Artificial heart valve: Difference between revisions
Esther Lee (talk | contribs) |
No edit summary |
||
| Line 149: | Line 149: | ||
* [http://www.ctsnet.org/medtronic/product/609 Medtronic] | * [http://www.ctsnet.org/medtronic/product/609 Medtronic] | ||
* [http://www.sjm.com/devices/devicetype.aspx?location=in&type=18 St. Jude] | * [http://www.sjm.com/devices/devicetype.aspx?location=in&type=18 St. Jude] | ||
==2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>== | |||
===Evaluation and Selection of Prosthetic Valves=== | |||
====Recommendations for Diagnosis and Follow up==== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.'''An initial [[TTE]] study is recommended in patients after prosthetic valve implantation for evaluation of valve hemodynamics. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B'']])<nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''2.'''Repeat [[TTE]] is recommended in patients with prosthetic heart valves if there is a change in clinical | |||
symptoms or signs suggesting valve dysfunction. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: C'']])<nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''3.'''[[TEE]] is recommended when clinical symptoms or signs suggest prosthetic valve dysfunction. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: C'']])<nowiki>"</nowiki> | |||
|- | |||
|} | |||
==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ||
Revision as of 03:05, 9 March 2014
| Artificial heart valve | |
 | |
|---|---|
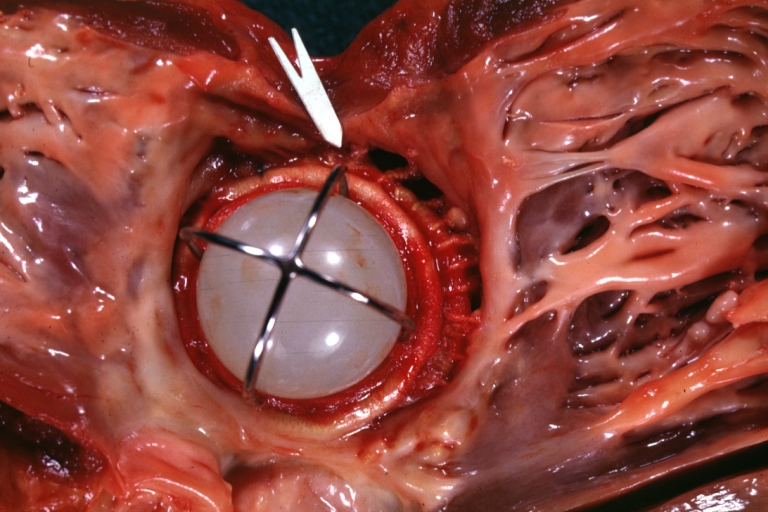
| Mitral Valve Prosthesis with Perivalvular Leak: Gross, natural color, close-up of valve with arrow to site of leakage, probably infected caged ball prosthesis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
An artificial heart valve is a device which is implanted in the heart of patients who suffer from valvular diseases in their heart. When one or two of the four heart valves of the heart have a malfunction, the choice is normally to replace the natural valve with an artificial valve. This requires open-heart surgery.
Valves are integral to the normal physiological functioning of the human heart. Natural heart valves are structures which have evolved a form which meets their functional requirements, which is to induce largely unidirectional flow through themselves. Natural heart valves may become dysfunctional due to a variety of pathological causes. Certain heart valve pathologies may necessitate the complete surgical replacement of the natural heart valves with heart valve prostheses.
Types of heart valve prostheses
There are two main types of artificial heart valves: the mechanical and the biological valves.
- Mechanical heart valves
- Percutaneous implantation
- Stent framed
- Not framed
- Sternotomy/Thoracotomy implantation
- Ball and cage
- Tilting disk
- Bi-leaflet
- Tri-leaflet
- Percutaneous implantation
Mechanical valves
Mechanical heart valves are prosthetics designed to replicate the function of the natural valves of the human heart. The human heart contains four valves: tricuspid valve, pulmonic valve, mitral valve and aortic valve. Their main purpose is to maintain unimpeded forward flow through the heart and from the heart into the major blood vessels connected to the heart, the pulmonary artery and the aorta. As a result of a number of disease processes, both acquired and congenital, any one of the four heart valves may malfunction and result in either stenosis (impeded forward flow) and/or backward flow (regurgitation). Either process burdens the heart and may lead to serious problems including heart failure. A mechanical heart valve is intended to replace a diseased heart valve with its prosthetic equivalent.
