COVID-19-associated abdominal pain: Difference between revisions
No edit summary |
|||
| Line 31: | Line 31: | ||
*[[COVID-19-associated diarrhea]] | *[[COVID-19-associated diarrhea]] | ||
*[[COVID-19-associated hepatic injury]] | *[[COVID-19-associated hepatic injury]] | ||
*[[COVID-19]] associated | *[[COVID-19]] associated [[acute abdomen]] (acute [[peritonitis]] and [[gastrointestinal perforation|gut perforation]])<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref> | ||
*[[Anxiety]] associated with | *[[COVID-19]] associated [[pancreatitis]]<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref><ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref> | ||
*[[Anxiety]] associated with [[patient]] condition | |||
==Differentiating abdominal pain due to [[COVID-19]] from other Diseases== | ==Differentiating abdominal pain due to [[COVID-19]] from other Diseases== | ||
| Line 38: | Line 39: | ||
*''[[Ulcerative colitis]]'': A [[relapse]] can have [[symptoms]] similar to [[COVID-19]] such as: [[anorexia]],[[diarrhea]], [[rash]]. A history of [[ulcerative colitis]] is important it is equally important to access for possible [[COVID-19]] infection. Patient should be counselled about the similarities in two diseases. | *''[[Ulcerative colitis]]'': A [[relapse]] can have [[symptoms]] similar to [[COVID-19]] such as: [[anorexia]],[[diarrhea]], [[rash]]. A history of [[ulcerative colitis]] is important it is equally important to access for possible [[COVID-19]] infection. Patient should be counselled about the similarities in two diseases. | ||
*''[[Hepatitis]]'': [[Acute]] [[hepatitis]] especially [[autoimmune hepatitis]] shared common symptoms such as [[fatigue]], [[anorexia]], [[nausea]], [[vomiting]], [[diarrhea]], skin [[rash]]. Some hepatic infections may involve [[pleuritis]] and [[pleural effusion]] thus [[chest pain]].<ref name="pmid22905065">{{cite journal |vauthors=Ponnurangam Nagarajan V, Palaniyadi A, Sathyamoorthi M, Sasitharan R, Shuba S, Padur Sivaraman R, Scott JX |title=Pleural effusion - An unusual cause |journal=Australas Med J |volume=5 |issue=7 |pages=369–72 |date=2012 |pmid=22905065 |pmc=3413004 |doi=10.4066/AMJ.2012.1024 |url=}}</ref> | *''[[Hepatitis]]'': [[Acute]] [[hepatitis]] especially [[autoimmune hepatitis]] shared common symptoms such as [[fatigue]], [[anorexia]], [[nausea]], [[vomiting]], [[diarrhea]], skin [[rash]]. Some hepatic infections may involve [[pleuritis]] and [[pleural effusion]] thus [[chest pain]].<ref name="pmid22905065">{{cite journal |vauthors=Ponnurangam Nagarajan V, Palaniyadi A, Sathyamoorthi M, Sasitharan R, Shuba S, Padur Sivaraman R, Scott JX |title=Pleural effusion - An unusual cause |journal=Australas Med J |volume=5 |issue=7 |pages=369–72 |date=2012 |pmid=22905065 |pmc=3413004 |doi=10.4066/AMJ.2012.1024 |url=}}</ref> | ||
*''Infectious [[diarrhea]]'': | *''Infectious [[diarrhea]]'': Abdominal pain associated with bloody [[diarrhea]] are features of infections such as [[clostridium difficile|C.difficile]], [[shigellosis]] and [[diverticulitis]]. A careful history, physical exam and stool [[RT-PCR]] for [[COVID-19|coronavirus]] can help in diagnosis. | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
| Line 52: | Line 53: | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The appearance of [[abdominal pain]] has no fixed pattern of appearance in the [[COVID-19]] clinical course. | |||
* | * A complication reported is [[gastrointestinal perforation|gut perforation]] due to [[ischemia]].<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
