Chronic myelogenous leukemia differential diagnosis: Difference between revisions
Usama Talib (talk | contribs) |
Ahmed Younes (talk | contribs) No edit summary |
||
| (18 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | [[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Chronic_myelogenous_leukemia]] | ||
{{ | {{CMG}} {{AE}} {{HMHJ}} {{Badria}} {{MJK}} {{SN}} {{HK}} | ||
==Overview== | ==Overview== | ||
Chronic myelogenous leukemia must be differentiated from [[leukemoid reaction]], [[chronic neutrophilic leukemia]], and [[acute myeloid leukemia]]. | [[Chronic myelogenous leukemia]] must be differentiated from [[leukemoid reaction]], [[chronic neutrophilic leukemia]], and [[acute myeloid leukemia]]. | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Chronic myelogenous leukemia must be differentiated from:<ref name="pmid24839370">{{cite journal| author=Gajendra S, Gupta R, Chandgothia M, Kumar L, Gupta R, Chavan SM| title=Chronic Neutrophilic Leukemia with V617F JAK2 Mutation. | journal=Indian J Hematol Blood Transfus | year= 2014 | volume= 30 | issue= 2 | pages= 139-42 | pmid=24839370 | doi=10.1007/s12288-012-0203-6 | pmc=PMC4022913 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24839370 }} </ref><ref name="pmid17385676">{{cite journal| author=Kanegae MP, Ximenes VF, Falcão RP, Colturato VA, de Mattos ER, Brunetti IL et al.| title=Chemiluminescent determination of leukocyte alkaline phosphatase: an advantageous alternative to the cytochemical assay. | journal=J Clin Lab Anal | year= 2007 | volume= 21 | issue= 2 | pages= 91-6 | pmid=17385676 | doi=10.1002/jcla.20140 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17385676 }} </ref><ref name="pmid24729196">{{cite journal| author=Jabbour E, Kantarjian H| title=Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management. | journal=Am J Hematol | year= 2014 | volume= 89 | issue= 5 | pages= 547-56 | pmid=24729196 | doi=10.1002/ajh.23691 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24729196 }} </ref> | Chronic myelogenous leukemia must be differentiated from:<ref name="pmid24839370">{{cite journal| author=Gajendra S, Gupta R, Chandgothia M, Kumar L, Gupta R, Chavan SM| title=Chronic Neutrophilic Leukemia with V617F JAK2 Mutation. | journal=Indian J Hematol Blood Transfus | year= 2014 | volume= 30 | issue= 2 | pages= 139-42 | pmid=24839370 | doi=10.1007/s12288-012-0203-6 | pmc=PMC4022913 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24839370 }} </ref><ref name="pmid17385676">{{cite journal| author=Kanegae MP, Ximenes VF, Falcão RP, Colturato VA, de Mattos ER, Brunetti IL et al.| title=Chemiluminescent determination of leukocyte alkaline phosphatase: an advantageous alternative to the cytochemical assay. | journal=J Clin Lab Anal | year= 2007 | volume= 21 | issue= 2 | pages= 91-6 | pmid=17385676 | doi=10.1002/jcla.20140 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17385676 }} </ref><ref name="pmid24729196">{{cite journal| author=Jabbour E, Kantarjian H| title=Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management. | journal=Am J Hematol | year= 2014 | volume= 89 | issue= 5 | pages= 547-56 | pmid=24729196 | doi=10.1002/ajh.23691 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24729196 }} </ref><ref name="pmid14521811">{{cite journal |vauthors=Niemeyer CM, Kratz C |title=Juvenile myelomonocytic leukemia |journal=Curr Oncol Rep |volume=5 |issue=6 |pages=510–5 |date=November 2003 |pmid=14521811 |doi= |url=}}</ref><ref name="pmid10847463">{{cite journal |vauthors=Hernández JM, del Cañizo MC, Cuneo A, García JL, Gutiérrez NC, González M, Castoldi G, San Miguel JF |title=Clinical, hematological and cytogenetic characteristics of atypical chronic myeloid leukemia |journal=Ann. Oncol. |volume=11 |issue=4 |pages=441–4 |date=April 2000 |pmid=10847463 |doi= |url=}}</ref><ref name="pmid9844604">{{cite journal |vauthors=Oliver JW, Deol I, Morgan DL, Tonk VS |title=Chronic eosinophilic leukemia and hypereosinophilic syndromes. Proposal for classification, literature review, and report of a case with a unique chromosomal abnormality |journal=Cancer Genet. Cytogenet. |volume=107 |issue=2 |pages=111–7 |date=December 1998 |pmid=9844604 |doi= |url=}}</ref><ref name="pmid8857931">{{cite journal |vauthors=Bain BJ |title=Eosinophilic leukaemias and the idiopathic hypereosinophilic syndrome |journal=Br. J. Haematol. |volume=95 |issue=1 |pages=2–9 |date=October 1996 |pmid=8857931 |doi= |url=}}</ref><ref name="pmid18439674">{{cite journal |vauthors=Krämer A |title=JAK2-V617F and BCR-ABL--double jeopardy? |journal=Leuk. Res. |volume=32 |issue=10 |pages=1489–90 |date=October 2008 |pmid=18439674 |doi=10.1016/j.leukres.2008.03.011 |url=}}</ref><ref name="pmid15087070">{{cite journal |vauthors=Elliott MA |title=Chronic neutrophilic leukemia: a contemporary review |journal=Curr. Hematol. Rep. |volume=3 |issue=3 |pages=210–7 |date=May 2004 |pmid=15087070 |doi= |url=}}</ref><ref name="pmid23896413">{{cite journal |vauthors=Gotlib J, Maxson JE, George TI, Tyner JW |title=The new genetics of chronic neutrophilic leukemia and atypical CML: implications for diagnosis and treatment |journal=Blood |volume=122 |issue=10 |pages=1707–11 |date=September 2013 |pmid=23896413 |pmc=3765056 |doi=10.1182/blood-2013-05-500959 |url=}}</ref><ref name="pmid1467514">{{cite journal |vauthors=Westbrook CA, Hooberman AL, Spino C, Dodge RK, Larson RA, Davey F, Wurster-Hill DH, Sobol RE, Schiffer C, Bloomfield CD |title=Clinical significance of the BCR-ABL fusion gene in adult acute lymphoblastic leukemia: a Cancer and Leukemia Group B Study (8762) |journal=Blood |volume=80 |issue=12 |pages=2983–90 |date=December 1992 |pmid=1467514 |doi= |url=}}</ref><ref name="pmid24839370" /> | ||
*[[Leukemoid reaction]] | *[[Leukemoid reaction]] | ||
:* | *[[Basophil]]s and [[eosinophil]]s are almost always increased in chronic myelogenous leukemia | ||
::* | |||
::*[[ | * [[Chronic neutrophilic leukemia]] | ||
::* | * [[Acute myeloid leukemia]] | ||
::*Absence of [[ | * [[Thrombocytosis]] | ||
:*[[ | * [[Chronic lymphoid leukemia]] | ||
*[[ | * [[Acute myeloid leukemia]] | ||
*[[ | * [[Juvenile myelomonocytic leukemia]] | ||
*[[ | * [[Chronic myelomonocytic leukemia ]] | ||
* [[Atypical CML]] | |||
* [[Chronic eosinophilic leukemia]] | |||
* [[Polycythemia vera]] | |||
* [[Essential thrombocytosis]] | |||
* The following table differentiates chronic myelogenous leukemia from other leukemias that may present with similar clinical features such as fever, fatigue, weight loss, recurrent infections and elevated leukocyte counts. The following are the differentials: | |||
==Differentiating Myeloproliferative Disorders== | |||
'''<small>ABBREVIATIONS''' | |||
'''N/A''': Not available, '''NL''': Normal, '''FISH''': Fluorescence in situ hybridization, '''PCR''': Polymerase chain reaction, '''LDH''': Lactate dehydrogenase, '''PUD''': Peptic ulcer disease, '''EPO''': Erythropoietin, '''LFTs''': Liver function tests, '''RFTs''': Renal function tests, '''LAP''': Leukocyte alkaline phosphatase, '''LAD''': Leukocyte alkaline dehydrgenase, '''WBCs''': White blood cells. </small> | |||
