Barrett's esophagus pathophysiology: Difference between revisions
Amresh Kumar (talk | contribs) |
No edit summary |
||
| (22 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{AMK}} | {{CMG}}; {{AE}} {{AMK}} | ||
==Overview== | ==Overview== | ||
Barrett's esophagus is marked by the presence of [[columnar epithelium]] in the lower [[esophagus]], replacing the [[normal]] [[squamous cell]] [[epithelium]]; an example of [[metaplasia]]. The [[columnar epithelium]] is better able to withstand the erosive action of the [[gastric]] [[secretions]]; however, this [[metaplasia]] confers an increased [[cancer]] risk of the [[adenocarcinoma]] type. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
* | * Barrett's esophagus (BE) is the [[metaplasia]] which occurs due to change in [[epithelium]] from normal squamous cell epithelium to columnar cell epithelium in the lower end of esophagus due to the [[corrosive]] action of [[gastric]] [[secretions]] in the lower end of the [[esophagus]].<ref name="pmid11342767">{{cite journal| author=Glickman JN, Chen YY, Wang HH, Antonioli DA, Odze RD| title=Phenotypic characteristics of a distinctive multilayered epithelium suggests that it is a precursor in the development of Barrett's esophagus. | journal=Am J Surg Pathol | year= 2001 | volume= 25 | issue= 5 | pages= 569-78 | pmid=11342767 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11342767 }} </ref><ref name="pmid2921087">{{cite journal| author=Gatermann S, Schulz E, Marre R| title=The microbiological efficacy of the combination of fosfomycin and vancomycin against clinically relevant staphylococci. | journal=Infection | year= 1989 | volume= 17 | issue= 1 | pages= 35-7 | pmid=2921087 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2921087 }} </ref> Barrett's esophagus has increased risk of developing into [[Esophageal cancer|esophageal adenocarcinoma]].<ref name="Fléjou_2005">{{cite journal |author=Fléjou J |title=Barrett's oesophagus: from metaplasia to dysplasia and cancer |journal=Gut |volume=54 Suppl 1 |issue= |pages=i6-12 |year=2005 |pmid=15711008}}</ref><ref name="pmid29066320">{{cite journal| author=Rumiato E, Boldrin E, Malacrida S, Realdon S, Fassan M, Morbin T et al.| title=Detection of genetic alterations in cfDNA as a possible strategy to monitor the neoplastic progression of Barrett's esophagus. | journal=Transl Res | year= 2017 | volume= 190 | issue= | pages= 16-24.e1 | pmid=29066320 | doi=10.1016/j.trsl.2017.09.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29066320 }} </ref><ref name="pmid11353048">{{cite journal| author=Bian YS, Osterheld MC, Bosman FT, Benhattar J, Fontolliet C| title=p53 gene mutation and protein accumulation during neoplastic progression in Barrett's esophagus. | journal=Mod Pathol | year= 2001 | volume= 14 | issue= 5 | pages= 397-403 | pmid=11353048 | doi=10.1038/modpathol.3880324 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11353048 }} </ref> | ||
* | * There are two types of [[cells]] occur in the [[Metaplasticity|metaplastic]] [[columnar epithelium]] of Barrett's esophagus: one is [[gastric]] type and other is colonic type. [[Gastric]] type resemble the same cells which line the gastric epithelium and colonic type resembles the same cells lining the [[intestinal]] [[epithelium]]. There will be combination of both type of [[cells]] seen on the [[biopsies]] taken from these [[patients]] during the [[endoscopy]]. The type of [[metaplasia]] in which there is increased chance of developing into Barrett's esophagus is colonic type [[metaplasia]] in patients with increased [[genetic]] risk.<ref name="pmid12171951">{{cite journal| author=Chak A, Lee T, Kinnard MF, Brock W, Faulx A, Willis J et al.