*''Prognosis'': In a meta-analysis by Mao R. et al. the odds ratio for severe disease in patients with [[anorexia]] as one of the [[gastrointestinal]] symptoms were 7.10.<ref name="MaoQiu2020">{{cite journal|last1=Mao|first1=Ren|last2=Qiu|first2=Yun|last3=He|first3=Jin-Shen|last4=Tan|first4=Jin-Yu|last5=Li|first5=Xue-Hua|last6=Liang|first6=Jie|last7=Shen|first7=Jun|last8=Zhu|first8=Liang-Ru|last9=Chen|first9=Yan|last10=Iacucci|first10=Marietta|last11=Ng|first11=Siew C|last12=Ghosh|first12=Subrata|last13=Chen|first13=Min-Hu|title=Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis|journal=The Lancet Gastroenterology & Hepatology|volume=5|issue=7|year=2020|pages=667–678|issn=24681253|doi=10.1016/S2468-1253(20)30126-6}}</ref> | *''Prognosis'': In a meta-analysis by Mao R. et al. the odds ratio for severe disease in patients with [[anorexia]] as one of the [[gastrointestinal]] symptoms were 7.10.<ref name="MaoQiu2020">{{cite journal|last1=Mao|first1=Ren|last2=Qiu|first2=Yun|last3=He|first3=Jin-Shen|last4=Tan|first4=Jin-Yu|last5=Li|first5=Xue-Hua|last6=Liang|first6=Jie|last7=Shen|first7=Jun|last8=Zhu|first8=Liang-Ru|last9=Chen|first9=Yan|last10=Iacucci|first10=Marietta|last11=Ng|first11=Siew C|last12=Ghosh|first12=Subrata|last13=Chen|first13=Min-Hu|title=Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis|journal=The Lancet Gastroenterology & Hepatology|volume=5|issue=7|year=2020|pages=667–678|issn=24681253|doi=10.1016/S2468-1253(20)30126-6}}</ref> | ||
| Line 74: | Line 73: | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*Infectious [[virions]] in the [[gastrointestinal|GI]] or [[respiratory tract]] can be detected via [[Reverse transcription polymerase chain reaction|reverse transcriptase polymerase chain reaction]] (rRT-PCR). | *Infectious [[virions]] in the [[gastrointestinal|GI]] or [[respiratory tract]] can be detected via [[Reverse transcription polymerase chain reaction|reverse transcriptase polymerase chain reaction]] (rRT-PCR). | ||
*There are no specific laboratory findings associated with abdominal pain in [[COVID-19]] patients. [[liver function tests|Biochemical markers of liver injury]] such as [[bilirubin]], [[C-reactive protein|CRP]], [[alanine aminotransferase|ALT]], [[aspartate aminotransferase|AST]] and [[ | *There are no specific laboratory findings associated with abdominal pain in [[COVID-19]] patients. [[liver function tests|Biochemical markers of liver injury]] such as [[bilirubin]], [[C-reactive protein|CRP]], [[alanine aminotransferase|ALT]], [[aspartate aminotransferase|AST]] and [[Gamma-glutamyltransferase|Gamma GT]] may be increased in blood tests.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*[[Serum potassium]] levels are normal in patients but an important test to exclude life-threatening conditions in patients presenting with abdominal pain. | *[[Serum potassium]] levels are normal in patients but an important test to exclude life-threatening conditions in patients presenting with abdominal pain. | ||
*[[Complete blood count]] provides information about the infectious status of the patient via | *[[Complete blood count]] provides information about the infectious status of the patient via [[leukicytosis]] such as in [[upper gastrointestinal bleeding|upper GI bleed]] and [[peritonitis]], or [[lymphocytes]] indicating viral infection. | ||
*Value of [[CRP]] and [[procalcitonin]] provide information on the inflammation and superimposed bacterial source of infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | *Value of [[CRP]] and [[procalcitonin]] provide information on the inflammation and superimposed bacterial source of infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*[[D-Dimer]] levels give information on active bleeding in the body such as [[acute abdomen]] and upper [[gastrointestinal bleeding|upper GI bleed]]) | |||