<small> | |||
{| class="wikitable" | |||
! colspan="2" rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Myeloproliferative neoplasms (MPN) | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Clinical manifestations | |||
! colspan="11" style="background:#4479BA; color: #FFFFFF;" align="center" + |Diagnosis | |||
! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Other features | |||
|- | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Symptoms | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Physical examination | |||
! colspan="9" style="background:#4479BA; color: #FFFFFF;" align="center" + |CBC & Peripheral smear | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Bone marrow biopsy | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Other investigations | |||
|- | |||
! colspan="7" style="background:#4479BA; color: #FFFFFF;" align="center" + |WBCs | |||
! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Hb | |||
! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Plat-<br>elets | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Leuko-cytes</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Blasts</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Left<br>shift</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Baso-<br>phils</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Eosino-<br>phils</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Mono-<br>cytes</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Others</small> | |||
|- | |||
| colspan="2" |[[Chronic myeloid leukemia]]<br>([[CML]]), [[BCR/ABL|BCR-ABL1]]+<ref name="pmid9012696">{{cite journal |vauthors=Savage DG, Szydlo RM, Goldman JM |title=Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period |journal=Br. J. Haematol. |volume=96 |issue=1 |pages=111–6 |date=January 1997 |pmid=9012696 |doi= |url=}}</ref><ref name="pmid26434969">{{cite journal |vauthors=Thompson PA, Kantarjian HM, Cortes JE |title=Diagnosis and Treatment of Chronic Myeloid Leukemia in 2015 |journal=Mayo Clin. Proc. |volume=90 |issue=10 |pages=1440–54 |date=October 2015 |pmid=26434969 |pmc=5656269 |doi=10.1016/j.mayocp.2015.08.010 |url=}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional</small> | |||
* <small>[[Hyperviscosity]] and/or [[anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Splenomegaly]]<br>(46–76%)</small> | |||
* <small>[[Purpura]]</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Priapism]]</small> | |||
|↑ | |||
|<small><2%</small> | |||
| + | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>NL</small> | |||
| | |||
* <small>Hypercellurarity with ↑ [[granuloscytosis]] and ↓ [[erythrocytosis]]</small> | |||
* <small>[[Fibrosis]]</small> | |||
| | |||
* <small>[[FISH]] for t(9;22)(q34;q11.2)</small> | |||
* <small>[[Reverse transcriptase]] quantitative [[PCR]] (RQ-PCR) for BCR-ABL</small> | |||
| | |||
* <small>[[Granulocytic]] [[dysplasia]] is minimal/absent</small> | |||
* <small>May present with [[blast]] crisis</small> | |||
* <small>Absolute [[leukocytosis]]</small> <small>(median of 100,000/µL)</small> | |||
* <small>Classic [[myelocyte]] bulge</small> | |||
* <small>[[thrombocytopenia]] indicates advanced stage</small> | |||
|- | |||
| colspan="2" |[[Chronic neutrophilic leukemia]] ([[CNL]])<ref name="pmid29440636">{{cite journal |vauthors=Szuber N, Tefferi A |title=Chronic neutrophilic leukemia: new science and new diagnostic criteria |journal=Blood Cancer J |volume=8 |issue=2 |pages=19 |date=February 2018 |pmid=29440636 |pmc=5811432 |doi=10.1038/s41408-018-0049-8 |url=}}</ref><ref name="pmid28028025">{{cite journal |vauthors=Maxson JE, Tyner JW |title=Genomics of chronic neutrophilic leukemia |journal=Blood |volume=129 |issue=6 |pages=715–722 |date=February 2017 |pmid=28028025 |pmc=5301820 |doi=10.1182/blood-2016-10-695981 |url=}}</ref><ref name="pmid26366092">{{cite journal |vauthors=Menezes J, Cigudosa JC |title=Chronic neutrophilic leukemia: a clinical perspective |journal=Onco Targets Ther |volume=8 |issue= |pages=2383–90 |date=2015 |pmid=26366092 |pmc=4562747 |doi=10.2147/OTT.S49688 |url=}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional symptoms</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Heptomegaly]]</small> | |||
* <small>[[Purpura]]</small> | |||
* <small>[[Anemia]] related</small> | |||
|↑ | |||
|<small>Minimal</small> | |||
| + | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[LDH]]</small> | |||
* <small>↑ [[B12]] levels</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Uniforme and intense hypercellularity with minimal to none [[fibrosis]]</small> | |||
* <small>[[Neutrophil]] toxic granulations and [[Dohle bodies]]</small> | |||
| | |||
* <small>[[FISH]]</small> | |||
* <small>Imaging for [[hepatosplenomegaly]]</small> | |||
| | |||
* <small>Associationed with [[polycythemia vera]] and [[plasma cell disorders]]</small> | |||
* <small>[[Leukocytosis]] with<br>[[chronic]] [[neutrophilia]]</small> | |||
|- | |||
| colspan="2" |[[Polycythemia vera]]<br>([[PV]])<ref name="pmid29194068">{{cite journal |vauthors=Vannucchi AM, Guglielmelli P, Tefferi A |title=Polycythemia vera and essential thrombocythemia: algorithmic approach |journal=Curr. Opin. Hematol. |volume=25 |issue=2 |pages=112–119 |date=March 2018 |pmid=29194068 |doi=10.1097/MOH.0000000000000402 |url=}}</ref><ref name="pmid30252337">{{cite journal |vauthors=Pillai AA, Babiker HM |title= |journal= |volume= |issue= |pages= |date= |pmid=30252337 |doi= |url=}}</ref><ref name="pmid30281843">{{cite journal |vauthors=Tefferi A, Barbui T |title=Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management |journal=Am. J. Hematol. |volume=94 |issue=1 |pages=133–143 |date=January 2019 |pmid=30281843 |doi=10.1002/ajh.25303 |url=}}</ref><ref name="pmid28028026">{{cite journal |vauthors=Rumi E, Cazzola M |title=Diagnosis, risk stratification, and response evaluation in classical myeloproliferative neoplasms |journal=Blood |volume=129 |issue=6 |pages=680–692 |date=February 2017 |pmid=28028026 |pmc=5335805 |doi=10.1182/blood-2016-10-695957 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Thromboembolism]]<br>and [[bleeding]]</small> | |||
* <small>[[Pruritus]] after<br>a warm bath</small> | |||
* <small>[[PUD]] related</small> | |||
| | |||
* <small>Facial ruddiness</small> | |||
* <small>Related to underlying cause</small> | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Renal]] [[bruit]]</small> | |||
|<small>NL or ↑</small> | |||
|<small>None</small> | |||
| - | |||
|<small>↑ or ↓</small> | |||
|<small>NL or ↑</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↓ Serum [[ferritin]]</small> | |||
* <small>↓ [[Folate]] levels</small> | |||
* <small>↑↑ [[B12]] levels</small> | |||
|<small>↑↑</small> | |||
|<small>NL</small> | |||
| | |||
* <small>Hypercellularity for age with tri-lineage growth</small> | |||
