Anaplastic large cell lymphoma pathophysiology: Difference between revisions
No edit summary |
|||
| Line 32: | Line 32: | ||
[[Category:Hematology]] | [[Category:Hematology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Needs overview]] | [[Category:Needs overview]] | ||
Revision as of 17:17, 14 August 2015
|
Anaplastic large cell lymphoma Microchapters |
|
Differentiating Anaplastic large cell lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Anaplastic large cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Anaplastic large cell lymphoma pathophysiology |
|
Directions to Hospitals Treating Anaplastic large cell lymphoma |
|
Risk calculators and risk factors for Anaplastic large cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Pathophysiology
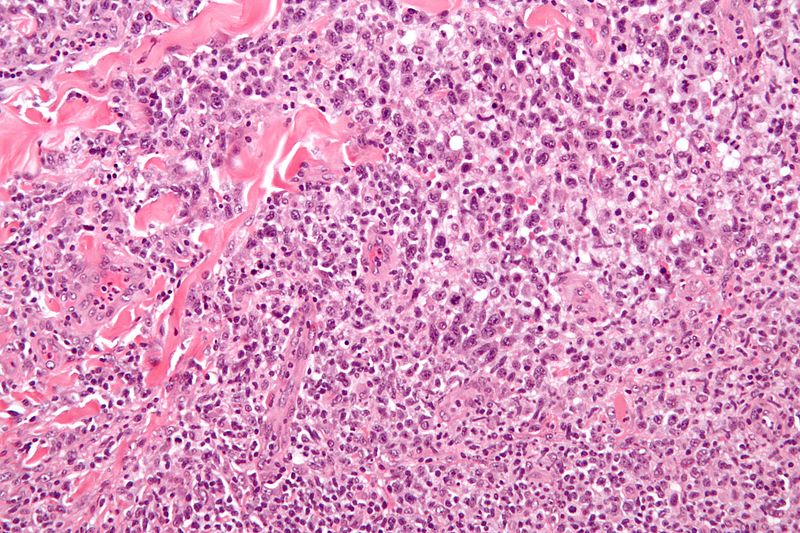
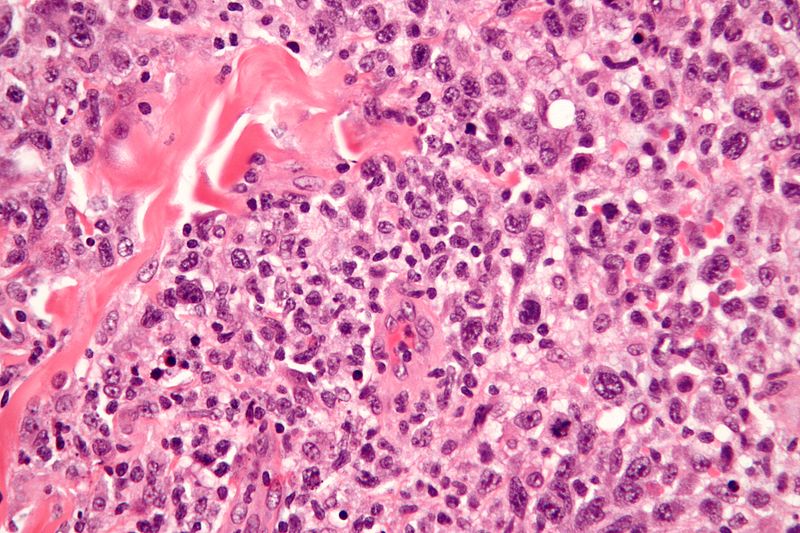
Microscopic Pathology
By definition, on histological examination, hallmark cells are always present. Where they are not present in large numbers, they are usually located around blood vessels. Morphologic variants include the following types:
- Common (featuring a predominance of hallmark cells)
- Small cell (featuring smaller cells with the same immunophenotype as the hallmark cells)
- Lymphohistiocytic
- Sarcomatoid
- Signet ring
The hallmark cells are of medium size and feature abundant cytoplasm (which may be clear, amphophilic or eosinophilic), kidney shaped nuclei, and a paranuclear eosinophilic region. Occasional cells may be identified in which the plane of section passes through the nucleus in such a way that it appears to enclose a region of cytoplasm within a ring; such cells are called "doughnut" cells.
Video
{{#ev:youtube|3-ajNCAGP4Y}}
Molecular Biology
The majority of cases, greater than 90%, contain a clonal rearrangement of the T-cell receptor. This may be identified using PCR techniques, such as T-gamma multiplex PCR. Oncogenetic potential is conferred by upregulation of a tyrosine kinase gene on chromosome 2. Several different translocations involving this gene have been identified in different cases of this lymphoma. The most common is a chromosomal translocation involving the nucleophosmin gene on chromosome 5. The translocation may be identified by analysis of giemsa-banded metaphase spreads of tumour cells and is characterised by t(2;5)(p23;q35). The product of this fusion gene may be identified by immunohistochemistry using antiserum to ALK protein. Probes are available to identify the translocation by fluorescent in situ hybridization. The nucleophosmin component associated with the commonest translocation results in nuclear positivity as well as cytoplasmic positivity. Positivity with the other translocations may be confined to the cytoplasm.
Immunophenotype
The hallmark cells (and variants) show immunopositivity for CD30 (also known as Ki-1). True positivity requires localisation of signal to the cell membrane and/or paranuclear region (cyptolasmic positivity is considered non-specific and non-informative). Another useful marker which helps to differentiate this lesion from Hodgkin lymphoma is Clusterin. The neoplastic cells have a golgi staining pattern (hence paranuclear staining), which is characteristic of this lymphoma. The cells are also typically positive for a subset of markers of T-cell lineage. However, as with other T-cell lymphomas, they are usually negative for the pan T-cell marker CD3. Occasional examples are of null (neither T nor B) cell type. These lymphomas show immunopositivity for ALK protein in 70% of cases. They are also typically positive for EMA. In contrast to many B-cell anaplastic CD30 positive lymphomas, they are negative for markers of Epstein-Barr Virus (EBV).