*[[Rena function tests]] are deranged in a [[dehydrated]] person (increased [[urea]]) and [[patient]] with upper [[gastrointestinal bleed|Upper GI bleed]] or gut perforation as a complication of [[COVID-19]] (increased [[BUN]] and [[creatinine]].<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | |||
===X-ray=== | ===X-ray=== | ||
| Line 87: | Line 88: | ||
===CT scan=== | ===CT scan=== | ||
[[CT scan]] abdomen: CT scan maybe normal or confirm the peri-intestinal inflammatory reaction.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | *[[CT scan]] abdomen: CT scan maybe normal or confirm the peri-intestinal inflammatory reaction in a patient with [[pancreatitis]] associated with [[COVID]].<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*[[CT scan]] of [[abdomen]] reals extensive [[pneumoperitoneum]] and of chest shows [[pneumothorax]] in a patient with [[gastrointestinal perforation|gut perforation]] associated with [[COVID-19]].<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
Revision as of 17:07, 29 June 2020
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Javaria Anwer M.D.[2]
Synonyms and keywords: COVID-19 associated abdominal pain, COVID associated abdominal pain, COVID likned abdominal pain, COVID-19 linked abdominal pain, coronavirus associated abdominal pain, coronavirus related belly pain, abdominal pain associated with COVID-19, abdominal pain associated with SARS CoV2, SARS CoV2 related abdominal pain, SARS CoV2 linked abdomin pain, abdominal pain and COVID-19, abdominal pain and SARS CoV2 ,abdominal pain in COVID, abdomin pain in COVID, abdominal pain in nCoV, abdominal discomfort in COVID-19, abdominal discomfort in SARS CoV2
Overview
Abdominal pain is a vast entity and sometimes a challenge due to its various potential diagnoses. Although COVID-19 is mainly a respiratory disease, abdominal pain is one of the symptoms of COVID-19 infection.
Historical Perspective
- In the first WHO report, a cluster of cases of pneumonia in Wuhan, China were first reported on December 30th, 2019 by Wuhan Municipal Health Commission, China.
- Three bronchoalveolar lavage samples collected from a patient with pneumonia of unknown etiology – a surveillance definition established following the SARS outbreak of 2002-2003 – in Wuhan Jinyintan Hospital. Real-time PCR (RT-PCR) assays on these samples were positive for pan-Betacoronavirus.
- Nanopore sequencing and bioinformatic analyses indicated that the virus had features typical of the coronavirus family and belonged to the Betacoronavirus 2B lineage.A novel coronavirus was eventually identified.[1]
- The first disease outbreak news on the new virus was first published by WHO on 5th January 2020.[2]
- On March 12, 2020, WHO declared the COVID-19 outbreak a pandemic.
- Initially COVID-19 was primarily known as a respiratory disease. In the initial phase of the pandemic, the screening criteria for COVID‐19 did not include symptoms of abdominal pain.
- On Feb 3rd, 2020, a study published by Wang D et al. first described abdominal pain as one of the less common symptoms of COVID-19.[3]
- With the increasing evidence and ongoing research, abdominal pain is now reported to be a common symptom in patients with COVID-19, and the viral infection is suspected in a patient presenting with abdominal pain. Research is underway to develop a better understanding of the etiology, risk factors, and treatment of abdominal pain associated with COVID-19.
Classification
There is no established system for the classification of abdominal pain in COVID-19. But a differentiation can be made based on the organ injury related to COVID-19 causing abdominal pain.