There are two basic types of valves that can be used for aortic valve replacement, mechanical and tissue valves. Modern mechanical valves can last indefinitely (the equivalent of over 50,000 years in an accelerated valve wear tester). However, current mechanical heart valves all require lifelong treatment with a blood thinner, e.g. warfarin, which requires monthly blood tests to monitor. This process of thinning the blood is called anticoagulation. Tissue heart valves, in contrast, do not require the use of anticoagulant drugs due to the improved blood flow dynamics resulting in less red cell damage and hence less clot formation. Their main weakness however, is their limited lifespan. Traditional tissue valves, made of pig heart valves, will last on average 15 years before they require replacement. (Studies as of November 2006 suggest that they may last longer in recipients under 50, refuting previous understanding)
Types of MHV's
There are three major types of mechanical valves - caged-ball, tilting-disk and bileaflet - with many modifications on these designs.
The first artificial heart valve was the caged-ball, which utilizes a metal cage to house a metal ball. When blood pressure in the chamber of the heart exceeds that of the pressure on the outside of the chamber the ball is pushed against the cage and allows blood to flow. At the completion of the heart's contraction, the pressure inside the chamber drops and is lower than beyond the valve, so the ball moves back against the base of the valve forming a seal. In 1952, Dr. Charles Hufnagel implanted caged-ball heart valves in ten patients (six survived the operation), marking the first long-term success in prosthetic heart valves. A similar valve was invented by Miles "Lowell" Edwards and Albert Starr in 1960 (commonly referred to as the Starr-Edwards Silastic Ball Valve). The first human implant was on Sept 21, 1960. It consisted of a silicone ball enclosed in a cage formed by wires originating from the valve housing. Caged ball valves have a high tendency to forming blood clots, so the patient must have a high degree of anti-coagulation, usually with a target INR of 2.5-3.5. Edwards Lifesciences discontinued production of the Starr-Edwards valve in 2007.
Soon after came tilting-disc valves, which have a single circular occluder controlled by a metal strut. They are made of a metal ring covered by a tissue, into which the suture threads are stitched in order to hold the valve in place. The metal ring holds, by means of two metal supports, a disc which opens and closes as the heart pumps blood through the valve. The disc is usually made of an extremely hard carbon material (pyrolytic carbon), in order to allow the valve to function for years without wearing out. The Medtronic-Hall model is the most common tilting-disc design in the US. In some models of mechanical valves, the disc is divided into two parts, which open and close as a door.
St. Jude Medical is the leader in bileaflet valves, which consist of two semicircular leaflets that rotate about struts attached to the valve housing. This design was introduced in 1979 and while they take care of some of the issues that were seen in the other models, bileaflets are vulnerable to backflow and so it cannot be considered as ideal. Bileaflet valves do, however, provide much more natural blood flow than caged-ball or tilting-disc implants. One of the main advantages of these valves is that they are well tolerated by the body. Only a small amount of blood thinner is needed to be taken by the patient each day in order to prevent clotting of the blood when flowing through the valve.
These bileaflet valves have the advantage that they have a greater effective opening area (2.4-3.2 square cm c.f. 1.5-2.1 for the single-leaflet valves). Also, they are the least thrombogenic of the artificial valves.
Mechanical heart valves are today very reliable and allow the patient to live a normal life. Most mechanical valves last for at least 20 to 30 years.
Durability
Mechanical heart valves are considered to be extremely durable in comparison to their bioprosthetic counterparts. The struts and occluders are made out of either pyrolytic carbon or titanium coated with pyrolytic carbon, and the sewing ring cuff is Teflon, polyester or dacron. The major load arises from transvalvular pressure generated at and after valve closure, and in cases where structural failure does happen, it is usually as a result of occluder impact on the components.
