fatigue), or severe disease (severe pneumonia, ARDS, fatal outcome).[15]
- In the presence of heart failure in COVID-19 disease, the course of the disease was much more severe and the risk of hospitalization was high.[16]
- The incidence of acute heart failure increased among COVID-19 patients and was associated with high mortality rates.[17]
- Patients with chronic heart failure may progress to develop acute decompensated heart failure in the setting of COVID-19.
- Discontinuation of guideline-directed medical therapy was associated with higher mortality rate in such patients. [18]
- Myocardial injury and high troponin level may be seen in heart failure associated COVID-19.
- During the pandemic period, heart failure hospitalization reduced ranging from 30% to 66% compared with parallel time due to fear of contracting the virus in hospital.[19]
- Patients with heart failure admitted in the hospital were sicker, presented with higher rates of NYHA 2-3 symptoms, and severe peripheral edema which are the markers of in-hospital mortality.[19]
- Presence of comorbidities including cardiovascular disease, diabetes, chronic respiratory disease, hypertension were associated with fatal outcome in covid-19 patients. [20]
- Among hospitalized COVID-19 patients, presence of heart failure was correlated with higher risk of mechanical ventilation and mortality, regardless of left ventricular ejection fraction.[21]
- Common complication of preexisting heart failure after diagnosis of COVID-19 are:[22]
- In COVID-19 patients presence of underlying cardiovascular disease was associated with poor outcome, and case fatality rate of COVID-19 with cardiovascular comorbidities was 10.5%.[23]
Diagnosis
History and Symptoms
- The most common symptoms of acute heart failure in COVID-19 patients are:
- New or worsening dyspnea: may overlap with dyspnea caused by concomitant respiratory involvement and acute respiratory distress syndrome due to COVID-19
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Peripheral edema
- Fatigue
- Palpitations
- Other common symptoms include:
- Confusion and altered mental status
- Cool extremities
- Cyanosis
- Dizziness
- Syncope
- Hemoptysis
Physical Examination
- Physical examination of patients with acute heart failure is usually remarkable for:
- Tachycardia
- Crackles on lung auscultation
- Distended jugular veins
- Lower extremity edema and/or ascites
- ventricular filling gallop (S3) and/or atrial gallop (S4) on cardiac auscultation
Laboratory Findings
- Cardiac Troponins: [24]
- Elevated cardiac troponin levels suggest the presence of myocardial cell injury or death.
- Cardiac troponin levels may increase in patients with chronic or acute decompensated heart failure.
- Natriuretic Peptides: [25] [26] [27] [28] [29] [30] [31] [32]
- Natriuretic peptides (BNP/NT-proBNP) are released from the heart in response to increased myocardial stress and are quantitative markers of increased intracardiac filling pressure.
- Elevated BNP and NT-proBNP are of both diagnostic and prognostic significance in patients with heart failure.
- Increased BNP or NT-proBNP levels have been demonstrated in COVID-19 patients.
- Increased NT-proBNP level was associated with worse clinical outcomes in patients with severe COVID-19.
- However, increased natriuretic peptide levels are frequently seen among patients with severe inflammatory or respiratory diseases.
- Therefore, routine measurement of BNP/NT-proBNP has not been recommended in COVID-19 patients, unless there is a high suspicion of heart failure based on clinical grounds.
Electrocardiogram
- There is no specific electrocardiographic finding for acute heart failure in COVID-19 patients.
- The ECG may help in identifying preexisting cardiac abnormalities and precipitating factors, such as ischemia, myocarditis, and arrhythmias.
- These ECG findings may include:
- Low QRS Voltage
- Left ventricular hypertrophy
- Left atrial enlargement
- Left bundle branch block
- Poor R progression
- Nonspecific ST-T changes
X-ray
- A Chest x-ray may be helpful in the diagnosis of heart failure. Findings on chest X-ray suggestive of heart failure include:
- Cardiomegaly
- Pulmonary congestion
- Increased pulmonary vascular markings.
- However, signs of pulmonary edema may be obscured by underlying respiratory involvement and acute respiratory distress syndrome due to COVID-19.