| title=Familial aggregation of Barrett's oesophagus, oesophageal adenocarcinoma, and oesophagogastric junctional adenocarcinoma in Caucasian adults. | journal=Gut | year= 2002 | volume= 51 | issue= 3 | pages= 323-8 | pmid=12171951 | doi= | pmc=1773365 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12171951 }} </ref><ref name="pmid24480679">{{cite journal| author=Verbeek RE, Spittuler LF, Peute A, van Oijen MG, Ten Kate FJ, Vermeijden JR et al.| title=Familial clustering of Barrett's esophagus and esophageal adenocarcinoma in a European cohort. | journal=Clin Gastroenterol Hepatol | year= 2014 | volume= 12 | issue= 10 | pages= 1656-63.e1 | pmid=24480679 | doi=10.1016/j.cgh.2014.01.028 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24480679 }} </ref><ref name="pmid29073141">{{cite journal| author=Sun X, Chandar AK, Canto MI, Thota PN, Brock M, Shaheen NJ et al.| title=Genomic regions associated with susceptibility to Barrett's esophagus and esophageal adenocarcinoma in African Americans: The cross BETRNet admixture study. | journal=PLoS One | year= 2017 | volume= 12 | issue= 10 | pages= e0184962 | pmid=29073141 | doi=10.1371/journal.pone.0184962 | pmc=5657624 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29073141 }} </ref><ref name="pmid27486097">{{cite journal| author=Buas MF, He Q, Johnson LG, Onstad L, Levine DM, Thrift AP et al.| title=Germline variation in inflammation-related pathways and risk of Barrett's oesophagus and oesophageal adenocarcinoma. | journal=Gut | year= 2017 | volume= 66 | issue= 10 | pages= 1739-1747 | pmid=27486097 | doi=10.1136/gutjnl-2016-311622 | pmc=5296402 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27486097 }} </ref><ref name="pmid26783083">{{cite journal| author=Becker J, May A, Gerges C, Anders M, Schmidt C, Veits L et al.| title=The Barrett-associated variants at GDF7 and TBX5 also increase esophageal adenocarcinoma risk. | journal=Cancer Med | year= 2016 | volume= 5 | issue= 5 | pages= 888-91 | pmid=26783083 | doi=10.1002/cam4.641 | pmc=4864818 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26783083 }} </ref><ref name="pmid26414697">{{cite journal| author=Ek WE, Lagergren K, Cook M, Wu AH, Abnet CC, Levine D et al.| title=Polymorphisms in genes in the androgen pathway and risk of Barrett's esophagus and esophageal adenocarcinoma. | journal=Int J Cancer | year= 2016 | volume= 138 | issue= 5 | pages= 1146-52 | pmid=26414697 | doi=10.1002/ijc.29863 | pmc=4715576 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26414697 }} </ref><ref name="pmid14518305">{{cite journal| author=Schneider PM, Hölscher AH, Wegerer S, König U, Becker K, Siewert JR| title=[Clinical significance of p53 tumor suppressor gene mutations in adenocarcinoma in Barrett esophagus]. | journal=Langenbecks Arch Chir Suppl Kongressbd | year= 1998 | volume= 115 | issue= Suppl I | pages= 495-9 | pmid=14518305 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14518305 }} </ref> | ||
* | * Barrett's esophagus can be seen grossly by its red/light brown color of its [[mucosa]] as compared to the light pink color of normal [[mucosa]] of [[esophagus]] under [[endoscopic]] [[examination]], but it is very important to take [[biopsy]] specimens during [[endoscopic]] [[examination]] and should be microscopically examined to see what type of [[cells]] are present among both the types of [[gastric]] and colonic type of [[cells]]. To make the final [[diagnosis]] of Barrett's, it is very necessary to find the colonic [[metaplasia]] and which can be identified by finding of the [[goblet cells]] in the [[epithelium]] of the [[biopsy]] specimens.<ref name="pmid26783083" /><ref name="pmid26414697" /><ref name="pmid14518305" /> | ||