Impact wear and friction wear dictate the loss of material in MHV’s. Impact wear usually occurs in the hinge regions of bileaflets, between the occluder and ring in tilting-discs, and between the ball and cage in caged-ball valves. Friction wear occurs between the occluder and strut in tilting-discs, and between the leaflet pivots and hinge cavities in bileaflets.
MHV’s made out of metal are also susceptible to fatigue failure owing to the polycrystalline characteristic of metals, but this is not an issue with pyrolytic carbon MHV’s because this material is not crystalline in nature.
Cavitation should also be considered when studying degradation of MHV’s.
Fluid mechanics
Many of the complications associated with MHV’s can be explained through fluid mechanics. For example, thrombus formation is a debilitating side effect of high shear stresses created by the design of the valves. An ideal heart valve from an engineering perspective would produce minimal pressure drops, have small regurgitation volumes, minimize turbulence, reduce prevalence of high stresses, and not create flow separations in the vicinity of the valve.
One measure of the quality of a valve is the effective orifice area (EOA), which can be calculated as follows:
<math>EOA(\mathrm{cm}^2) = \frac{Q_{rms}}{51.6\sqrt{\Delta p}}\ </math>
where <math>Q_{rms}</math> is the root mean square systolic/diastolic flow rate (cm³/s) and <math>\Delta p</math> is the mean systolic/diastolic pressure drop (mmHg). This is a measure of how much the prosthesis impedes blood flow through the valve. A higher EOA corresponds to a smaller energy loss. The performance index (PI) normalizes the EOA by valve size and is a size-independent measure of the valve’s resistance characteristics. Bileaflet valves typically have higher PI’s than tilted-disc models, which in turn have higher PI’s than caged-ball models.
As blood flows through a prosthetic heart valve, a sudden pressure drop occurs across the valve due to the reduction in cross-sectional area within the valve housing. This can be quantified through the continuity equation and Bernoulli’s equation:
<math>A_1V_1 = A_2V_2</math>
<math>P_1 + \frac{1}{2} \rho _1 V_1^2 = P_2 + \frac{1}{2} \rho_2 V_2^2</math>
where A represents the cross-sectional area, P is pressure, <math>\rho</math> is density, and V is the velocity. As cross-sectional area decreases in the valve, velocity increases and pressure drops as a result. This effect is more dramatic in caged-ball valves than in tilting-disc and bileaflet valves. A larger systolic pressure is required to drive flow forward in order to compensate for a large pressure drop, so it should be minimized.
Regurgitation is the sum of retrograde flow during the closing motion of the valve and leakage flow after closure. It is directly proportional to valve size and is also dependent on valve type. Typically, caged-ball valves have a low amount of regurgitation as there is very little leakage. Tilting-disc and bileaflet valves are comparable, with the bileaflet valves have a slightly larger regurgitation volume. Bioprosthetics prevail over MHV’s in this case, as they have virtually no regurgitation volume.
Turbulence and high shear stresses are also major issues with MHV’s, as they can fracture the valve housing or components, or induce blood damage. A large flow gradient can lead to these factors, so flow separation and stagnation should be as small as possible. High stresses are created at the edges of the annular jet in caged-ball valves, in narrow regions at the edges of the major orifice jet in tilting-disc valves, and in regions immediately distal to the valve leaflets in bileaflet valves. The implications of blood damage from these stresses are discussed in the next section.
The cavitation phenomenon can also be described using fluid mechanics. This can result from pressure oscillations, flow deceleration, tip cortices, streamline contraction, and squeeze jets [4]. This last cause is the most contributive factor to cavitation. The squeeze jets are formed when the valve is closing and the blood between the occluder and valve housing is “squeezed” out to create a high-speed jet. This in turn creates intense vortices with very low pressures that can lead to cavitation.