Pathophysiology
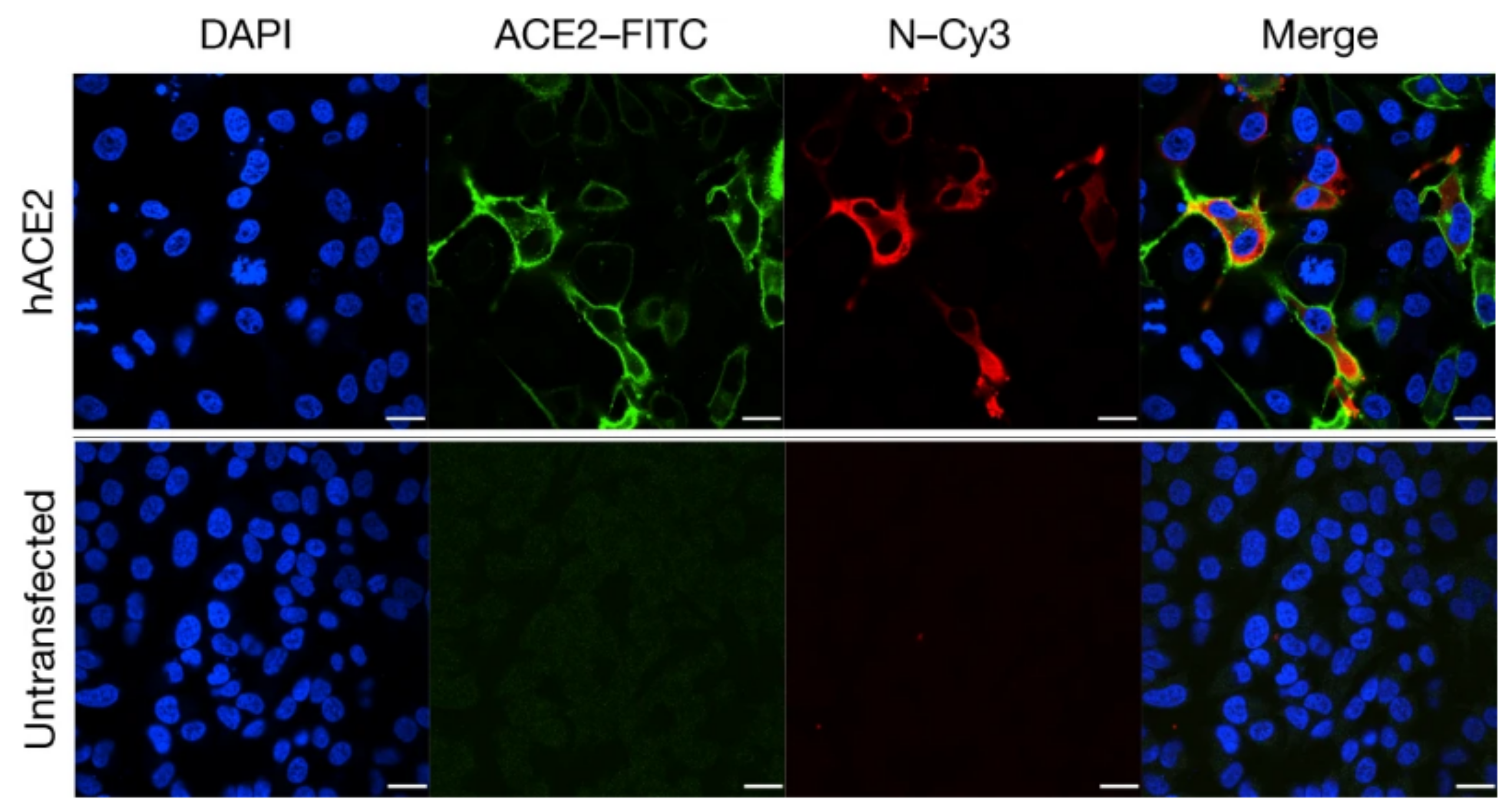
- ACE 2 acts as the SARS-CoV2 receptor for infectivity and the entrance into the cell. Research has shown ACE 2 receptors in esophageal epithelial cells, ileal and colon enterocytes making them vulnerable to COVID-19 infection. The detection of viral nucleocapsid protein in gastrointestinal epithelial cells and viral RNA in fecal specimens reflects the infectivity and chance of direct viral damage of organs.[4][5][6] The entry of the virus causes disruption of the enterocytes and may lead to inflammation, impaired cell permeability, and cellular damage.
- The abdominal pain can be due to direct viral infection of the gastrointestinal tract via cellular ACE 2 receptors in several abdominal organs, making them susceptible to viral infection.
