Abdominal pain differential diagnosis
| <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline> |
Resident Survival Guide |
|
Abdominal pain Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Abdominal pain On the Web |
|
American Roentgen Ray Society Images of Abdominal pain |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]Amandeep Singh M.D.[3]
Overview
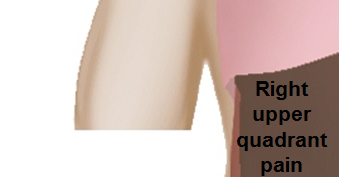
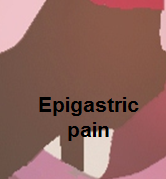
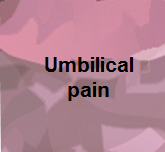
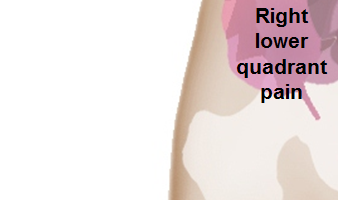
Diagnosing the cause of abdominal pain can be difficult, because many diseases can cause this symptom. Most frequently the cause is benign and/or self-limiting, but more serious causes may require urgent intervention. Acute abdominal pain is a severe, persistent abdominal pain of sudden onset that is likely to require surgical intervention to treat its cause. The following table summarizes differential diagnosis for abdominal pain.
Differential diagnosis of abdominal pain
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
 |

|
 |
 |

|
 |
 |

|
The following is a list of diseases that present with acute onset severe lower abdominal pain:
| Disease | Findings |
|---|---|
| Ectopic pregnancy | History of missed menses, positive pregnancy test, ultrasound reveals an empty uterus and may show a mass in the fallopian tubes.[1] |
| Appendicitis | Pain localized to the right iliac fossa, vomiting, abdominal ultrasound sensitivity for diagnosis of acute appendicitis is 75% to 90%.[2] |
| Rupturedovarian cyst | Usually spontaneous, can follow history of trauma, mild chronic lower abdominal discomfort may suddenly intensify, ultrasound is diagnostic.[3] |
| Ovarian cyst torsion | Presents with acute severe unilateral lower quadrant abdominal pain, nausea and vomiting, tender adnexal mass palpated in 90%, ultrasound is diagnostic.[4] |
| Hemorrhagic ovarian cyst | Presents with localized abdominal pain, nausea and vomiting. Hypovolemic shock may be present, abdominal tenderness and guarding are physical exam findings, ultrasound is diagnostic.[4] |
| Endometriosis | Presents with cyclic pain that is exacerbated by onset of menses, dyspareunia. laparoscopic exploration is diagnostic.[4] |
| Acute cystitis | Presents with features of increased urinary frequency, urgency, dysuria, and suprapubic pain.[5][6] |
References
- ↑ Morin L, Cargill YM, Glanc P (2016). "Ultrasound Evaluation of First Trimester Complications of Pregnancy". J Obstet Gynaecol Can. 38 (10): 982–988. doi:10.1016/j.jogc.2016.06.001. PMID 27720100.
- ↑ Balthazar EJ, Birnbaum BA, Yee J, Megibow AJ, Roshkow J, Gray C (1994). "Acute appendicitis: CT and US correlation in 100 patients". Radiology. 190 (1): 31–5. doi:10.1148/radiology.190.1.8259423. PMID 8259423.
- ↑ Bottomley C, Bourne T (2009). "Diagnosis and management of ovarian cyst accidents". Best Pract Res Clin Obstet Gynaecol. 23 (5): 711–24. doi:10.1016/j.bpobgyn.2009.02.001. PMID 19299205.
- ↑ 4.0 4.1 4.2 Bhavsar AK, Gelner EJ, Shorma T (2016). "Common Questions About the Evaluation of Acute Pelvic Pain". Am Fam Physician. 93 (1): 41–8. PMID 26760839.
- ↑ {{Cite journal | author = W. E. Stamm | title = Etiology and management of the acute urethral syndrome | journal = Sexually transmitted diseases | volume = 8 | issue = 3 | pages = 235–238 | year = 1981 | month = July-September | pmid = 7292216
- ↑ {{Cite journal | author = W. E. Stamm, K. F. Wagner, R. Amsel, E. R. Alexander, M. Turck, G. W. Counts & K. K. Holmes | title = Causes of the acute urethral syndrome in women | journal = The New England journal of medicine | volume = 303 | issue = 8 | pages = 409–415 | year = 1980 | month = August | doi = 10.1056/NEJM198008213030801 | pmid = 6993946