Blood damage
One of the major drawbacks of mechanical heart valves is that patients with these implants require consistent anti-coagulation therapy. Clots formed by red blood cell (RBC) and platelet damage can block up blood vessels and lead to very serious consequences. Clotting occurs in one of three basic pathways: tissue factor exposure, platelet activation, or contact activation by foreign materials, and in three steps: initiation, amplification, and propagation.
In the tissue factor exposure path, initiation begins when cells are ruptured and expose tissue factor (TF). Plasma Factor (f) VII binds to TF and sets off a chain reaction which activates fXa and fVa which bind to each other to produce thrombin which in turn activates platelets and fVIII. The platelets activate by binding to the damaged tissue in the initiation phase, and fibrin stabilizes the clot during the propagation phase.
The platelet activation pathway is triggered when stresses reach a level above 6 to 8 Pa (60–80 dyn/cm²). The steps involved with this are less clearly understood, but initiation begins with the binding of vWF from the plasma to GPIb on the platelet. This is followed by a large influx of Ca2+ ions, which activates the platelets. GPIIb-IIIa facilitates platelet-platelet adhesion during amplification. The propagation step is still under study.
Contact activation begins when fXII binds to a negatively charged surface. This in turn activates prekallikrein (PK) and high-molecular-weight kininogen (HK). Eventually, HKa-PK and HKa-fXI complexes form on the surface. In amplification, Hka-FXIa complexes activate fIX to fIXa, which in turn forms thrombin and platelets. Proteins buildup on the surface and facilitate platelet adhesion and tissue growth in the propagation stage.
All MHV models are vulnerable to thrombus formation due to high shear stress, stagnation, and flow separation. The caged-ball designs experience high stresses at the walls that can damage cells, as well as flow separation due to high-velocity reverse flow surrounded by stagnant flow. Tilting-disc valves have flow separation behind the valve struts and disc as a result of a combination of high velocity and stagnant flows. The bileaflet models have high stresses during forward and leakage flows as well as adjacent stagnant flow in the hinge area. As it turns out, the hinge area is the most critical part of bileaflets and is where the thrombus formation is usually prevalent.
In general, blood damage affects valves in both the mitral and aortic positions. High stresses during leakage flow in aortal valves result from higher transvalvular pressures, and high stresses occur during forward flow for mitral valves. Valvular thrombosis is most common in mitral prosthetics. The caged-ball model is better than the other two models in terms of controlling this problem, because it is at a lower risk for thrombosis and it is gradual when it does happen. The bileaflet is more adaptable to this problem than the tilting-disc model because if one leaflet stops working, the other can still function. However, if the hinge is blocked, both leaflets will stop functioning.
Because all models experience high stresses, patients with mechanical heart valve implants require anti-coagulation therapy. Bioprosthetics are less prone to develop blood clotting, but the trade-off concerning durability generally favors their use in patients older than age 55.
Mechanical heart valves can also cause hemolytic anemia with hemolysis of the red blood cells as they pass through the valve.
Biological valves
Biological valves are valves of animals, like pigs, which undergo several chemical procedures in order to make them suitable for implantation in the human heart. The porcine (or pig) heart is most similar to the human heart, and therefore represents the best anatomical fit for replacement. Implantation of a porcine valve is a type of Xenotransplantation, or Xenograft, which means a transplant from one species (in this case a pig) to another. There are some risks associated with a Xenograft such as the human body's tendency to reject foreign material. Medication can be used to retard this effect, but is not always successful.
Another type of biological valve utilizes biological tissue to make leaflets that are sewn into a metal frame. This tissue is typically harvested from the Pericardial Sac of either Bovine (cows) or Equine (horses). The pericardial sac is particularly well suited for a valve leaflet due to its extremely durable physical properties. This type of biological valve is extremely effective means of valve replacement. The tissue is sterilized so that the biological markers are removed, eliminating a response from the host's immune system. The leaflets are flexible and durable and do not require the patient to take blood thinners for the rest of their life.
The most used heart valves in the US and EU are those utilizing tissue leaflets. Mechanical valves are more commonly used in Asia and Latin America. The following companies manufacture tissue heart valves: Edwards Lifesciences, Medtronic, St. Jude Medical, Sorin, ATS, 3F, and CryoLife.