Echocardiography or Ultrasound
- Echocardiography is not recommended routinely in COVID-19 patients. However, Echocardiography may be useful in selected COVID-19 patients (about 16% ) who have high level of D-dimer and troponin level for measurement of plmonary arterial pressure, cardiac thrombus,right ventricular function.[33]
- Among COVID-19 patients with underlying cardiovascular disease, left ventricular function commonly was normal. However, presence of right ventricular dilation and dysfunction were associated with poor outcome in such situation.[34]
CT scan
- A Chest CT scan may be helpful in the diagnosis of pulmonary edema in patients with heart failure.
- Findings suggestive of pulmonary edema include:
- Interstitial Edema:
- Gound-glass opacification
- Bronchovascular bundle thickening caused by increased vascular diameter and/or peribronchovascular thickening
- Interlobular septal thickening
- Alveolar edema:
- Airspace consolidation (in addition to findings of interstitial edema).
- Interstitial Edema:
- In patients with cardiogenic pulmonary edema, caused by increased pulmonary vasculature hydrostatic pressure, bilateral pleural effusions are also frequently seen.
CMR
- Due to the risk of contamination of equipment and staff, performing Cardiac magnetic resonance (CMR) should be limited to clinically urgent cases.
- Cardiac magnetic resonance may be helpful in patients suspicious of acute myocarditis, in particular when elevated cardiac biomarkers, ventricular dysfunction and/or severe arrhythmias cannot be explained by other diagnostics and imaging studies.
- To read more on the role of CMR in the diagnosis of myocarditis, click here.
Other Imaging Findings
- To view other imaging findings on COVID-19, click here.
Other Diagnostic Studies
- To view other diagnostic studies for COVID-19, click here.
Treatment
Medical Therapy
- Acute heart failure in the setting of COVID-19 is generally treated similarly to acute heart failure in other settings. These may include:
- Fluid restriction
- Diuretic therapy
- Vasopressors and/or inotropes
- Beta-blockers should not be initiated during the acute stage due to their negative inotropic effects.[35]
- Patients with chronic heart failure are recommended to continue their previous guideline-directed medical therapy, including beta-blockers, ACE inhibitors or Angiotensin II receptor blockers, and mineralocorticoid receptor antagonists. [36]
Interventional therapy
- Extracorporeal membrane oxygenation (ECMO) may be helpful in patients with cardiogenic shock unresponsive to medical therapy.
Surgery
- The mainstay of treatment for acute heart failure is medical therapy.
- Ventricular assisted devices are usually reserved for patients with cardiogenic shock.
Primary Prevention
- There are no established measures for the primary prevention of heart failure in patients with COVID-19.
Secondary Prevention
- During fluid management in heart failure patients, attempts would be done to prevent both volume overload and circulatory failure.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) should be used with caution in patients with acute heart failure due to their effect on fluid and sodium retention.[37]
References
- ↑ "WHO | Pneumonia of unknown cause – China".
- ↑ "WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020".
- ↑ Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M (March 2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1096. PMID 32219357 Check
|pmid=value (help). - ↑ van der Pol A, van Gilst WH, Voors AA, van der Meer P (April 2019). "Treating oxidative stress in heart failure: past, present and future". Eur J Heart Fail. 21 (4): 425–435. doi:10.1002/ejhf.1320. PMC 6607515 Check
|pmc=value (help). PMID 30338885. - ↑ Unudurthi SD, Luthra P, Bose R, McCarthy JR, Kontaridis MI (November 2020). "Cardiac inflammation in COVID-19: Lessons from heart failure". Life Sci. 260: 118482. doi:10.1016/j.lfs.2020.118482. PMC 7505073 Check
|pmc=value (help). PMID 32971105 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE (March 1996). "Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum". J Exp Med. 183 (3): 949–58. doi:10.1084/jem.183.3.949. PMC 2192364. PMID 8642298.