* | * One of the main causes of the Barrett's esophagus is [[GERD|gastroesophageal reflux disease (GERD)]]. It has been seen in many studies that chronic [[reflux]] caused by [[GERD]] induces a vicious circle of [[injury|injuries]] and repair cycle in the [[squamous epithelium]] of [[esophagus]]. By this process, it leads to change of epithelium from normal squamous epithelium to the [[columnar epithelium]] as [[columnar epithelium]] is less susceptible to the [[injury]] caused by the [[acid]] [[injury]] as compared to the [[squamous epithelium]].<ref>Spechler SJ. Barrett's esophagus. Semin Gastrointest Dis 1996; 7:51.</ref><ref name="pmid8705259">{{cite journal| author=Spechler SJ| title=Barrett's esophagus. | journal=Semin Gastrointest Dis | year= 1996 | volume= 7 | issue= 2 | pages= 51-60 | pmid=8705259 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8705259 }} </ref><ref name="pmid4146903">{{cite journal| author=Lavy UI, Funcke AB, van Hell G, Timmerman H| title=Pharmacological properties of ((3alpha-tropanyl)oxy)-5H-benzo(4,5)cycloheptal(1,2-b)-pyridine hydrogen maleate (BS 7723). | journal=Arzneimittelforschung | year= 1973 | volume= 23 | issue= 6 | pages= 854-8 | pmid=4146903 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4146903 }} </ref><ref name="pmid10929625">{{cite journal| author=von Schrenck T| title=[Diagnosis of gastroesophageal reflux and Barrett esophagus]. | journal=Zentralbl Chir | year= 2000 | volume= 125 | issue= 5 | pages= 414-23 | pmid=10929625 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10929625 }} </ref><ref name="pmid28336546">{{cite journal| author=Minacapelli CD, Bajpai M, Geng X, Cheng CL, Chouthai AA, Souza R et al.| title=Barrett's metaplasia develops from cellular reprograming of esophageal squamous epithelium due to gastroesophageal reflux. | journal=Am J Physiol Gastrointest Liver Physiol | year= 2017 | volume= 312 | issue= 6 | pages= G615-G622 | pmid=28336546 | doi=10.1152/ajpgi.00268.2016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28336546 }} </ref> | ||
* | * [[Patients]] with BE tend to have more severe [[GERD]]. | ||
* Although one would think that BE develops over years, with [[slow]] replacement of [[squamous]] [[cells]] by columnar [[cells]], it appears that this is not the case. BE tends to develop all at once with little or no progression. The reason for this is unknown. | |||
* Although one would think that BE develops over years, with [[slow]] replacement of [[squamous]] [[cells]] by | |||
==Genetics== | ==Genetics== | ||
| Line 29: | Line 25: | ||
==Associated Conditions== | ==Associated Conditions== | ||
Barrett's esophagus is associated with following associated conditions: | |||
* [[Gastroesophageal reflux disease]]<ref name="pmid10929625">{{cite journal| author=von Schrenck T| title=[Diagnosis of gastroesophageal reflux and Barrett esophagus]. | journal=Zentralbl Chir | year= 2000 | volume= 125 | issue= 5 | pages= 414-23 | pmid=10929625 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10929625 }} </ref><ref name="pmid28336546">{{cite journal| author=Minacapelli CD, Bajpai M, Geng X, Cheng CL, Chouthai AA, Souza R et al.| title=Barrett's metaplasia develops from cellular reprograming of esophageal squamous epithelium due to gastroesophageal reflux. | journal=Am J Physiol Gastrointest Liver Physiol | year= 2017 | volume= 312 | issue= 6 | pages= G615-G622 | pmid=28336546 | doi=10.1152/ajpgi.00268.2016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28336546 }} </ref><ref name="pmid8705259">{{cite journal| author=Spechler SJ| title=Barrett's esophagus. | journal=Semin Gastrointest Dis | year= 1996 | volume= 7 | issue= 2 | pages= 51-60 | pmid=8705259 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8705259 }} </ref> | * [[Gastroesophageal reflux disease]]<ref name="pmid10929625">{{cite journal| author=von Schrenck T| title=[Diagnosis of gastroesophageal reflux and Barrett esophagus]. | journal=Zentralbl Chir | year= 2000 | volume= 125 | issue= 5 | pages= 414-23 | pmid=10929625 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10929625 }} </ref><ref name="pmid28336546">{{cite journal| author=Minacapelli CD, Bajpai M, Geng X, Cheng CL, Chouthai AA, Souza R et al.| title=Barrett's metaplasia develops from cellular reprograming of esophageal squamous epithelium due to gastroesophageal reflux. | journal=Am J Physiol Gastrointest Liver Physiol | year= 2017 | volume= 312 | issue= 6 | pages= G615-G622 | pmid=28336546 | doi=10.1152/ajpgi.00268.2016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28336546 }} </ref><ref name="pmid8705259">{{cite journal| author=Spechler SJ| title=Barrett's esophagus. | journal=Semin Gastrointest Dis | year= 1996 | volume= 7 | issue= 2 | pages= 51-60 | pmid=8705259 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8705259 }} </ref> | ||