Causes
- COVID-19-associated diarrhea
- COVID-19-associated hepatic injury
- COVID-19 associated acute abdomen (acute peritonitis and gut perforation)[7]
- COVID-19 associated pancreatitis[8][9]
- Anxiety associated with patient condition
Differentiating abdominal pain due to COVID-19 from other Diseases
- Crohn's disease: The disease may have [[remission]s] and relapses and present with symptoms shared by COVID-19 infection as well specially during a relapse. Other symptoms of Crohn's disease include anorexia, diarrhea that may or may not be bloody, fever and rash. A history of Crohn's disease can help the clinician decide on the differential diagnosis but it is equally important to access for possible COVID-19 infection. Patient should be counselled about the similarities in two diseases.
- Ulcerative colitis: A relapse can have symptoms similar to COVID-19 such as: anorexia,diarrhea, rash. A history of ulcerative colitis is important it is equally important to access for possible COVID-19 infection. Patient should be counselled about the similarities in two diseases.
- Hepatitis: Acute hepatitis especially autoimmune hepatitis shared common symptoms such as fatigue, anorexia, nausea, vomiting, diarrhea, skin rash. Some hepatic infections may involve pleuritis and pleural effusion thus chest pain.[10]
- Infectious diarrhea: Abdominal pain associated with bloody diarrhea are features of infections such as C.difficile, shigellosis and diverticulitis. A careful history, physical exam and stool RT-PCR for coronavirus can help in diagnosis.
Epidemiology and Demographics
- Based upon the meta-analysis including 78 studies the Weighted Pooled Prevalence (WPP) of abdominal pain associated with COVID-19 is approximately 6.2% (2.6%-10.3%). Although the data comes from four studies, the WPP of abdominal pain at illness onset was 4.1% and at admission was 7.3%.[11]
Age
- Very limited data is available about the detailed demographics of the patients having abdominal pain as one of the symptoms of COVID-19 infection. A study reporting 10 cases presenting with abdominal pain as one of the symptoms showed the mean age of 50±18 years.
Race
- Data from 12797 patients showed a higher weighted pooled prevalence of abdominal pain associated with COVID-19 in the non-Chinese subgroup.
Risk Factors
- The main risk factor for the development of the disease is COVID-19 infection.
- The incidence of abdominal pain and diarrhea is higher in patients with severe COVID-19.
Natural History, Complications and Prognosis
- The appearance of abdominal pain has no fixed pattern of appearance in the COVID-19 clinical course.
- A complication reported is gut perforation due to ischemia.[12]
- Prognosis: In a meta-analysis by Mao R. et al. the odds ratio for severe disease in patients with anorexia as one of the gastrointestinal symptoms were 7.10.[13]
Diagnosis
Diagnostic Criteria
- There are no established diagnostic criteria to identify the cause of abdominal pain in SARS-CoV2 patient. Abdominal ultrasound or CT scan, and blood tests showing deranged liver functions can give a clue of possible gastrointestinal involvement.
History and Symptoms
- The patient may have abdominal pain as an accompanying symptom along with other SARS-CoV2 infection symptoms such as anorexia, fever, cough, and malaise. Very few patients present with abdominal pain as the sole symptom and high suspicion is required in order to reach the diagnosis.
Physical Examination
- Patients with abdominal pain associated with COVID-19 can be in distress due to their general condition or the severity of abdominal pain. A person with pancreatitis will appear dehydrated, lethargic and in severe pain.
- The patient can be febrile due to COVID-19 infection, hypothermic, or have a normal temperature.
- Shallow breathing can be due to severe respiratory distress or severe abdominal pain.[14]
- A COVID-19 positive patient may have pulmonary manifestations depicting pneumonia or ARDS.
- Based of a few case reports generalised abdominal or epigastric tenderness or right iliac fossa tenderness may accompany the symptom mimicking acute appendicitis.[15][9]
Laboratory Findings
- Infectious virions in the GI or respiratory tract can be detected via reverse transcriptase polymerase chain reaction (rRT-PCR).
- There are no specific laboratory findings associated with abdominal pain in COVID-19 patients. Biochemical markers of liver injury such as bilirubin, CRP, ALT, AST and Gamma GT may be increased in blood tests.[14]
- Serum potassium levels are normal in patients but an important test to exclude life-threatening conditions in patients presenting with abdominal pain.
- Complete blood count provides information about the infectious status of the patient via leukicytosis such as in upper GI bleed and peritonitis, or lymphocytes indicating viral infection.