* <small>[[Myelofibrosis]] (in up to 20% of patients)</small> | |||
| | |||
* <small>[[Radioisotope]] studies</small> | |||
* <small>[[Serum]] [[EPO]] levels</small> | |||
* <small>[[LFTs]]</small> | |||
* <small>[[RFTs]]</small> | |||
* <small>[[Imaging]] studies</small> | |||
| | |||
* <small>May transform into [[myelofibrosis]] or [[leukemia]]</small> | |||
|- | |||
| colspan="2" |[[Primary myelofibrosis]] ([[PMF]])<ref name="pmid26891375">{{cite journal |vauthors=Cervantes F, Correa JG, Hernandez-Boluda JC |title=Alleviating anemia and thrombocytopenia in myelofibrosis patients |journal=Expert Rev Hematol |volume=9 |issue=5 |pages=489–96 |date=May 2016 |pmid=26891375 |doi=10.1586/17474086.2016.1154452 |url=}}</ref><ref>{{cite book | last = Hoffman | first = Ronald | title = Hematology : basic principles and practice | publisher = Elsevier | location = Philadelphia, PA | year = 2018 | isbn = 9780323357623 }}</ref><ref name="pmid16919893">{{cite journal |vauthors=Michiels JJ, Bernema Z, Van Bockstaele D, De Raeve H, Schroyens W |title=Current diagnostic criteria for the chronic myeloproliferative disorders (MPD) essential thrombocythemia (ET), polycythemia vera (PV) and chronic idiopathic myelofibrosis (CIMF) |journal=Pathol. Biol. |volume=55 |issue=2 |pages=92–104 |date=March 2007 |pmid=16919893 |doi=10.1016/j.patbio.2006.06.002 |url=}}</ref><ref>{{cite book | last = Hoffman | first = Ronald | title = Hematology : basic principles and practice | publisher = Elsevier | location = Philadelphia, PA | year = 2018 | isbn = 9780323357623 }}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
* <small>[[Abdominal]] [[Pain]]</small> | |||
| | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
* <small>[[Petechiae]] & [[ecchymoses]]</small> | |||
* <small>Abdominal distension</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
|↓ | |||
|<small>[[Erythroblasts]]</small> | |||
| - | |||
|<small>Absent</small> | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[LAP]]</small> | |||
* <small>↑ [[LAD]]</small> | |||
* ↑ <small>[[Uric acid]]</small> | |||
* <small>↑ [[B12]] levels</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Variable with [[fibrosis]] or hypercellularity</small> | |||
| | |||
* <small>JAK2 mutation</small> | |||
* <small>[[CALR]] [[mutation]]</small> | |||
* <small>[[MPL]] [[mutation]]</small> | |||
| | |||
* <small>[[Bone marrow]] aspiration shows a dry tap</small> | |||
* <small>Variable with [[leukocytosis]] or [[leukopenia]]</small> | |||
|- | |||
| colspan="2" |[[Essential thrombocythemia]] ([[ET]])<ref name="pmidhttp://dx.doi.org/10.1182/blood-2007-04-083501">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=http://dx.doi.org/10.1182/blood-2007-04-083501 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref>{{Cite journal | |||
| author = [[Daniel A. Arber]], [[Attilio Orazi]], [[Robert Hasserjian]], [[Jurgen Thiele]], [[Michael J. Borowitz]], [[Michelle M. Le Beau]], [[Clara D. Bloomfield]], [[Mario Cazzola]] & [[James W. Vardiman]] | |||
| title = The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia | |||
| journal = [[Blood]] | |||
| volume = 127 | |||
| issue = 20 | |||
| pages = 2391–2405 | |||
| year = 2016 | |||
| month = May | |||
| doi = 10.1182/blood-2016-03-643544 | |||
| pmid = 27069254 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[A. Tefferi]], [[R. Fonseca]], [[D. L. Pereira]] & [[H. C. Hoagland]] | |||
| title = A long-term retrospective study of young women with essential thrombocythemia | |||
| journal = [[Mayo Clinic proceedings]] | |||
| volume = 76 | |||
| issue = 1 | |||
| pages = 22–28 | |||
| year = 2001 | |||
| month = January | |||
| doi = 10.4065/76.1.22 | |||
| pmid = 11155408 | |||
}}</ref> | |||
| | |||
* <small>Headache</small> | |||
* <small>[[Dizziness]]</small> | |||
* <small>[[Visual]] disturbances</small> | |||
* <small>[[Priapism]]</small> | |||
* <small>Acute [[chest pain]]</small> | |||
| | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Skin]] [[bruises]]</small> | |||
| | |||
<small>NL or ↑</small> | |||
| | |||
<small>None</small> | |||
| - | |||
| | |||
<small>↓ or absent</small> | |||
| | |||
<small>NL</small> | |||
| | |||
<small>NL</small> | |||
| | |||
* <small>N/A</small> | |||
| | |||
[[Anemia|<small>↓</small>]] | |||
| | |||
<small>↑↑</small> | |||
| | |||
* <small>Normal/Hypercellular</small> | |||
| | |||
* <small>[[JAK2]] [[mutation]]</small> | |||
* <small>[[CALR]] [[mutation]]</small> | |||
* <small>[[MPL]] [[mutation]]</small> | |||
| | |||
* <small>[[Thrombosis]]</small> | |||
* <small>[[Hemorrhage]]</small> | |||
* <small>[[Pregnancy]] loss</small> | |||
|- | |||
| colspan="2" |[[Chronic eosinophilic leukemia]],<br>not otherwise specified<br>(NOS)<ref name="pmid27512192">{{cite journal |vauthors=Vidyadharan S, Joseph B, Nair SP |title=Chronic Eosinophilic Leukemia Presenting Predominantly with Cutaneous Manifestations |journal=Indian J Dermatol |volume=61 |issue=4 |pages=437–9 |date=2016 |pmid=27512192 |pmc=4966405 |doi=10.4103/0019-5154.185716 |url=}}</ref><ref name="pmid29892549">{{cite journal |vauthors=Hofmans M, Delie A, Vandepoele K, Van Roy N, Van der Meulen J, Philippé J, Moors I |title=A case of chronic eosinophilic leukemia with secondary transformation to acute myeloid leukemia |journal=Leuk Res Rep |volume=9 |issue= |pages=45–47 |date=2018 |pmid=29892549 |pmc=5993353 |doi=10.1016/j.lrr.2018.04.001 |url=}}</ref><ref name="pmid23662039">{{cite journal |vauthors=Yamada Y, Rothenberg ME, Cancelas JA |title=Current concepts on the pathogenesis of the hypereosinophilic syndrome/chronic eosinophilic leukemia |journal=Transl Oncogenomics |volume=1 |issue= |pages=53–63 |date=2006 |pmid=23662039 |pmc=3642145 |doi= |url=}}</ref><ref name="pmid27722133">{{cite journal |vauthors=Kim TH, Gu HJ, Lee WI, Lee J, Yoon HJ, Park TS |title=Chronic eosinophilic leukemia with FIP1L1-PDGFRA rearrangement |journal=Blood Res |volume=51 |issue=3 |pages=204–206 |date=September 2016 |pmid=27722133 |doi=10.5045/br.2016.51.3.204 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Rash]]</small> | |||
* <small>[[Rhinitis]]</small> | |||
* <small>[[Gastritis]]</small> | |||
* <small>[[Thromboembolism]]<br>related</small> | |||
| | |||
* <small>[[Hypertension]]</small> | |||
* <small>[[Eczema]], [[mucosal]] [[ulcers]], [[erythema]]</small> | |||
* <small>[[Angioedema]]</small> | |||
* <small>[[Ataxia]]</small> | |||
* <small>[[Anemia]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>Present</small> | |||
| + | |||
|<small>↑</small> | |||
|<small>↑↑</small> | |||
|<small>↑</small> | |||
| | |||
* <small>↑ [[B12]] levels</small> | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercelluar with ↑ [[eosinophilic]] precursors, ↑ [[eosinophils]], and atypical [[mononuclear cells]]</small> | |||
| | |||
* <small>[[FISH]]</small> | |||
* <small>Cytogenetic analysis of purified [[eosinophils]] and [[X-chromosome]] inactivation analysis</small> | |||