* [[Systemic Sclerosis]]<ref name="pmid16142744">{{cite journal| author=Wipff J, Allanore Y, Soussi F, Terris B, Abitbol V, Raymond J et al.| title=Prevalence of Barrett's esophagus in systemic sclerosis. | journal=Arthritis Rheum | year= 2005 | volume= 52 | issue= 9 | pages= 2882-8 | pmid=16142744 | doi=10.1002/art.21261 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16142744 }} </ref> | * [[Systemic Sclerosis]]<ref name="pmid16142744">{{cite journal| author=Wipff J, Allanore Y, Soussi F, Terris B, Abitbol V, Raymond J et al.| title=Prevalence of Barrett's esophagus in systemic sclerosis. | journal=Arthritis Rheum | year= 2005 | volume= 52 | issue= 9 | pages= 2882-8 | pmid=16142744 | doi=10.1002/art.21261 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16142744 }} </ref> | ||
| Line 36: | Line 31: | ||
==Gross Pathology== | ==Gross Pathology== | ||
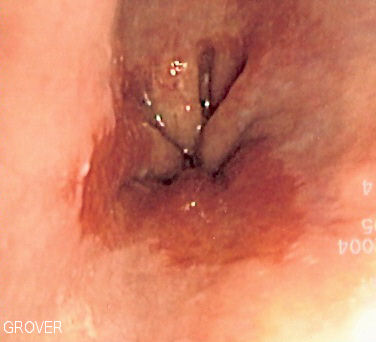
*Normally the [[mucosa]] of normal [[esophagus]] is [[light]] pink [[color]] as seen from | *Normally the [[mucosa]] of normal [[esophagus]] is [[light]] pink [[color]] as seen from underlying picture. | ||
*On [[gross]] [[pathology]], [[Barrett's esophagus]] looks like Red/light brown [[esophageal]] [[mucosa]]. | *On [[gross]] [[pathology]], [[Barrett's esophagus]] looks like Red/light brown [[esophageal]] [[mucosa]]. | ||
[[File:Barretts esophagus.jpg|thumb|center|By Nephron [https://upload.wikimedia.org/wikipedia/commons/8/86/Barretts_esophagus.jpg Source: Libre Pathology]]] | [[File:Barretts esophagus.jpg|thumb|center|By Nephron [https://upload.wikimedia.org/wikipedia/commons/8/86/Barretts_esophagus.jpg Source: Libre Pathology]]] | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic histopathological analysis, gastric junctional type epithelium, gastric fundus type epithelium and specialized intestinal columnar metaplasia are characteristic findings of Barrett's esophagus.<ref name="pmid22943014">{{cite journal| author=Booth CL, Thompson KS| title=Barrett's esophagus: A review of diagnostic criteria, clinical surveillance practices and new developments. | journal=J Gastrointest Oncol | year= 2012 | volume= 3 | issue= 3 | pages= 232-42 | pmid=22943014 | doi=10.3978/j.issn.2078-6891.2012.028 | pmc=3418534 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22943014 }} </ref> | *On microscopic histopathological analysis, gastric junctional type epithelium, gastric fundus type epithelium and specialized intestinal columnar metaplasia are characteristic findings of Barrett's esophagus.<ref name="pmid22943014">{{cite journal| author=Booth CL, Thompson KS| title=Barrett's esophagus: A review of diagnostic criteria, clinical surveillance practices and new developments. | journal=J Gastrointest Oncol | year= 2012 | volume= 3 | issue= 3 | pages= 232-42 | pmid=22943014 | doi=10.3978/j.issn.2078-6891.2012.028 | pmc=3418534 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22943014 }} </ref><ref name="pmid940579">{{cite journal| author=Paull A, Trier JS, Dalton MD, Camp RC, Loeb P, Goyal RK| title=The histologic spectrum of Barrett's esophagus. | journal=N Engl J Med | year= 1976 | volume= 295 | issue= 9 | pages= 476-80 | pmid=940579 | doi=10.1056/NEJM197608262950904 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=940579 }} </ref> | ||