Functional requirements of heart valve prostheses
The functioning of natural heart valves is characterised by many advantages:
- Minimal regurgitation - This means that the amount of blood lost upstream as the valve closes is small. For example, closure regurgitation through the mitral valve would result in some blood loss from the left ventricle to the left atrium as the mitral valve closes. Some degree of valvular regurgitation is inevitable and natural (Fixme: Give indicative value). However, several heart valve pathologies (e.g. rheumatic endocarditis) may lead to clinically significant valvular regurgitation. A desirable characteristic of heart valve prostheses is that regurgitation is minimal over the full range of physiological heart function (i.e. complete functional envelope of cardiac output vs. heart rate).
- Minimal transvalvular pressure gradient - Whenever a fluid flows through a restriction, such as a valve, a pressure gradient arises over the restriction. This pressure gradient is a result of the increased resistance to flow through the restriction. Natural heart valves have a low transvalvular pressure gradient as they present little obstruction to the flow through themselves (Fixme: Give indicative value). A desirable characteristic of heart valve prostheses is that their transvalvular pressure gradient is as small as possible.
- Non-thrombogenic - As natural heart valves are lined with an endothelium continuous with the endothelium lining the heart chambers they are not normally thrombogenic. This is important as should thrombus form on the heart valve leaflets and become seeded with bacteria, so called "bacterial vegetations" will form. Such vegetations are difficult for the body to deal with as the normal physiological defense mechanisms are not present within the valve leaflets because they are avascular and largely composed of connective tissue (Fixme: Create article discussing the pathgonesis of leaflet bacterial vegetations.). Should bacterial vegetations form on the valve leafets they may continually seed bacteria into the arterial tree which may lead to bacteremia or septicaemia. Portions of the vegetation may also break off forming septic emboli. Septic emboli can lodge anywhere in the arterial tree (e.g. brain, bowel, lungs) causing local infectious foci. Even dislodged fragments from non-infectious vegetations (Fixme: Is this the correct terminology?) can be hazardous as they can lodge in, and block, downstream arteries (e.g. coronary arteries leading to myocardial infarction, cerebral arteries leading to stroke). A desirable characteristic of heart valve prostheses is that they are non or minimally thrombogenic.
- Self-repairing - Although of limited extent compared to well vascularised tissue (e.g. muscle), the valve leaflets do retain some capacity for repair due to the presence of regenerative cells (e.g. fibroblasts) in the connective tissue from which the leaflets are composed. As the human heart beats approximately 3.4x109 times during a typical human lifespan this limited but nevertheless present repair capacity is critically important. No heart valve prostheses can currently self-repair but replacement tissues grown using stem cell technology may eventually offer such capabilities. (State that they wear).
- Rapid dynamic response - STD
Design challenges of heart valve prostheses
- Thrombogenesis / haemocompatibility
- Mechanisms:
- Forward and backward flow shear
- Static leakage shear
- Presence of foreign material (i.e. intrinsic coagulation cascade)
- Cellular maceration
- Mechanisms:
- Valve-tissue interaction
- Wear
- Blockage
- Getting stuck
- Dynamic responsiveness
- Failure safety
- Valve orifice to anatomical orifice ratio
- Trans-valvular pressure gradient
- Minimal leakages
Typical configuration of a heart valve prosthesis
- Anchor
- Leaflets
MHV manufacturers
Companies that manufacture MHVs include:
- ATS Medical, Inc.