| | |||
* <small>[[Heart failure]]</small> <small>[[Lung fibrosis]]</small> | |||
* <small>[[Encephalopathy]]</small> | |||
* <small>[[Erythema annulare centrifugam]]</small> | |||
|- | |||
| colspan="2" |[[Myeloproliferative neoplasm|MPN]],<br>unclassifiable | |||
|<small> | |||
*Similar to other<br>[[Myeloproliferative neoplasm|myeloproliferative neoplasms]]</small> | |||
|<small> | |||
*Similar to other<br>[[Myeloproliferative neoplasm|myeloproliferative neoplasms]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>Variable</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>May resemble other<br>[[myeloproliferative neoplasms]]</small> | |||
|<small>↓</small> | |||
|<small>↑</small> | |||
| | |||
* <small>↑ [[megakaryocyte]] proliferation with variable hypercellularity in [[granulocytic]] or [[erythrocytic]] cell lines</small> | |||
| | |||
* <small>N/A</small> | |||
|<small> | |||
*Similar to other [[myeloprolifeartive neoplasms]] but do not fulfil the criteria to be classified to a specific type</small> | |||
|- | |||
| colspan="2" |[[Mastocytosis]]<ref name="pmid24262698">{{cite journal |vauthors=Carter MC, Metcalfe DD, Komarow HD |title=Mastocytosis |journal=Immunol Allergy Clin North Am |volume=34 |issue=1 |pages=181–96 |date=February 2014 |pmid=24262698 |pmc=3863935 |doi=10.1016/j.iac.2013.09.001 |url=}}</ref><ref name="pmid29494109">{{cite journal |vauthors=Macri A, Cook C |title= |journal= |volume= |issue= |pages= |date= |pmid=29494109 |doi= |url=}}</ref><ref name="pmid25031064">{{cite journal |vauthors=Lladó AC, Mihon CE, Silva M, Galzerano A |title=Systemic mastocytosis - a diagnostic challenge |journal=Rev Bras Hematol Hemoter |volume=36 |issue=3 |pages=226–9 |date=2014 |pmid=25031064 |pmc=4109736 |doi=10.1016/j.bjhh.2014.03.003 |url=}}</ref><ref name="pmid28031180">{{cite journal |vauthors=Valent P, Akin C, Metcalfe DD |title=Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts |journal=Blood |volume=129 |issue=11 |pages=1420–1427 |date=March 2017 |pmid=28031180 |pmc=5356454 |doi=10.1182/blood-2016-09-731893 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Pruritus]] & [[Flushing]]</small> | |||
* <small>[[Urticaria]] & [[Blisters]]</small> | |||
* <small>[[Hypotension]] & [[PUD]]</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Bronchoconstriction]]</small> | |||
| | |||
* <small>[[Mastocytosis exanthema]]</small> | |||
* <small>[[Blistering]]</small> | |||
* <small>[[Swelling]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Fibrosis]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>None</small> | |||
| - | |||
|<small>NL</small> | |||
|<small>[[Eosinophilia|↑]]</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[Alkaline phosphatase]]</small> | |||
* <small>↑ [[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>↓ or ↑</small> | |||
| | |||
* <small>Multifocal dense infiltrates of [[mast cells]] with atypical [[morphology]] in >25 %</small> | |||
| | |||
* <small>Cytogenetic analysis for [[c-KIT]] [[receptor]] [[mutations]]</small> | |||
* <small>[[Serum]] [[tryptase]] levels</small> | |||
* <small>24-hour urine test for N-methyl [[histamine]] and 11-beta-[[prostaglandine]]</small> | |||
| | |||
* <small>Skin most commonly involved</small> | |||
* <small>Susceptibility to [[anaphylaxix]]</small> | |||
* <small>[[Osteoporosis]]</small> | |||
|- | |||
| colspan="2" |[[Myeloid]]/[[lymphoid]] [[neoplasms]]<br>with [[eosinophilia]] and rearrangement<br>of [[PDGFR|PDGFRA]], [[PDGFRB]], or [[FGFR1]],<br>or with [[PCM1]]-[[JAK2]]<ref name="KumarChen2015">{{cite journal|last1=Kumar|first1=Kirthi R.|last2=Chen|first2=Weina|last3=Koduru|first3=Prasad R.|last4=Luu|first4=Hung S.|title=Myeloid and Lymphoid Neoplasm With Abnormalities of FGFR1 Presenting With Trilineage Blasts and RUNX1 Rearrangement|journal=American Journal of Clinical Pathology|volume=143|issue=5|year=2015|pages=738–748|issn=1943-7722|doi=10.1309/AJCPUD6W1JLQQMNA}}</ref><ref>{{Cite journal | |||
| author = [[Paolo Strati]], [[Guilin Tang]], [[Dzifa Y. Duose]], [[Saradhi Mallampati]], [[Rajyalakshmi Luthra]], [[Keyur P. Patel]], [[Mohammad Hussaini]], [[Abu-Sayeef Mirza]], [[Rami S. Komrokji]], [[Stephen Oh]], [[John Mascarenhas]], [[Vesna Najfeld]], [[Vivek Subbiah]], [[Hagop Kantarjian]], [[Guillermo Garcia-Manero]], [[Srdan Verstovsek]] & [[Naval Daver]] | |||
| title = Myeloid/lymphoid neoplasms with FGFR1 rearrangement | |||
| journal = [[Leukemia & lymphoma]] | |||
| volume = 59 | |||
| issue = 7 | |||
| pages = 1672–1676 | |||
| year = 2018 | |||
| month = July | |||
| doi = 10.1080/10428194.2017.1397663 | |||
| pmid = 29119847 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Ximena Montenegro-Garreaud]], [[Roberto N. Miranda]], [[Alexandra Reynolds]], [[Guilin Tang]], [[Sa A. Wang]], [[Mariko Yabe]], [[Wei Wang]], [[Lianghua Fang]], [[Carlos E. Bueso-Ramos]], [[Pei Lin]], [[L. Jeffrey Medeiros]] & [[Xinyan Lu]] | |||
| title = Myeloproliferative neoplasms with t(8;22)(p11.2;q11.2)/BCR-FGFR1: a meta-analysis of 20 cases shows cytogenetic progression with B-lymphoid blast phase | |||
| journal = [[Human pathology]] | |||
| volume = 65 | |||
| pages = 147–156 | |||
| year = 2017 | |||
| month = July | |||
| doi = 10.1016/j.humpath.2017.05.008 | |||
| pmid = 28551329 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Paola Villafuerte-Gutierrez]], [[Montserrat Lopez Rubio]], [[Pilar Herrera]] & [[Eva Arranz]] | |||
| title = A Case of Myeloproliferative Neoplasm with BCR-FGFR1 Rearrangement: Favorable Outcome after Haploidentical Allogeneic Transplantation | |||
| journal = [[Case reports in hematology]] | |||
| volume = 2018 | |||
| pages = 5724960 | |||
| year = 2018 | |||
| month = | |||
| doi = 10.1155/2018/5724960 | |||
| pmid = 30647980 | |||
}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional</small> | |||
* <small>[[Rash]]</small> | |||
* <small>[[Cough]] & breathlessness</small> | |||
* <small>[[Peripheral neuropathy]]/<br>[[encephalopathy]]</small> | |||
| | |||
* <small>[[Fever]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
| ↑ | |||
| <small>NL</small> | |||
| - | |||
| <small>NL</small> | |||
| <small>[[Eosinophilia|↑]]</small> | |||
|<small>[[Monocytosis|↑]]</small> | |||
| | |||
* <small>None</small> | |||
| <small>NL</small> | |||
| <small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Myeloid]] expansion with [[eosinophilia]]</small> | |||
| | |||
* <small>[[FISH]] shows t(8;13) and t(8;22)</small> | |||
| | |||
* <small>May present or evolve into [[acute myeloid]] or [[lymphoblastic leukemia]]</small> | |||
* <small>[[Leukocytosis]] (30 - 59 × 10<sup>9</sup>/L</small> | |||
|- | |||