- ↑ Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D (July 2020). "Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19". N Engl J Med. 383 (2): 120–128. doi:10.1056/NEJMoa2015432. PMC 7412750 Check
|pmc=value (help). PMID 32437596 Check|pmid=value (help). - ↑ Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, Wiselka M, Ustianowski A, Elmahi E, Prudon B, Whitehouse T, Felton T, Williams J, Faccenda J, Underwood J, Baillie JK, Chappell LC, Faust SN, Jaki T, Jeffery K, Lim WS, Montgomery A, Rowan K, Tarning J, Watson JA, White NJ, Juszczak E, Haynes R, Landray MJ (November 2020). "Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19". N Engl J Med. 383 (21): 2030–2040. doi:10.1056/NEJMoa2022926. PMC 7556338 Check
|pmc=value (help). PMID 33031652 Check|pmid=value (help). - ↑ Nguyen LS, Dolladille C, Drici MD, Fenioux C, Alexandre J, Mira JP, Moslehi JJ, Roden DM, Funck-Brentano C, Salem JE (July 2020). "Cardiovascular Toxicities Associated With Hydroxychloroquine and Azithromycin: An Analysis of the World Health Organization Pharmacovigilance Database". Circulation. 142 (3): 303–305. doi:10.1161/CIRCULATIONAHA.120.048238. PMC 7365677 Check
|pmc=value (help). PMID 32442023 Check|pmid=value (help). - ↑ Bailey AL, Dmytrenko O, Greenberg L, Bredemeyer AL, Ma P, Liu J, Penna V, Winkler ES, Sviben S, Brooks E, Nair AP, Heck KA, Rali AS, Simpson L, Saririan M, Hobohm D, Stump WT, Fitzpatrick JA, Xie X, Zhang X, Shi PY, Hinson JT, Gi WT, Schmidt C, Leuschner F, Lin CY, Diamond MS, Greenberg MJ, Lavine KJ (April 2021). "SARS-CoV-2 Infects Human Engineered Heart Tissues and Models COVID-19 Myocarditis". JACC Basic Transl Sci. 6 (4): 331–345. doi:10.1016/j.jacbts.2021.01.002. PMC 7909907 Check
|pmc=value (help). PMID 33681537 Check|pmid=value (help). - ↑ Jabri A, Kalra A, Kumar A, Alameh A, Adroja S, Bashir H, Nowacki AS, Shah R, Khubber S, Kanaa'N A, Hedrick DP, Sleik KM, Mehta N, Chung MK, Khot UN, Kapadia SR, Puri R, Reed GW (July 2020). "Incidence of Stress Cardiomyopathy During the Coronavirus Disease 2019 Pandemic". JAMA Netw Open. 3 (7): e2014780. doi:10.1001/jamanetworkopen.2020.14780. PMC 7348683 Check
|pmc=value (help). PMID 32644140 Check|pmid=value (help). - ↑ Minhas AS, Scheel P, Garibaldi B, Liu G, Horton M, Jennings M, Jones SR, Michos ED, Hays AG (May 2020). "Takotsubo Syndrome in the Setting of COVID-19 Infection". JACC Case Rep. doi:10.1016/j.jaccas.2020.04.023. PMC 7194596 Check
|pmc=value (help). PMID 32363351 Check|pmid=value (help). - ↑ Lala A, Johnson KW, Januzzi JL, Russak AJ, Paranjpe I, Richter F, Zhao S, Somani S, Van Vleck T, Vaid A, Chaudhry F, De Freitas JK, Fayad ZA, Pinney SP, Levin M, Charney A, Bagiella E, Narula J, Glicksberg BS, Nadkarni G, Mancini DM, Fuster V (August 2020). "Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection". J Am Coll Cardiol. 76 (5): 533–546. doi:10.1016/j.jacc.2020.06.007. PMC 7279721 Check
|pmc=value (help). PMID 32517963 Check|pmid=value (help). - ↑ Li J, Gong X, Wang Z, Chen R, Li T, Zeng D, Li M (September 2020). "Clinical features of familial clustering in patients infected with 2019 novel coronavirus in Wuhan, China". Virus Res. 286: 198043. doi:10.1016/j.virusres.2020.198043. PMC 7265838 Check
|pmc=value (help). PMID 32502551 Check|pmid=value (help). - ↑ Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI (May 2020). "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study". BMJ. 369: m1966. doi:10.1136/bmj.m1966. PMC 7243801 Check