- CarboMedics
- Edwards Lifesciences (formerly Baxter-Edwards Critical Care)
- Medtronic
- St. Jude
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary[1]
Evaluation and Selection of Prosthetic Valves
Recommendations for Diagnosis and Follow up
| Class I |
| "1.An initial TTE study is recommended in patients after prosthetic valve implantation for evaluation of valve hemodynamics. (Level of Evidence: B)" |
| "2.Repeat TTE is recommended in patients with prosthetic heart valves if there is a change in clinical
symptoms or signs suggesting valve dysfunction. (Level of Evidence: C)" |
| "3.TEE is recommended when clinical symptoms or signs suggest prosthetic valve dysfunction. (Level of Evidence: C)" |
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [2]
Antithrombotic Therapy for Prosthetic Heart Valves (DO NOT EDIT) [2]
| Class I |
| "1. After AVR with bileaflet mechanical or Medtronic Hall prostheses, in patients with no risk factors,* warfarin is indicated to achieve an INR of 2.0 to 3.0. If the patient has risk factors, warfarin is indicated to achieve an INR of 2.5 to 3.5. (Level of Evidence: B)" |
| "2. After AVR with Starr-Edwards valves or mechanical disc valves (other than Medtronic Hall prostheses), in patients with no risk factors,* warfarin is indicated to achieve an INR of 2.5 to 3.5. (Level of Evidence: B)" |
| "3. After mitral valve replacement with any mechanical valve, warfarin is indicated to achieve an INR of 2.5 to 3.5. (Level of Evidence: C)" |
| "4. After AVR or MV replacement with a bioprosthesis and no risk factors,* aspirin is indicated at 75 to 100 mg per day. (Level of Evidence: C)" |
| "5. After AVR with a bioprosthesis and risk factors,* warfarin is indicated to achieve an INR of 2.0 to 3.0. (Level of Evidence: C)" |
| "6. After MV replacement with a bioprosthesis and risk factors,* warfarin is indicated to achieve an INR of 2.0 to 3.0. (Level of Evidence: C)" |
| "7. For those patients who are unable to take warfarin after MV replacement or AVR, aspirin is indicated in a dose of 75 to 325mg per day. (Level of Evidence: Level B)" |
| "8. The addition of aspirin 75 to 100 mg once daily to therapeutic warfarin is recommended for all patients with mechanical heart valves and those patients with biological valves who have risk factors.* (Level of Evidence: B)" |
| Class IIa |
| "1. During the first 3 months after AVR or MV replacement with a bioprosthesis, in patients with no risk factors,* it is reasonable to give warfarin to achieve an INR of 2.0 to 3.0. (Level of Evidence: C)" |
| "2. In high-risk patients with prosthetic heart valves in whom aspirin cannot be used, it may be reasonable to give clopidogrel (75 mg per day) or warfarin to achieve an INR of 3.5 to 4.5. (Level of Evidence: C)" |
| “ |
* Risk factors include atrial fibrillation, previous thromboembolism, LV dysfunction, and hypercoagulable condition. |
” |
Bridging Therapy in Patients With Mechanical Valves (DO NOT EDIT) [3]
| Class I |
| "1. In patients at low risk of thrombosis, defined as those with a bileaflet mechanical AVR with no risk factors,* it is recommended that warfarin be stopped 48 to 72 h before the procedure (so the INR falls to less than 1.5) and restarted within 24 h after the procedure. Heparin is usually unnecessary. (Level of Evidence B)" |
| "2. In patients at high risk of thrombosis, defined as those with any mechanical MV replacement or a mechanical AVR with any risk factor, therapeutic doses of intravenous UFH should be started when the INR falls below 2.0 (typically 48 h before surgery), stopped 4 to 6 h before the procedure, restarted as early after surgery as bleeding stability allows, and continued until the INR is again therapeutic with warfarin therapy. (Level of Evidence: B)" |
| Class III |
| "1. In patients with mechanical valves who require interruption of warfarin therapy for noncardiac surgery, invasive procedures, or dental care, high-dose vitamin K1 should not be given routinely, because this may create a hypercoagulable condition. (Level of Evidence: B)" |
| Class IIa |
| "1. It is reasonable to give fresh frozen plasma to patients with mechanical valves who require interruption of warfarin therapy for emergency noncardiac surgery, invasive procedures, or dental care. Fresh frozen plasma is preferable to high-dose vitamin K1. (Level of Evidence: B)" |