- Value of CRP and procalcitonin provide information on the inflammation and superimposed bacterial source of infection.[14]
- D-Dimer levels give information on active bleeding in the body such as acute abdomen and upper upper GI bleed)
- Rena function tests are deranged in a dehydrated person (increased urea) and patient with upper Upper GI bleed or gut perforation as a complication of COVID-19 (increased BUN and creatinine.[12]
X-ray
- A Chest X-ray may be normal or show consolidation, bilateral perihilar and interstitial opacities opacities with air bronchograms.
- Abdominal Xray has been reported to be normal in a few studies available.[9][15]
Ultrasound
Ultrasound of the abdomen may or may not show any abnormal findings. A case of bowel inflammatory signs (peri-intestinal inflammatory reaction) has been reported in a patient with abdominal pain associated with COVID-19.[14]
CT scan
- CT scan abdomen: CT scan maybe normal or confirm the peri-intestinal inflammatory reaction in a patient with pancreatitis associated with COVID.[14]
- CT scan of abdomen reals extensive pneumoperitoneum and of chest shows pneumothorax in a patient with gut perforation associated with COVID-19.[12]
Other Imaging Findings
A study by Poggiali et al. strongly recommends bedside lung ultrasound to detect the signs of respiratory COVID-19 infection even when there are no respiratory symptoms.[14]
Treatment
Medical Therapy
- The mainstay of therapy for COVID-19 associated abdominal pain is antiviral therapy, including lopinavir and ritonavir tablets. Treating the infection treats the direct cause of gut damage.
- Supportive care such as IV fluid therapy is essential especially if vomiting accompanies anorexia.
- Associated vomiting is treated with antiemetic drugs and diarrhea is treated with antidiarrheal drugs such as loperamide if C.difficile infection has been ruled out.
- Although the COVID-19 infection and IBDs mimic in some parameters, glucocorticoids treatment should not be abruptly discontinued. It can be maintained at the lowest dose possible.[16]
- Response to medical therapy can be monitored with the patient's general condition, symptoms, vital signs, and US of the abdomen or CT scan abdomen if required.
Surgery
- An acute abdomen associated with COVID-19 having complications such as gut perforation requires surgery. The reported procedures performed include exploratory laparotomy, followed by GI repair or partial resection.[7]
Primary Prevention
- There have been rigorous efforts in order to develop a vaccine for novel coronavirus and several vaccines are in the later phases of trials.[17]
- The only prevention for COVID-19 associated abdominal pain is the prevention and early diagnosis of the coronavirus-19 infection itself. According to the CDC, the measures include:[18]
- Frequent handwashing with soap and water for at least 20 seconds or using a alcohol based hand sanitizer with at least 60% alcohol.
- Staying at least 6 feet (about 2 arms’ length) from other people who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
Secondary prevention
- Contact tracing helps reduce the spread of the disease.[19]
- For the prevention of transmission through gastrointestinal tract (presence of viral RNA in the stool raise suspicion for fecal-oral transmission)
- Use of personal protective equipment (PPE) by the personnel handling the fecal matter.
- Screening of fecal microbiota transplant donors for COVID-19 is also recommended.[20]
References
- ↑ "www.who.int" (PDF).
- ↑ "WHO Timeline - COVID-19".
- ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ Zou, Xin; Chen, Ke; Zou, Jiawei; Han, Peiyi; Hao, Jie; Han, Zeguang (2020). "Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection". Frontiers of Medicine. 14 (2): 185–192. doi:10.1007/s11684-020-0754-0. ISSN 2095-0217.