|pmc=value (help). PMID 32444366 Check|pmid=value (help). - ↑ König S, Hohenstein S, Meier-Hellmann A, Kuhlen R, Hindricks G, Bollmann A (December 2020). "In-hospital care in acute heart failure during the COVID-19 pandemic: insights from the German-wide Helios hospital network". Eur J Heart Fail. 22 (12): 2190–2201. doi:10.1002/ejhf.2044. PMID 33135851 Check
|pmid=value (help). - ↑ Rey JR, Caro-Codón J, Rosillo SO, Iniesta ÁM, Castrejón-Castrejón S, Marco-Clement I, Martín-Polo L, Merino-Argos C, Rodríguez-Sotelo L, García-Veas JM, Martínez-Marín LA, Martínez-Cossiani M, Buño A, Gonzalez-Valle L, Herrero A, López-Sendón JL, Merino JL (December 2020). "Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications". Eur J Heart Fail. 22 (12): 2205–2215. doi:10.1002/ejhf.1990. PMC 7461427 Check
|pmc=value (help). PMID 32833283 Check|pmid=value (help). - ↑ 19.0 19.1 Shah N, Ahmed I, Nazir T (February 2021). "Heart failure-related hospitalisation and management during the COVID-19 pandemic: a reflection. Letter regarding the article 'The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic'". Eur J Heart Fail. 23 (2): 343–344. doi:10.1002/ejhf.1931. PMC 7300617 Check
|pmc=value (help). PMID 32519793 Check|pmid=value (help). - ↑ Cannatà A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M, Piper S, Shah AM, McDonagh TA (December 2020). "Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London". Eur J Heart Fail. 22 (12): 2219–2224. doi:10.1002/ejhf.1986. PMC 7461082 Check
|pmc=value (help). PMID 32809274 Check|pmid=value (help). - ↑ Alvarez-Garcia J, Lee S, Gupta A, Cagliostro M, Joshi AA, Rivas-Lasarte M, Contreras J, Mitter SS, LaRocca G, Tlachi P, Brunjes D, Glicksberg BS, Levin MA, Nadkarni G, Fayad Z, Fuster V, Mancini D, Lala A (November 2020). "Prognostic Impact of Prior Heart Failure in Patients Hospitalized With COVID-19". J Am Coll Cardiol. 76 (20): 2334–2348. doi:10.1016/j.jacc.2020.09.549. PMC 7598769 Check
|pmc=value (help). PMID 33129663 Check|pmid=value (help). - ↑ Tomasoni D, Inciardi RM, Lombardi CM, Tedino C, Agostoni P, Ameri P, Barbieri L, Bellasi A, Camporotondo R, Canale C, Carubelli V, Carugo S, Catagnano F, Dalla Vecchia LA, Danzi GB, Di Pasquale M, Gaudenzi M, Giovinazzo S, Gnecchi M, Iorio A, La Rovere MT, Leonardi S, Maccagni G, Mapelli M, Margonato D, Merlo M, Monzo L, Mortara A, Nuzzi V, Piepoli M, Porto I, Pozzi A, Sarullo F, Sinagra G, Volterrani M, Zaccone G, Guazzi M, Senni M, Metra M (December 2020). "Impact of heart failure on the clinical course and outcomes of patients hospitalized for COVID-19. Results of the Cardio-COVID-Italy multicentre study". Eur J Heart Fail. 22 (12): 2238–2247. doi:10.1002/ejhf.2052. PMID 33179839 Check
|pmid=value (help). - ↑ Bae S, Kim SR, Kim MN, Shim WJ, Park SM (March 2021). "Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis". Heart. 107 (5): 373–380. doi:10.1136/heartjnl-2020-317901. PMC 7747496 Check
|pmc=value (help). PMID 33334865 Check|pmid=value (help). - ↑ Kociol RD, Pang PS, Gheorghiade M, Fonarow GC, O'Connor CM, Felker GM (2010). "Troponin elevation in heart failure prevalence, mechanisms, and clinical implications". J Am Coll Cardiol. 56 (14): 1071–8. doi:10.1016/j.jacc.2010.06.016. PMID 20863950.
- ↑ Saenger AK, Rodriguez-Fraga O, Ler R, Ordonez-Llanos J, Jaffe AS, Goetze JP; et al. (2017). "Specificity of B-Type Natriuretic Peptide Assays: Cross-Reactivity with Different BNP, NT-proBNP, and proBNP Peptides". Clin Chem. 63 (1): 351–358. doi:10.1373/clinchem.2016.263749. PMID 28062628.
