Whipworm infection pathophysiology
|
Whipworm infection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Whipworm infection pathophysiology On the Web |
|
American Roentgen Ray Society Images of Whipworm infection pathophysiology |
|
Risk calculators and risk factors for Whipworm infection pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2], Syed Hassan A. Kazmi BSc, MD [3]
Overview
Infection is acquired by the ingestion of embryonated eggs from contaminated drinking water and food. Once the eggs are ingested, they hatch in the small intestine then, larvae enter the intestinal crypts. The larvae migrate to the proximal colon and mature into adult worms. The females begin to oviposit 60 to 70 days after infection and shed between 3,000 and 20,000 eggs per day. Whipworm causes disease by colonic mucosal invasion by the adult worms and resulting in inflammation of the colonic mucosa.
Pathophysiology
Life Cycle
1. The eggs develop into a 2-cell stage.
2. The two cell stage then leads to an advanced cleavage stage.
3. The eggs embryonate.
4. Eggs become infective in 15 to 30 days.
5. Mature adult worms travel in the colon.
6. The adult worms (approximately 4 cm in length) live in the cecum and ascending colon. The life span of the adult worm is approximately 1 year.
Transmission
- Whipworm infection is acquired by the ingestion of embryonated eggs from contaminated drinking water and food.
Pathogenesis
- The eggs once ingested hatch in the small intestine, and the larvae enter the intestinal crypts.[1][2]
- The larve migrate to the proximal colon and mature into adult worms.
- The adult worms live in the cecum and ascending colon and attach themselves to the colonic mucosa with the anterior portions threaded into the mucosa.
- The females begin to oviposit 60 to 70 days after infection and shed between 3,000 and 20,000 eggs per day.
- Whipworm causes disease by colonic mucosal invasion of the adult worms and resulting in inflammation of the colonic mucosa.[3]
Molecular pathology
| Secreted molecules by whipworm | Role in pathogenesis |
| Trichuris trichiura 47 (TT47) | Forms pores in caecal epithelial cells, allowing parasite to keep anterior end in syncytial environment[4] |
| Excretory secretory products (ES products) | Promote Th2/Treg response that decreases intestinal inflammation[5] |
| Trichinella spiralis macrophage inhibitory factor (TsMIF) | Inhibits migration of macrophages by inhibiting host macrophage inhibitory factor[6] |
Host response
- Whipworm infection leads to a predominantly T helper cell 2 (Th2) type immune response, which is an antibody based immune response.[7]
- Whipworm infection induces the production of cytokines (interleukin-4, interleukin-5, interleukin-10, and interleukin-13), parasite-specific immunoglobulin, and IgE.[8]
- This leads to stimulation and proliferation of mast cells, eosinophils, and basophils, which play effector roles during the infection.
Associated Conditions
- Whipworm infection is frequently present in combination with Ascaris lumbricoides, Necator americanus and Entamoeba histolytica infections.[9]
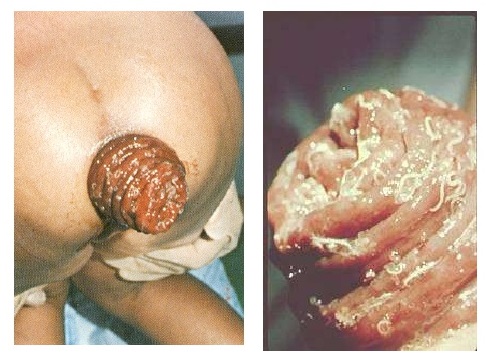
Gross Pathology
- Whipworm infection in humans can lead to rectal prolapse which may be visible grossly.[10]
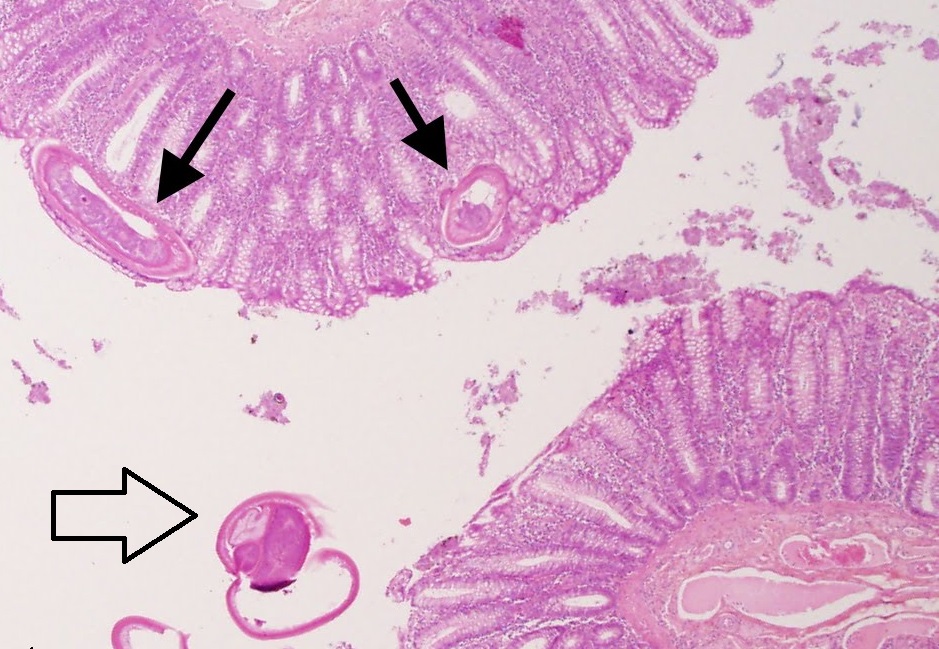
Microscopic Pathology
Colonic Biopsy
- Microscopy of the colonic mucosal biopsy from the affected site will demonstrate infiltration by eosinophils and neutrophils.[11]
- Hematoxylin and eosin (H&E) stain of an infected colon may show one end of the worm embedded in the hyperemic mucosa and other end freely movable within the lumen.[12]
Stool Examination
- A stool examination for ova and parasites reveals the presence of whipworm eggs.