| Class IIb |
| "1. In patients at high risk of thrombosis, therapeutic doses of subcutaneous UFH (15 000 U every 12 h) or LMWH (100 U per kg every 12 h) may be considered during the period of a subtherapeutic INR. (Level of Evidence: B)" |
| “ | * Risk factors: atrial fibrillation, previous thromboembolism, LV dysfunction, hypercoagulable conditions, older-generation thrombogenic valves, mechanical tricuspid valves, or more than 1 mechanical valve | ” |
Thrombosis of Prosthetic Heart Valves (DO NOT EDIT) [3]
| Class I |
| "1. Transthoracic and Doppler echocardiography is indicated in patients with suspected prosthetic valve thrombosis to assess hemodynamic severity. (Level of Evidence: B)" |
| "2. Transesophageal echocardiography and/or fluoroscopy is indicated in patients with suspected valve thrombosis to assess valve motion and clot burden. (Level of Evidence: B)" |
| Class IIa |
| "1. Emergency operation is reasonable for patients with a thrombosed left-sided prosthetic valve and NYHA functional class III–IV symptoms. (Level of Evidence: C)" |
| "2. Emergency operation is reasonable for patients with a thrombosed left-sided prosthetic valve and a large clot burden. (Level of Evidence: C)" |
| "3. Fibrinolytic therapy is reasonable for thrombosed right-sided prosthetic heart valves with NYHA functional class III–IV symptoms or a large clot burden. (Level of Evidence: C)" |
| Class IIb |
| "1. Fibrinolytic therapy may be considered as a first-line therapy for patients with a thrombosed left-sided prosthetic valve, NYHA functional class I–II symptoms, and a small clot burden. (Level of Evidence: B)" |
| "2. Fibrinolytic therapy may be considered as a first-line therapy for patients with a thrombosed left-sided prosthetic valve, NYHA functional class III–IV symptoms, and a small clot burden if surgery is high risk or not available. (Level of Evidence: B)" |
| "3. Fibrinolytic therapy may be considered for patients with an obstructed, thrombosed left-sided prosthetic valve who have NYHA functional class II–IV symptoms and a large clot burden if emergency surgery is high risk or not available. . (Level of Evidence: C)" |
| "4. Intravenous UFH as an alternative to fibrinolytic therapy may be considered for patients with a thrombosed valve who are in NYHA functional class I–II and have a small clot burden. (Level of Evidence: C)" |
Follow-up Visits (DO NOT EDIT) [3]
| Class I |
| "1. For patients with prosthetic heart valves, a history, physical examination, and appropriate tests should be performed at the first postoperative outpatient evaluation, 2 to 4 weeks after hospital discharge. This should include a transthoracic Doppler echocardiogram if a baseline echocardiogram was not obtained before hospital discharge. (Level of evidence C)" |
| "2. For patients with prosthetic heart valves, routine follow-up visits should be conducted annually, with earlier re-evaluations (with echocardiography) if there is a change in clinical status. (Level of evidence C)" |
| Class III |
| "1. Routine annual echocardiograms are not indicated in the absence of a change in clinical status in patients with mechanical heart valves or during the first 5 years after valve replacement with a bioprosthetic valve. (Level of evidence C)" |
| Class IIb |
| "1. Patients with bioprosthetic valves may be considered for annual echocardiograms after the first 5 years in the absence of a change in clinical status. (Level of evidence C)" |
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [2]
References
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ 2.0 2.1 2.2 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 3.2 Bonow RO, Carabello BA, Kanu C; et al. (2006). "ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons". Circulation. 114 (5): e84–231. doi:10.1161/CIRCULATIONAHA.106.176857. PMID 16880336. Unknown parameter
|month=ignored (help)
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion: safety of Lovenox in pregnancy. Obstet Gynecol. Oct 2002;100(4):845-6.
- Baddour LM, Wilson WR, Bayer AS. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications. Circulation. Jun 14 2005;111(23):e394-434.
- Bettadapur MS. Caring for patients with prosthetic heart valves. Cleveland Clinic Journal of Medicine 69 (1), 75-87.