| colspan="2" |B-lymphoblastic leukemia/lymphoma<ref name="pmid30107017">{{cite journal |vauthors=Kamiya-Matsuoka C, Garciarena P, Amin HM, Tremont-Lukats IW, de Groot JF |title=B lymphoblastic leukemia/lymphoma presenting as seventh cranial nerve palsy |journal=Neurol Clin Pract |volume=3 |issue=6 |pages=532–534 |date=December 2013 |pmid=30107017 |pmc=6082360 |doi=10.1212/CPJ.0b013e3182a78ef0 |url=}}</ref><ref name="pmid29029550">{{cite journal |vauthors=Zhang X, Rastogi P, Shah B, Zhang L |title=B lymphoblastic leukemia/lymphoma: new insights into genetics, molecular aberrations, subclassification and targeted therapy |journal=Oncotarget |volume=8 |issue=39 |pages=66728–66741 |date=September 2017 |pmid=29029550 |pmc=5630450 |doi=10.18632/oncotarget.19271 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
* <small>[[Bone pain]]</small> | |||
| | |||
* <small>[[Pallor]]</small> | |||
* <small>[[Petechiae]]</small> | |||
* <small>[[Organomegaly]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
|<small>NL or ↑</small> | |||
|<small>>25%</small> | |||
|<small>N/A</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>[[Auer rod|Auer bodies]]</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercellular with [[blast]] infilteration</small><small>with or without [[myelodysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>May present as [[Extramedullary myeloid tumor|extramedullary]] disease ([[Extramedullary Myeloid Cell Tumor|Myeloid sarcoma]])</small> | |||
|- | |||
| colspan="2" |[[Myelodysplastic syndrome|Myelodysplastic syndromes]]<br>([[MDS]])<ref name="pmid24300826">{{cite journal |vauthors=Germing U, Kobbe G, Haas R, Gattermann N |title=Myelodysplastic syndromes: diagnosis, prognosis, and treatment |journal=Dtsch Arztebl Int |volume=110 |issue=46 |pages=783–90 |date=November 2013 |pmid=24300826 |pmc=3855821 |doi=10.3238/arztebl.2013.0783 |url=}}</ref><ref name="pmid26769228">{{cite journal |vauthors=Gangat N, Patnaik MM, Tefferi A |title=Myelodysplastic syndromes: Contemporary review and how we treat |journal=Am. J. Hematol. |volume=91 |issue=1 |pages=76–89 |date=January 2016 |pmid=26769228 |doi=10.1002/ajh.24253 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Pallor]]</small> | |||
* <small>[[Petechiae]]</small> | |||
* <small>[[Organomegaly]]</small> | |||
|[[Leukopenia|<small>↓</small>]] | |||
|<small>Variable</small> | |||
| - | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Macro-ovalocytes</small> | |||
* <small>Basophilic stippling</small> | |||
* [[Howell-Jolly body|<small>Howell-Jolly body</small>]] | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercellular</small><small>/ normocellular [[bone marrow]] with [[Dysplastic change|dysplastic]] changes</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>[[Leukemia]] transformation</small> | |||
* <small>Acquired pseudo-Pelger-Huët anomaly</small> | |||
|- | |||
| colspan="2" |[[Acute myeloid leukemia]] ([[AML]])<br>and related [[neoplasms]]<ref name="pmid3864727">{{cite journal |vauthors=Islam A, Catovsky D, Goldman JM, Galton DA |title=Bone marrow biopsy changes in acute myeloid leukaemia. I: Observations before chemotherapy |journal=Histopathology |volume=9 |issue=9 |pages=939–57 |date=September 1985 |pmid=3864727 |doi= |url=}}</ref><ref name="pmid17587881">{{cite journal |vauthors=Orazi A |title=Histopathology in the diagnosis and classification of acute myeloid leukemia, myelodysplastic syndromes, and myelodysplastic/myeloproliferative diseases |journal=Pathobiology |volume=74 |issue=2 |pages=97–114 |date=2007 |pmid=17587881 |doi=10.1159/000101709 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* [[Bleeding|<small>Bleeding</small>]] | |||
* [[Bone pain|<small>Bone pain</small>]] | |||
* [[Joint pain|<small>Joint pain</small>]] | |||
* [[Infections|<small>Infections</small>]] | |||
| | |||
* <small>[[Infection]] related</small> | |||
* [[Pallor|<small>Pallor</small>]] | |||
* [[Chloroma|<small>Leukemia cutis</small>]] | |||
* <small>[[Bruising]] & [[Petechia|petechiae]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* [[Hepatomegaly|<small>Hepatosplenomegaly</small>]] | |||
|<small>NL or ↑</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>↑ [[Potassium]]</small> | |||
* <small>↑ [[Uric acid]]</small> | |||
* <small>↑ [[Phosphorus]]</small> | |||
* <small>↓ [[Calcium]]</small> | |||
* <small>↑ [[LDH]]</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Increased immature[[myeloid]] [[cells]]</small> | |||
<small>with [[Dysplastic change|dysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>Common in [[Down syndrome]]</small> | |||
|- | |||
| colspan="2" |[[Blastic plasmacytoid dendritic cell neoplasm|Blastic plasmacytoid<br>dendritic cell neoplasm]]<ref>{{Cite journal | |||
| author = [[F. Julia]], [[T. Petrella]], [[M. Beylot-Barry]], [[M. Bagot]], [[D. Lipsker]], [[L. Machet]], [[P. Joly]], [[O. Dereure]], [[M. Wetterwald]], [[M. d'Incan]], [[F. Grange]], [[J. Cornillon]], [[G. Tertian]], [[E. Maubec]], [[P. Saiag]], [[S. Barete]], [[I. Templier]], [[F. Aubin]] & [[S. Dalle]] | |||
| title = Blastic plasmacytoid dendritic cell neoplasm: clinical features in 90 patients | |||
| journal = [[The British journal of dermatology]] | |||
| volume = 169 | |||
| issue = 3 | |||
| pages = 579–586 | |||
| year = 2013 | |||
| month = September | |||
| doi = 10.1111/bjd.12412 | |||
| pmid = 23646868 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Livio Pagano]], [[Caterina Giovanna Valentini]], [[Alessandro Pulsoni]], [[Simona Fisogni]], [[Paola Carluccio]], [[Francesco Mannelli]], [[Monia Lunghi]], [[Gianmatteo Pica]], [[Francesco Onida]], [[Chiara Cattaneo]], [[Pier Paolo Piccaluga]], [[Eros Di Bona]], [[Elisabetta Todisco]], [[Pellegrino Musto]], [[Antonio Spadea]], [[Alfonso D'Arco]], [[Stefano Pileri]], [[Giuseppe Leone]], [[Sergio Amadori]] & [[Fabio Facchetti]] | |||
| title = Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study | |||
| journal = [[Haematologica]] | |||
| volume = 98 | |||
| issue = 2 | |||
| pages = 239–246 | |||
| year = 2013 | |||
| month = February | |||
| doi = 10.3324/haematol.2012.072645 | |||
| pmid = 23065521 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Joseph D. Khoury]] | |||
| title = Blastic Plasmacytoid Dendritic Cell Neoplasm | |||
| journal = [[Current hematologic malignancy reports]] | |||
| volume = 13 | |||
| issue = 6 | |||
| pages = 477–483 | |||
| year = 2018 | |||
| month = December | |||
| doi = 10.1007/s11899-018-0489-z | |||
| pmid = 30350260 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Shinichiro Sukegawa]], [[Mamiko Sakata-Yanagimoto]], [[Ryota Matsuoka]], [[Haruka Momose]], [[Yusuke Kiyoki]], [[Masayuki Noguchi]], [[Naoya Nakamura]], [[Rei Watanabe]], [[Manabu Fujimoto]], [[Yasuhisa Yokoyama]], [[Hidekazu Nishikii]], [[Takayasu Kato]], [[Manabu Kusakabe]], [[Naoki Kurita]], [[Naoshi Obara]], [[Yuichi Hasegawa]] & [[Shigeru Chiba]] | |||
| title = [Blastic plasmacytoid dendritic cell neoplasm accompanied by chronic myelomonocytic leukemia successfully treated with azacitidine] | |||
| journal = <nowiki>[[[Rinsho ketsueki] The Japanese journal of clinical hematology]]</nowiki> | |||
| volume = 59 | |||
| issue = 12 | |||
| pages = 2567–2573 | |||
| year = 2018 | |||
| month = | |||