- The diagnostic characteristics are:[13]
- A typical barrel shape
- Two polar plugs, that are unstained
- Size: 50 to 54 µm by 22 to 23 µm
- The external layer of the shell of the egg is yellow-brown (in contrast to the clear polar plugs).

References
- ↑ Elston DM (2006). "What's eating you? Trichuris trichiura (human whipworm)". Cutis. 77 (2): 75–6. PMID 16570666.
- ↑ Elsayed S, Yilmaz A, Hershfield N (2004). "Trichuris trichiura worm infection". Gastrointest Endosc. 60 (6): 990–1. PMID 15605023.
- ↑ Tilney LG, Connelly PS, Guild GM, Vranich KA, Artis D (2005). "Adaptation of a nematode parasite to living within the mammalian epithelium". J Exp Zool A Comp Exp Biol. 303 (11): 927–45. doi:10.1002/jez.a.214. PMID 16217807.
- ↑ Drake L, Korchev Y, Bashford L, Djamgoz M, Wakelin D, Ashall F, Bundy D (1994). "The major secreted product of the whipworm, Trichuris, is a pore-forming protein". Proc. Biol. Sci. 257 (1350): 255–61. doi:10.1098/rspb.1994.0123. PMID 7991635.
- ↑ Parthasarathy G, Mansfield LS (2005). "Trichuris suis excretory secretory products (ESP) elicit interleukin-6 (IL-6) and IL-10 secretion from intestinal epithelial cells (IPEC-1)". Vet. Parasitol. 131 (3–4): 317–24. doi:10.1016/j.vetpar.2005.03.043. PMID 15978725.
- ↑ Tan TH, Edgerton SA, Kumari R, McAlister MS, Roe SM, Nagl S, Pearl LH, Selkirk ME, Bianco AE, Totty NF, Engwerda C, Gray CA, Meyer DJ, Rowe SM (2001). "Macrophage migration inhibitory factor of the parasitic nematode Trichinella spiralis". Biochem. J. 357 (Pt 2): 373–83. PMC 1221963. PMID 11439086.
- ↑ "Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm - ScienceDirect".
- ↑ Maizels RM, Bundy DA, Selkirk ME, Smith DF, Anderson RM (1993). "Immunological modulation and evasion by helminth parasites in human populations". Nature. 365 (6449): 797–805. doi:10.1038/365797a0. PMID 8413664.
- ↑ Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, Hotez PJ (2006). "Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm". Lancet. 367 (9521): 1521–32. doi:10.1016/S0140-6736(06)68653-4. PMID 16679166.
- ↑ "CDC - Trichuriasis".
- ↑ Kaur G, Raj SM, Naing NN (2002). "Trichuriasis: localized inflammatory responses in the colon". Southeast Asian J Trop Med Public Health. 33 (2): 224–8. PMID 12236416.
- ↑ Ok KS, Kim YS, Song JH, Lee JH, Ryu SH, Lee JH, Moon JS, Whang DH, Lee HK (2009). "Trichuris trichiura infection diagnosed by colonoscopy: case reports and review of literature". Korean J. Parasitol. 47 (3): 275–80. doi:10.3347/kjp.2009.47.3.275. PMC 2735694. PMID 19724702.
- ↑ Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, Hotez PJ (2006). "Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm". Lancet. 367 (9521): 1521–32. doi:10.1016/S0140-6736(06)68653-4. PMID 16679166.