- Bloomfield P (2002). Choice of heart valve prosthesis. Heart,87, 583-589.
- Bonow et al (1998). Management of patients with prosthetic heart valves. JACC 32(5), 1555-1565.
- Bussey HI. An overview of anticoagulants, antiplatelet agents, and the combination in patients with mechanical heart valves. J Heart Valve Dis. May 2004;13(3):319-24.
- Butany J, Ahluwalia MS, Munroe C, et al. prostheses: identification and evaluation (erratum). Cardiovasc Pathol. Nov-Dec 2003;12(6):322-44.
- Butany J, Fayet C, Ahluwalia MS, et al. Biological replacement heart valves. Identification and evaluation. Cardiovasc Pathol. May-Jun 2003;12(3):119-39.
- Cannegieter SC, Rosendaal FR, Briet E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation. Feb 1994;89(2):635-41.
- Crawford MH (2002). The patient with prosthetic heart valves. In: Evaluation of the patient with heart disease. Integrating the physical exam & echocardiography. Eds: Roldan CA, Abrams J. Lippincott Williams & Wilkins, Philadelphia,USA, pp 251-262.
- Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. Circulation. Jul 1 1997;96(1):358-66.
- David TE, Puschmann R, Ivanov J, et al (1998). Aortic valve replacement with stentless and stented porcine valves: a case-match study. J Thorac Cardiovasc Surg, 116, 236-41.
- Garcia MJ (2002). Prosthetic valve disease. In: Textbook of Cardiovascular Medicine. 2nd Ed. Topol EJ. Lippincott-Raven, Philadelphia, USA, pp 549-68.
- Goldman ME. Echocardiographic doppler evaluation of prosthetic valve function and dysfunction. Adv Cardiol. 2004;41:179-84.
- Grunkemeier GL, Starr A, Rahimtoola SH (2001). Clinical performance of prosthethic heart valves. In: Hurst's The Heart. 10th ed. Eds: Fuster V, Alexander RW, O'Rourke RA. The McGraw-Hill Companies, USA, pp 1759-1782.
- Hung L, Rahimtoola SH (2003). Prosthetic heart valves and pregnancy. Circulation, 107, 1240-1246.
- Jamieson WR, Marchand MA, Pelletier CL, et al (1999). Structural valve deterioration in mitral replacement surgery: Comparison of carpentier-Edwards supra-anular porcine and perimount pericardial bioprostheses. J Thorac Cardiovasc Surg, 118, 297-304.
- Kahn S. Long-term outcomes with mechanical and tissue valves. J Heart Valve Dis. 2002;11, Suppl 1:S8-S14.
- Lengyel M, Fuster V, Keltai M, et al. Guidelines for management of left-sided prosthetic valve thrombosis: a role for thrombolytic therapy. Consensus Conference on Prosthetic Valve Thrombosis. J Am Coll Cardiol. Nov 15 1997; 30(6): 1521-6.
- MacKenzie GS, Heinle SK. Echocardiography and Doppler assessment of prosthetic heart valves with transesophageal echocardiography. Crit Care Clin. Apr 1996;12(2):383-409.
- Mehlman DJ. A pictorial and radiographic guide for identification of prosthetic heart valve devices. Prog Cardiovasc Dis. May-Jun 1988;30(6):441-64.
- Piper C, Kprfer R, Horstkotte D. Prosthetic valve endocarditis. Heart. May 2001;85(5):590-3.
- Roudaut R, Lafitte S, Roudaut MF, et al. Fibrinolysis of mechanical prosthetic valve thrombosis: a single-center study of 127 cases. J Am Coll Cardiol. Feb 19 2003;41(4):653-8.
- Stein PD, Alpert JS, Bussey HI, et al. Antithrombotic therapy in patients with mechanical and biological prosthetic heart valves. Chest. Jan 2001;119(1 Suppl):220S-227S.
- Vongpatanasin W, Hillis LD, Lange RA. Prosthetic heart valves. N Engl J Med. Aug 8 1996;335(6):407-16.