| doi = 10.11406/rinketsu.59.2567 | |||
| pmid = 30626790 | |||
}}</ref> | |||
| | |||
* <small>[[Cutaneous]] symptoms (brown/purple nodular lesions) on [[face]], [[scalp]], [[lower limb]] & [[trunk]]</small> | |||
| | |||
* <small>Brown/violaceous [[bruise]] like lesions</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Splenomegaly]]</small> | |||
| <small>NL</small> | |||
| <small>↑</small> | |||
| | |||
|<small>NL</small> | |||
| <small>NL</small> | |||
| <small>NL</small> | |||
| | |||
* <small>[[Neutropenia]]</small> | |||
| [[Anemia|<small>↓</small>]] | |||
| <small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Malignant|Malignant cells]]</small> | |||
| | |||
* <small>[[Immunohistochemistry]] or [[flow cytometry]] for [[CD4]] & [[CD56]]</small> | |||
| | |||
* <small>TdT expression positive</small> | |||
* <small>May develop [[chronic myelomonocytic leukemia]] (CMML)</small> | |||
|- | |||
| rowspan="4" |[[Myelodysplastic]]<br>/[[Myeloproliferative neoplasm|myeloproliferative<br>neoplasms]] (MDS/MPN) | |||
|<small>[[Chronic myelomonocytic leukemia]] (CMML)</small><ref name="pmid27185207">{{cite journal |vauthors=Patnaik MM, Tefferi A |title=Chronic myelomonocytic leukemia: 2016 update on diagnosis, risk stratification, and management |journal=Am. J. Hematol. |volume=91 |issue=6 |pages=631–42 |date=June 2016 |pmid=27185207 |doi=10.1002/ajh.24396 |url=}}</ref> | |||
: <ref name="pmid22615103">{{cite journal |vauthors=Parikh SA, Tefferi A |title=Chronic myelomonocytic leukemia: 2012 update on diagnosis, risk stratification, and management |journal=Am. J. Hematol. |volume=87 |issue=6 |pages=610–9 |date=June 2012 |pmid=22615103 |doi=10.1002/ajh.23203 |url=}}</ref><ref name="pmid25869097">{{cite journal |vauthors=Benton CB, Nazha A, Pemmaraju N, Garcia-Manero G |title=Chronic myelomonocytic leukemia: Forefront of the field in 2015 |journal=Crit. Rev. Oncol. Hematol. |volume=95 |issue=2 |pages=222–42 |date=August 2015 |pmid=25869097 |pmc=4859155 |doi=10.1016/j.critrevonc.2015.03.002 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infections]]</small> | |||
* <small>[[Bone]] [[pain]]</small> | |||
* <small>[[Leukemia Cutis]]</small> | |||
| | |||
* <small>[[Organomegaly]]</small> | |||
* <small>[[Bruising]]</small> | |||
|↑ | |||
| <small>< 20%</small> | |||
| | |||
|<small>NL</small> | |||
|<small>[[Eosinophilia|↑]]</small> | |||
|↑↑ | |||
| | |||
* <small>↑ [[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Myelodysplastic]] and [[myeloproliferative]] feature</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Overlapping of both, [[MDS]] and [[MPN]]</small> | |||
* <small>Absolute [[monocytosis]] > 1 × 10<sup>9</sup>/L (defining feature)</small> | |||
* <small>MD-CMML:</small><small>[[WBC]] ≤ 13 × 10<sup>9</sup>/L (FAB)</small> | |||
* <small> MP-CMML:</small><small>[[WBC]] > 13 × 10<sup>9</sup>/L</small> <small>(FAB)</small> | |||
|- | |||
|<small>[[Atypical chronic myeloid leukemia]] (aCML), [[BCR/ABL|BCR-ABL]]1-</small><ref name="pmid26637732">{{cite journal |vauthors=Dao KH, Tyner JW |title=What's different about atypical CML and chronic neutrophilic leukemia? |journal=Hematology Am Soc Hematol Educ Program |volume=2015 |issue= |pages=264–71 |date=2015 |pmid=26637732 |pmc=5266507 |doi=10.1182/asheducation-2015.1.264 |url=}}</ref><ref name="pmid22289493">{{cite journal |vauthors=Muramatsu H, Makishima H, Maciejewski JP |title=Chronic myelomonocytic leukemia and atypical chronic myeloid leukemia: novel pathogenetic lesions |journal=Semin. Oncol. |volume=39 |issue=1 |pages=67–73 |date=February 2012 |pmid=22289493 |pmc=3523950 |doi=10.1053/j.seminoncol.2011.11.004 |url=}}</ref> | |||
|<small> | |||
*Asymptomatic</small> | |||
* Constitutional | |||
* [[Hyperviscosity|Hyperviscosity]] and/or [[anemia]] related | |||
* [[Bleeding|Bleeding]] | |||
* [[Infection|Infection]] | |||
|<small> | |||
* [[Splenomegaly]]</small> (46–76%) | |||
* [[Purpura]] | |||
* [[Anemia]] related | |||
* [[Priapism]] | |||
|↑ | |||
|<small><20%</small> | |||
| + | |||
|<small><2% of WBCs</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
| | |||
* <small>N/A</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Granulocytic [[hyperplasia]] with prominent [[dysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Granulocytic [[dysplasia]] is prominent</small> | |||
* <small>Absence of ''[[BCR/ABL|BCR-ABL]]'' or ''PDGFRA'', [[PDGFRB|''PDGFRB'',]] or ''[[FGFR1]]'' rearrangements</small> | |||
* <small>[[WBC]] > 13 × 10<sup>9</sup>/L</small> | |||
|- | |||
|<small>[[Juvenile myelomonocytic leukemia (patient information)|Juvenile myelomonocytic leukemia (]]JMML)</small><ref name="pmid9226148">{{cite journal |vauthors=Aricò M, Biondi A, Pui CH |title=Juvenile myelomonocytic leukemia |journal=Blood |volume=90 |issue=2 |pages=479–88 |date=July 1997 |pmid=9226148 |doi= |url=}}</ref><ref name="pmid80255132">{{cite journal |vauthors=Hasle H |title=Myelodysplastic syndromes in childhood--classification, epidemiology, and treatment |journal=Leuk. Lymphoma |volume=13 |issue=1-2 |pages=11–26 |date=March 1994 |pmid=8025513 |doi=10.3109/10428199409051647 |url=}}</ref> | |||
| | |||
* <small>[[Infections]]</small> | |||
* <small>[[Anemia]] related</small> | |||
| | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Rash]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
|<small>[[Monocytosis|↑]]</small> | |||
| | |||
* <small>↓ [[Serum]] [[Iron]]</small> | |||
* <small>↑ [[Vitamin B12|B12]] levels</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercelluar with ↑ [[myeloid cells]] in stages of maturation</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Polyclonal [[hypergammaglobulinemia]]</small> | |||
|- | |||
|<small>[[MDS]]/[[MPN]] with ring sideroblasts and [[thrombocytosis]] (MDS/MPN-RS-T)</small><ref name="pmid28188970">{{cite journal |vauthors=Patnaik MM, Tefferi A |title=Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis (RARS-T): 2017 update on diagnosis, risk-stratification, and management |journal=Am. J. Hematol. |volume=92 |issue=3 |pages=297–310 |date=March 2017 |pmid=28188970 |doi=10.1002/ajh.24637 |url=}}</ref><ref name="pmid30186759">{{cite journal |vauthors=Alshaban A, Padilla O, Philipovskiy A, Corral J, McAlice M, Gaur S |title=Lenalidomide induced durable remission in a patient with MDS/MPN-with ring sideroblasts and thrombocytosis with associated 5q- syndrome |journal=Leuk Res Rep |volume=10 |issue= |pages=37–40 |date=2018 |pmid=30186759 |doi=10.1016/j.lrr.2018.08.001 |url=}}</ref><ref name="pmid30524760">{{cite journal |vauthors=Bouchla A, Papageorgiou SG, Tsakiraki Z, Glezou E, Pavlidis G, Stavroulaki G, Bazani E, Foukas P, Pappa V |title=Plasmablastic Lymphoma in an Immunocompetent Patient with MDS/MPN with Ring Sideroblasts and Thrombocytosis-A Case Report |journal=Case Rep Hematol |volume=2018 |issue= |pages=2525070 |date=2018 |pmid=30524760 |pmc=6247723 |doi=10.1155/2018/2525070 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Thrombosis]]</small> | |||