* Paull et.al. described three types of [[columnar epithelium]] that can be seen in BE: | * Paull et.al. described three types of [[columnar epithelium]] that can be seen in BE: | ||
| Line 57: | Line 52: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category: | [[Category:Gastroenterology]] | ||
[[Category:Medicine]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 16:59, 21 February 2018
|
Barrett's Esophagus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Barrett's esophagus pathophysiology On the Web |
|
American Roentgen Ray Society Images of Barrett's esophagus pathophysiology |
|
Risk calculators and risk factors for Barrett's esophagus pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amresh Kumar MD [2]
Overview
Barrett's esophagus is marked by the presence of columnar epithelium in the lower esophagus, replacing the normal squamous cell epithelium; an example of metaplasia. The columnar epithelium is better able to withstand the erosive action of the gastric secretions; however, this metaplasia confers an increased cancer risk of the adenocarcinoma type.
Pathophysiology
Pathogenesis
- Barrett's esophagus (BE) is the metaplasia which occurs due to change in epithelium from normal squamous cell epithelium to columnar cell epithelium in the lower end of esophagus due to the corrosive action of gastric secretions in the lower end of the esophagus.[1][2] Barrett's esophagus has increased risk of developing into esophageal adenocarcinoma.[3][4][5]
- There are two types of cells occur in the metaplastic columnar epithelium of Barrett's esophagus: one is gastric type and other is colonic type. Gastric type resemble the same cells which line the gastric epithelium and colonic type resembles the same cells lining the intestinal epithelium. There will be combination of both type of cells seen on the biopsies taken from these patients during the endoscopy. The type of metaplasia in which there is increased chance of developing into Barrett's esophagus is colonic type metaplasia in patients with increased genetic risk.[6][7][8][9][10][11][12]
- Barrett's esophagus can be seen grossly by its red/light brown color of its mucosa as compared to the light pink color of normal mucosa of esophagus under endoscopic examination, but it is very important to take biopsy specimens during endoscopic examination and should be microscopically examined to see what type of cells are present among both the types of gastric and colonic type of cells. To make the final diagnosis of Barrett's, it is very necessary to find the colonic metaplasia and which can be identified by finding of the goblet cells in the epithelium of the biopsy specimens.[10][11][12]
- One of the main causes of the Barrett's esophagus is gastroesophageal reflux disease (GERD). It has been seen in many studies that chronic reflux caused by GERD induces a vicious circle of injuries and repair cycle in the squamous epithelium of esophagus. By this process, it leads to change of epithelium from normal squamous epithelium to the columnar epithelium as columnar epithelium is less susceptible to the injury caused by the acid injury as compared to the squamous epithelium.[13][14][15][16][17]
- Although one would think that BE develops over years, with slow replacement of squamous cells by columnar cells, it appears that this is not the case. BE tends to develop all at once with little or no progression. The reason for this is unknown.
Genetics
- The development of Barrett's esophagus is the result of multiple genetic mutations including mutations on chromosome 11p in European ancestry, genetic mutation of MGST1, mutations of genes GDF7 and TBX5, polymorphisms in genes in the androgen pathway and genetic mutations in p53 tumor suppressor.[6][7][8][9][10][11][12]
Associated Conditions
Barrett's esophagus is associated with following associated conditions:
Gross Pathology
- Normally the mucosa of normal esophagus is light pink color as seen from underlying picture.