- ↑ Tian Y, Rong L, Nian W, He Y (May 2020). "Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission". Aliment. Pharmacol. Ther. 51 (9): 843–851. doi:10.1111/apt.15731. PMC 7161803 Check
|pmc=value (help). PMID 32222988 Check|pmid=value (help). - ↑ Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY (May 2020). "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2". Circ. Res. 126 (10): 1456–1474. doi:10.1161/CIRCRESAHA.120.317015. PMC 7188049 Check
|pmc=value (help). PMID 32264791 Check|pmid=value (help). - ↑ 7.0 7.1 Gao Y, Xi H, Chen L (July 2020). "Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives". Ann. Surg. 272 (1): e38–e39. doi:10.1097/SLA.0000000000003961. PMC 7188052 Check
|pmc=value (help). PMID 32301807 Check|pmid=value (help). - ↑ Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H (May 2020). "COVID-19 presenting as acute pancreatitis". Pancreatology. doi:10.1016/j.pan.2020.05.003. PMC 7207100 Check
|pmc=value (help). PMID 32444169 Check|pmid=value (help). - ↑ 9.0 9.1 9.2 Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL (June 2020). "Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members". Pancreatology. 20 (4): 665–667. doi:10.1016/j.pan.2020.04.021. PMC 7199002 Check
|pmc=value (help). PMID 32387082 Check|pmid=value (help). - ↑ Ponnurangam Nagarajan V, Palaniyadi A, Sathyamoorthi M, Sasitharan R, Shuba S, Padur Sivaraman R, Scott JX (2012). "Pleural effusion - An unusual cause". Australas Med J. 5 (7): 369–72. doi:10.4066/AMJ.2012.1024. PMC 3413004. PMID 22905065.
- ↑ Tariq, Raseen; Saha, Srishti; Furqan, Fateeha; Hassett, Leslie; Pardi, Darrell; Khanna, Sahil (2020). "Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis". Mayo Clinic Proceedings. doi:10.1016/j.mayocp.2020.06.003. ISSN 0025-6196.
- ↑ 12.0 12.1 12.2 Corrêa Neto, Isaac José Felippe; Viana, Kaline Fortes; Silva, Milena Braga Soares da; Silva, Leandro Mariano da; Oliveira, Gustavo de; Cecchini, Angelo Rossi da Silva; Rolim, Alexander Sá; Robles, Laercio (2020). "Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease". Journal of Coloproctology. doi:10.1016/j.jcol.2020.05.011. ISSN 2237-9363.
- ↑ Mao, Ren; Qiu, Yun; He, Jin-Shen; Tan, Jin-Yu; Li, Xue-Hua; Liang, Jie; Shen, Jun; Zhu, Liang-Ru; Chen, Yan; Iacucci, Marietta; Ng, Siew C; Ghosh, Subrata; Chen, Min-Hu (2020). "Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis". The Lancet Gastroenterology & Hepatology. 5 (7): 667–678. doi:10.1016/S2468-1253(20)30126-6. ISSN 2468-1253.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A (2020). "Abdominal Pain: A Real Challenge in Novel COVID-19 Infection". Eur J Case Rep Intern Med. 7 (4): 001632. doi:10.12890/2020_001632. PMC 7162568 Check
|pmc=value (help). PMID 32309266 Check|pmid=value (help). - ↑ 15.0 15.1 Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L (2020). "Can COVID 19 present like appendicitis?". IDCases. 21: e00860. doi:10.1016/j.idcr.2020.e00860. PMC 7265835 Check
|pmc=value (help). PMID 32523872 Check|pmid=value (help). - ↑ Queiroz N, Barros LL, Azevedo M, Oba J, Sobrado CW, Carlos AS, Milani LR, Sipahi AM, Damião A (2020). "Management of inflammatory bowel disease patients in the COVID-19 pandemic era: a Brazilian tertiary referral center guidance". Clinics (Sao Paulo). 75: e1909. doi:10.6061/clinics/2020/e1909. PMC 7153358 Check
|pmc=value (help). PMID 32321117 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ "NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)".
- ↑ "How to Protect Yourself & Others | CDC".
- ↑ "Contact Tracing for COVID-19 | CDC".
- ↑ Green CA, Quraishi MN, Shabir S, Sharma N, Hansen R, Gaya DR, Hart AL, Loman NJ, Iqbal TH (June 2020). "Screening faecal microbiota transplant donors for SARS-CoV-2 by molecular testing of stool is the safest way forward". Lancet Gastroenterol Hepatol. 5 (6): 531. doi:10.1016/S2468-1253(20)30089-3. PMC 7225406 Check
|pmc=value (help). PMID 32240618 Check|pmid=value (help).