| | |||
* <small>Variable</small> | |||
|<small>NL or ↑</small> | |||
|<small>NL</small> | |||
| - | |||
|<small>NL</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
| | |||
* ↑ <small>[[Serum]] [[Iron]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytosis|↑]]</small> | |||
| | |||
* <small>Hypercellularity with [[dyserythropoiesis]] and increased [[megakaryocytes]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Large atypical [[megakaryocytes]]</small> | |||
* <small>Ringed [[sideroblasts]]</small> | |||
* <small>[[SF3B1]] [[mutation]]</small> | |||
|- | |||
| rowspan="3" |T-lymphoblastic leukemia/<br>lymphoma | |||
* | |||
* | |||
|<small>T-lymphoblastic leukemia/<br>lymphoma</small><ref name="pmid26276771">{{cite journal |vauthors=You MJ, Medeiros LJ, Hsi ED |title=T-lymphoblastic leukemia/lymphoma |journal=Am. J. Clin. Pathol. |volume=144 |issue=3 |pages=411–22 |date=September 2015 |pmid=26276771 |doi=10.1309/AJCPMF03LVSBLHPJ |url=}}</ref><ref name="pmid19284608">{{cite journal |vauthors=Patel KJ, Latif SU, de Calaca WM |title=An unusual presentation of precursor T cell lymphoblastic leukemia/lymphoma with cholestatic jaundice: case report |journal=J Hematol Oncol |volume=2 |issue= |pages=12 |date=March 2009 |pmid=19284608 |pmc=2663564 |doi=10.1186/1756-8722-2-12 |url=}}</ref><ref name="pmid24822133">{{cite journal |vauthors=Elreda L, Sandhu M, Sun X, Bekele W, Cohen AJ, Shah M |title=T-cell lymphoblastic leukemia/lymphoma: relapse 16 years after first remission |journal=Case Rep Hematol |volume=2014 |issue= |pages=359158 |date=2014 |pmid=24822133 |pmc=4005062 |doi=10.1155/2014/359158 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>>25% [[Blast|blasts]] ([[Leukemia]])</small> | |||
<small><25% [[Blast|blasts]] ([[Lymphoma]])</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
* <small>Positive for TdT</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Hypercelluarity with increased [[T cells]] precursors</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small><small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>May involve [[brain]], [[skin]], and [[testes]].</small> | |||
|- | |||
|<small>Provisional entity: Natural killer (NK) cell lymphoblastic leukemia/lymph</small><ref name="pmid28868017">{{cite journal |vauthors=Sedick Q, Alotaibi S, Alshieban S, Naheet KB, Elyamany G |title=Natural Killer Cell Lymphoblastic Leukaemia/Lymphoma: Case Report and Review of the Recent Literature |journal=Case Rep Oncol |volume=10 |issue=2 |pages=588–595 |date=2017 |pmid=28868017 |doi=10.1159/000477843 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>N/A</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[FISH]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Similar to [[T-cell]] lymphoblastic [[leukemia]] but may have more aggressive clinical course.</small> | |||
* <small>[[Diagnosis]] is usually based on presence of [[CD56]] expression, and [[T-cell]]-associated markers such as [[CD2]] and [[CD7]].</small> | |||
* <small>[[B cell|B-cell]] markers are absent.</small> | |||
|- | |||
|<small>Provisional entity: Early T-cell precursor lymphoblastic leukemia</small><ref name="pmid26747249">{{cite journal |vauthors=Jain N, Lamb AV, O'Brien S, Ravandi F, Konopleva M, Jabbour E, Zuo Z, Jorgensen J, Lin P, Pierce S, Thomas D, Rytting M, Borthakur G, Kadia T, Cortes J, Kantarjian HM, Khoury JD |title=Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype |journal=Blood |volume=127 |issue=15 |pages=1863–9 |date=April 2016 |pmid=26747249 |pmc=4915808 |doi=10.1182/blood-2015-08-661702 |url=}}</ref><ref name="pmid23695450">{{cite journal |vauthors=Haydu JE, Ferrando AA |title=Early T-cell precursor acute lymphoblastic leukaemia |journal=Curr. Opin. Hematol. |volume=20 |issue=4 |pages=369–73 |date=July 2013 |pmid=23695450 |pmc=3886681 |doi=10.1097/MOH.0b013e3283623c61 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Hypercelluarity with increased [[T cells]] precursors</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[FISH]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Similar to [[T cell|T-cell]] lymphoblastic [[leukemia]] but is more aggressive clinically and cell are characterized by [[Flow cytometry|cytometry]] as [[CD1a]]<sup>−</sup>, [[CD8]]<sup>−</sup>, [[CD5]]<sup>−</sup> (dim), and positivity for 1 or more stem cell or [[myeloid]] [[antigens]].</small> | |||
* <small>[[Gene expression]] indicates more immature [[cells]] as compared to other subtypes of [[T cell|T-cell]] [[neoplasms]].</small> | |||
|} | |||
==References== | ==References== | ||
| Line 27: | Line 825: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Hematology]] | |||
[[Category:Immunology]] | |||
Latest revision as of 20:34, 27 February 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Hannan Javed, M.D.[2] Badria Munir M.B.B.S.[3] Mohamad Alkateb, MBBCh [4] "sandbox:SN"
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief:
Overview
Pernicious anemia (also called Addison's anemia) is a type of red blood cell disorder caused by impaired vitamin B12 metabolism. Vitamin B12 is primarily absorbed by the small intestine, after being bound to intrinsic factor secreted by parietal cells of gastric mucosa. When this process is disrupted by conditions like atrophic gastritis, celiac disease, small bowel resection etc, B12 deficiency ensues.
Historical perspective
- Pernicious anemia was first discovered by Thomas Addison, hence it is also known as addison's anemia.
- Loss of life from large volume blood loss in the people fighting in the first world war inspired George Whipple to investigate blood forming components such as arsenic, iron pills etc, but found liver to be the most effective. He bled dogs until they had clinical anemia and fed them cooked liver which showed an improvement in symptoms and hematopoeisis. [1]
- In 1948, Smith, Rickles et al., isolated the anti-pernicious factor from liver extract and named it Vitamin B12. They showed that even small amounts of this factor can be used to treat and to prevent pernicious anemia. [2]
Pathophysiology
Vitamin B12 is an essential vitamin for humans and animals because we cannot synthesise it on our own. B12 is a cofactor in DNA synthesis and other important biochemical reactions. Vitamin B12 deficiency manifests as anemia because hematopoetic stem cells in the bone marrow which are rapidly dividing need B12 for division and DNA production. This process is impaired leading to ineffective hematopoeisis. Vitamin B12 is also necessary for production of myelin which is an important component in the covering sheath of nerves. Deficiency results in improper nerve conduction due to nerve destabilisation. [3]
Physiology
- Vitamin B12 is also called cobalamin because it contains cobalt at the core of its structure. Dietary sources of vitamin B12 include meat, fish and eggs.[4]
- When consumed through its dietary source, B12 is bound to protein till it enters the stomach.