- On gross pathology, Barrett's esophagus looks like Red/light brown esophageal mucosa.
Microscopic Pathology
- On microscopic histopathological analysis, gastric junctional type epithelium, gastric fundus type epithelium and specialized intestinal columnar metaplasia are characteristic findings of Barrett's esophagus.[22][23]
- Paull et.al. described three types of columnar epithelium that can be seen in BE:
- Gastric junctional-type epithelium which has a pitted (foveolar) surface and mucus-secreting cells.
- Gastric fundus-type epithelium that also has a pitted surface lined by mucus-secreting cells, in addition to having a deeper glandular layer that contains chief and parietal cells.
- Specialized intestinal (columnar) metaplasia that has a villiform surface with mucus secreting columnar cells and goblet cells.

References
- ↑ Glickman JN, Chen YY, Wang HH, Antonioli DA, Odze RD (2001). "Phenotypic characteristics of a distinctive multilayered epithelium suggests that it is a precursor in the development of Barrett's esophagus". Am J Surg Pathol. 25 (5): 569–78. PMID 11342767.
- ↑ Gatermann S, Schulz E, Marre R (1989). "The microbiological efficacy of the combination of fosfomycin and vancomycin against clinically relevant staphylococci". Infection. 17 (1): 35–7. PMID 2921087.
- ↑ Fléjou J (2005). "Barrett's oesophagus: from metaplasia to dysplasia and cancer". Gut. 54 Suppl 1: i6–12. PMID 15711008.
- ↑ Rumiato E, Boldrin E, Malacrida S, Realdon S, Fassan M, Morbin T; et al. (2017). "Detection of genetic alterations in cfDNA as a possible strategy to monitor the neoplastic progression of Barrett's esophagus". Transl Res. 190: 16–24.e1. doi:10.1016/j.trsl.2017.09.004. PMID 29066320.
- ↑ Bian YS, Osterheld MC, Bosman FT, Benhattar J, Fontolliet C (2001). "p53 gene mutation and protein accumulation during neoplastic progression in Barrett's esophagus". Mod Pathol. 14 (5): 397–403. doi:10.1038/modpathol.3880324. PMID 11353048.
- ↑ 6.0 6.1 Chak A, Lee T, Kinnard MF, Brock W, Faulx A, Willis J; et al. (2002). "Familial aggregation of Barrett's oesophagus, oesophageal adenocarcinoma, and oesophagogastric junctional adenocarcinoma in Caucasian adults". Gut. 51 (3): 323–8. PMC 1773365. PMID 12171951.
- ↑ 7.0 7.1 Verbeek RE, Spittuler LF, Peute A, van Oijen MG, Ten Kate FJ, Vermeijden JR; et al. (2014). "Familial clustering of Barrett's esophagus and esophageal adenocarcinoma in a European cohort". Clin Gastroenterol Hepatol. 12 (10): 1656–63.e1. doi:10.1016/j.cgh.2014.01.028. PMID 24480679.
- ↑ 8.0 8.1 Sun X, Chandar AK, Canto MI, Thota PN, Brock M, Shaheen NJ; et al. (2017). "Genomic regions associated with susceptibility to Barrett's esophagus and esophageal adenocarcinoma in African Americans: The cross BETRNet admixture study". PLoS One. 12 (10): e0184962. doi:10.1371/journal.pone.0184962. PMC 5657624. PMID 29073141.
- ↑ 9.0 9.1 Buas MF, He Q, Johnson LG, Onstad L, Levine DM, Thrift AP; et al. (2017). "Germline variation in inflammation-related pathways and risk of Barrett's oesophagus and oesophageal adenocarcinoma". Gut. 66 (10): 1739–1747. doi:10.1136/gutjnl-2016-311622. PMC 5296402. PMID 27486097.
- ↑ 10.0 10.1 10.2 Becker J, May A, Gerges C, Anders M, Schmidt C, Veits L; et al. (2016). "The Barrett-associated variants at GDF7 and TBX5 also increase esophageal adenocarcinoma risk". Cancer Med. 5 (5): 888–91. doi:10.1002/cam4.641. PMC 4864818. PMID 26783083.