- ↑ Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B; et al. (2020). "Prognostic value of NT-proBNP in patients with severe COVID-19". Respir Res. 21 (1): 83. doi:10.1186/s12931-020-01352-w. PMC 7156898 Check
|pmc=value (help). PMID 32293449 Check|pmid=value (help). - ↑ Han H, Xie L, Liu R, Yang J, Liu F, Wu K; et al. (2020). "Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China". J Med Virol. 92 (7): 819–823. doi:10.1002/jmv.25809. PMC 7228305 Check
|pmc=value (help). PMID 32232979 Check|pmid=value (help). - ↑ Christ-Crain M, Breidthardt T, Stolz D, Zobrist K, Bingisser R, Miedinger D, Leuppi J, Tamm M, Mueller B, Mueller C (August 2008). "Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia". J. Intern. Med. 264 (2): 166–76. doi:10.1111/j.1365-2796.2008.01934.x. PMID 18298480.
- ↑ Mueller C, Laule-Kilian K, Frana B, Rodriguez D, Scholer A, Schindler C, Perruchoud AP (February 2006). "Use of B-type natriuretic peptide in the management of acute dyspnea in patients with pulmonary disease". Am. Heart J. 151 (2): 471–7. doi:10.1016/j.ahj.2005.03.036. PMID 16442916.
- ↑ Lai CC, Sung MI, Ho CH, Liu HH, Chen CM, Chiang SR, Chao CM, Liu WL, Hsing SC, Cheng KC (March 2017). "The prognostic value of N-terminal proB-type natriuretic peptide in patients with acute respiratory distress syndrome". Sci Rep. 7: 44784. doi:10.1038/srep44784. PMID 28322314.
- ↑ Determann RM, Royakkers AA, Schaefers J, de Boer AM, Binnekade JM, van Straalen JP, Schultz MJ (July 2013). "Serum levels of N-terminal proB-type natriuretic peptide in mechanically ventilated critically ill patients--relation to tidal volume size and development of acute respiratory distress syndrome". BMC Pulm Med. 13: 42. doi:10.1186/1471-2466-13-42. PMID 23837838.
- ↑ Park BH, Park MS, Kim YS, Kim SK, Kang YA, Jung JY, Lim JE, Kim EY, Chang J (August 2011). "Prognostic utility of changes in N-terminal pro-brain natriuretic Peptide combined with sequential organ failure assessment scores in patients with acute lung injury/acute respiratory distress syndrome concomitant with septic shock". Shock. 36 (2): 109–14. doi:10.1097/SHK.0b013e31821d8f2d. PMID 21478812.
- ↑ Benyounes N, Van Der Vynckt C, Tibi S, Iglesias A, Salomon L, Gout O, Tibi T (2020). "Echocardiography in Confirmed and Highly Suspected Symptomatic COVID-19 Patients and Its Impact on Treatment Change". Cardiol Res Pract. 2020: 4348598. doi:10.1155/2020/4348598. PMC 7495215 Check
|pmc=value (help). PMID 32963823 Check|pmid=value (help). - ↑ Li Y, Fang L, Zhu S, Xie Y, Wang B, He L, Zhang D, Zhang Y, Yuan H, Wu C, Li H, Sun W, Zhang Y, Li M, Cui L, Cai Y, Wang J, Yang Y, Lv Q, Zhang L, Johri AM, Xie M (2021). "Echocardiographic Characteristics and Outcome in Patients With COVID-19 Infection and Underlying Cardiovascular Disease". Front Cardiovasc Med. 8: 642973. doi:10.3389/fcvm.2021.642973. PMC 8008078 Check
|pmc=value (help). PMID 33796573 Check|pmid=value (help). - ↑ Teerlink JR, Alburikan K, Metra M, Rodgers JE (2015). "Acute decompensated heart failure update". Curr Cardiol Rev. 11 (1): 53–62. doi:10.2174/1573403x09666131117174414. PMID 24251454.
- ↑ Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland J, de Boer RA, Drexel H, Ben Gal T, Hill L, Jaarsma T, Jankowska EA, Anker MS, Lainscak M, Lewis BS, McDonagh T, Metra M, Milicic D, Mullens W, Piepoli MF, Rosano G, Ruschitzka F, Volterrani M, Voors AA, Filippatos G, Coats A (October 2019). "Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology". Eur. J. Heart Fail. 21 (10): 1169–1186. doi:10.1002/ejhf.1531. PMID 31129923. Vancouver style error: initials (help)
- ↑ Bleumink GS, Feenstra J, Sturkenboom MC, Stricker BH (2003). "Nonsteroidal anti-inflammatory drugs and heart failure". Drugs. 63 (6): 525–34. doi:10.2165/00003495-200363060-00001. PMID 12656651.