- ↑ 11.0 11.1 11.2 Ek WE, Lagergren K, Cook M, Wu AH, Abnet CC, Levine D; et al. (2016). "Polymorphisms in genes in the androgen pathway and risk of Barrett's esophagus and esophageal adenocarcinoma". Int J Cancer. 138 (5): 1146–52. doi:10.1002/ijc.29863. PMC 4715576. PMID 26414697.
- ↑ 12.0 12.1 12.2 Schneider PM, Hölscher AH, Wegerer S, König U, Becker K, Siewert JR (1998). "[Clinical significance of p53 tumor suppressor gene mutations in adenocarcinoma in Barrett esophagus]". Langenbecks Arch Chir Suppl Kongressbd. 115 (Suppl I): 495–9. PMID 14518305.
- ↑ Spechler SJ. Barrett's esophagus. Semin Gastrointest Dis 1996; 7:51.
- ↑ 14.0 14.1 Spechler SJ (1996). "Barrett's esophagus". Semin Gastrointest Dis. 7 (2): 51–60. PMID 8705259.
- ↑ Lavy UI, Funcke AB, van Hell G, Timmerman H (1973). "Pharmacological properties of ((3alpha-tropanyl)oxy)-5H-benzo(4,5)cycloheptal(1,2-b)-pyridine hydrogen maleate (BS 7723)". Arzneimittelforschung. 23 (6): 854–8. PMID 4146903.
- ↑ 16.0 16.1 von Schrenck T (2000). "[Diagnosis of gastroesophageal reflux and Barrett esophagus]". Zentralbl Chir. 125 (5): 414–23. PMID 10929625.
- ↑ 17.0 17.1 Minacapelli CD, Bajpai M, Geng X, Cheng CL, Chouthai AA, Souza R; et al. (2017). "Barrett's metaplasia develops from cellular reprograming of esophageal squamous epithelium due to gastroesophageal reflux". Am J Physiol Gastrointest Liver Physiol. 312 (6): G615–G622. doi:10.1152/ajpgi.00268.2016. PMID 28336546.
- ↑ Wipff J, Allanore Y, Soussi F, Terris B, Abitbol V, Raymond J; et al. (2005). "Prevalence of Barrett's esophagus in systemic sclerosis". Arthritis Rheum. 52 (9): 2882–8. doi:10.1002/art.21261. PMID 16142744.
- ↑ Drahos J, Li L, Jick SS, Cook MB (2016). "Metabolic syndrome in relation to Barrett's esophagus and esophageal adenocarcinoma: Results from a large population-based case-control study in the Clinical Practice Research Datalink". Cancer Epidemiol. 42: 9–14. doi:10.1016/j.canep.2016.02.008. PMC 4899201. PMID 26972225.
- ↑ Drahos J, Ricker W, Parsons R, Pfeiffer RM, Warren JL, Cook MB (2015). "Metabolic syndrome increases risk of Barrett esophagus in the absence of gastroesophageal reflux: an analysis of SEER-Medicare Data". J Clin Gastroenterol. 49 (4): 282–8. doi:10.1097/MCG.0000000000000119. PMC 4176548. PMID 24671095.
- ↑ He Q, Li JD, Huang W, Zhu WC, Yang JQ (2016). "Metabolic syndrome is associated with increased risk of Barrett esophagus: A meta-analysis". Medicine (Baltimore). 95 (31): e4338. doi:10.1097/MD.0000000000004338. PMC 4979793. PMID 27495039.
- ↑ Booth CL, Thompson KS (2012). "Barrett's esophagus: A review of diagnostic criteria, clinical surveillance practices and new developments". J Gastrointest Oncol. 3 (3): 232–42. doi:10.3978/j.issn.2078-6891.2012.028. PMC 3418534. PMID 22943014.
- ↑ Paull A, Trier JS, Dalton MD, Camp RC, Loeb P, Goyal RK (1976). "The histologic spectrum of Barrett's esophagus". N Engl J Med. 295 (9): 476–80. doi:10.1056/NEJM197608262950904. PMID 940579.