- In the stomach, B12 is uncoupled from its carrier protein due to the presence of gastric acid, which is why vitamin B12 deficiency is so commonly seen among those on chronic antacid medication. [5]
- Once in the stomach, it is then bound to gastric R binder, a glycoprotein secreted by the salivary glands till it reaches the duodenum.[6]
- In the duodenum and jejunum, the pancreatic enzymes digest the gastric R binder and cobalamin is bound to intrinsic factor (IF).
- Intrinsic factor is secreted by the gastric parietal cells. Once bound to IF, vitamin B12 travels up to the ileum where IF is removed and B12 binds with carrier proteins called transcobalamins and this complex is taken up by the liver and bone marrow, among other tissues.
- Inside the cells, the transcobalamin-B12 complex is dissolved and cobalamin is reduced to methylcobalamin which serves as a cofactor and coenzyme in many important biochemical reactions[7].
The two major reactions involving B12 in the human body are:
- Vitamin B12 in the from of cyanocobalamin is required in the synthesis of methionine. Methionine is produced from homocysteine and is catalysed by the enzyme methionine synthase. This enzyme utilises cyanocobalamin as a cofactor. Deficiency of vitamin B12 causes a decreased production of methionine and buildup of homocysteine. Hyperhomocysteinemia is implicated as a risk factor in cardiovascular disease.[8]
- The Kreb's cycle utilises vitamin B12 in the reaction converting methylmalonyl-CoA to succinyl-CoA. Thus vitamin B12 deficiency causes a buildup of methylmalonic acid, the substrate for the enzyme methylmalonyl coenzyme A mutase. Methylmalonic acid levels are elevated in the urine of people affected with pernicious anemia and other forms of B12 deficiency.
Storage
The human body can store anywhere from 2-5mg of vitamin B12. Most of this is stored in the liver and is recycled via enterohepatic circulation.
Pathogenesis
Pernicious anemia is a type of megaloblastic anemia caused due to improper vitamin B12 absorption by the body. Impaired absorption occurs because of deficiency of intrinsic factor which is produced by the parietal cells of the stomach. The etiology of pernicious anemia can be due to autoimmune causes or genetic disease. In autoimmune disease, the antibodies attack most of the gastric mucosa, but the antrum is spared.
Autoimmune causes of pernicious anemia
This is the most common cause of pernicious anemia. In autoimmune pernicious anemia, the body produces antibodies against parietal cells or intrinsic factor.
- Antibodies against parietal cells of the gastric mucosa work to inhibit the H+/K(+)-ATPase which is the proton pump present in the parietal cells. The proton pump serves as an auto antigen and activates the cytotoxic CD4+ T cells which proceed to destroy gastric mucosal cells.[9][10]
- Intrinsic factor antibodies are present in fewer cases of pernicious anaemia but are highly specific. There are 2 types of IF antibodies. They prevent the binding and absorption of cobalamin in the ileum via its receptor.[11]
Clinical features
- The symptoms of pernicious anemia take months, and often years to manifest. Patients most commonly present with symptoms of anemia like lightheadedness, dizziness, shortness of breath etc. The population affected with pernicious anemia is usually the elderly (>60 years) owing to its insidious onset.
- Pernicious anemia has hematological, gastrointestinal and neurological manifestations.
- Hematological signs are the earliest manifestation of the disease while neurological signs are seen much later.
- Patients with pernicious anemia usually have very low levels of hydrochloric acid in the stomach (achlorhydria) and high levels on gastrin (hypergastrinemia).
Differentiating pernicious anemia from other diseases
Pernicious anemia shares many similarities with other forms of megaloblastic anemia like B12 and folate deficiency.
- Vitamin B12 deficiency due to insufficient intake (eg veganism) has all the features of pernicious anemia like megaloblasts, hypersegmented neutrophils, neuropsychiatric manifestations. But atrophic gastritis is absent, so achlorhydria, parietal cell antibodies or IF antibodies are absent. Intrinsic factor levels are also normal.[6]
- Folic acid deficiency also results in megaloblastic anemia and similar hematological changes as pernicious anemia, but urinary excretion of methylmalonic acid is absent, so are features of pernicious anemia like achlorhydria, antibodies and normal IF levels.
- Ileal resection causes B12 deficiency due to decreased absorption.
- Certain drugs such as methotrexate, azathioprine cause folate deficiency and result in megaloblastic anemia. This is usually seen in patients taking chemotherapy or other chronic conditions such as rheumatoid arthritis. [12]
- Chronic proton pump inhibitor therapy also results in B12 deficiency as vitamin B12 cannot dissociate from its carrier protein in the absence of an acidic environment.[13]
- Long term use of metformin, such as in diabetics, is linked to vitamin B12 deficiency and symptoms similar to pernicious anemia, but this can be differentiated from pernicious anemia as it is seen in diabetics on chronic therapy.[14]
Associated Conditions
People affected with pernicious anemia might have other coexisting autoimmune conditions such as autoimmune thyroiditis, autoimmune diabetes, vitiligo etc. Autoimmune thyroiditis is most commonly seen in patients with pernicious anemia, particularly females. HLA DR3 has been implicated in the development of autoimmune diseases such as pernicious anemia[15].
Epidemiology and demographics
- Pernicious anemia is a disease of the elderly. The mean age of patients who are symptomatic is >60.[16]
- An exception is the genetic form of the disease which is a congenital deficiency of intrinsic factor and is seen in children <10 years of age.
- Men and women are equally affected
- Prevalence of pernicious anemia is estimated at 0.1% of the population.[17]
Genetics
- Some forms of pernicious anemia are congenital and a genetic link has been postulated because of a higher incidence in certain populations.
- Affected people have a complete or near total absence of intrinsic factor and the presence of antibodies against intrinsic factor.
- The genetic variant is transmitted through an autosomal recessive pattern.[18]
Risk factors
- People who have autoimmune conditions like diabetes mellitus, autoimmune thyroiditis are at higher risk of developing pernicious anemia.
Natural History, Complications and Prognosis
- In most cases, patients affected with pernicious anemia remain asymptomatic for many years.
- Early manifestations include fatigue, shortness of breath, pallor and weakness.
- Long standing untreated pernicious anemia results in irreversible neurological damage such as subacute combined degeneration of the spinal cord.
- Neurological changes are irreversible once they set in and do not resolve with cobalamin supplementation.
Diagnosis
A diagnosis of pernicious anemia is made by a history and physical examination, along with hematological and neurological examination.
Diagnostic criteria
- The only specific criteria to diagnose pernicious anemia is an intrinsic factor output of less than 200U/h after pentagastrin stimulation, where normal levels would be >2000U/h. [19]
Symptoms
Symptoms of pernicious anemia are summarised below
| Hematological symptoms | Gastrointestinal symptoms | Neurological symptoms |
|---|---|---|
| Fatigue | Loss of appetite | Parasthesias |
| Weakness | Weight loss
|
Depression |
| Shortness of breath | Nausea | Gait problems |
| Dizziness | Burning sensation on tongue | Weakness |
| Tachycardia | Diarrhea | Loss of balance |
| Lightheadedness | Vomiting | Confusion |
Physical examination findings
Most important physical examination findings are the neurological findings of long standing B12 deficiency which leads to subacute combined degeneration of the spinal cord.
- Hematological signs include pallor and icterus.[20]
- Neurological signs: Vitamin B12 deficiency causes nerve demyelination. B12 deficiency also causes a buildup of methylmalonic acid which is toxic to neuronal cells and causes apoptosis.[21].
The main neurological manifestation of pernicious anemia and vitamin B12 deficiency is subacute combined degeneration. The posterior and lateral columns of the spinal cord are affected. Lateral column demyelination manifests as hyperreflexia and spasticity, while posterior column defects are loss of proprioception and vibration sense. Ataxia and loss of tandem gait are also manifestations of posterior column demyelination. Recreational or accidental inhalation of nitrous oxide gas (laughing gas) can precipitate subacute combined degeneration in people with low levels of vitamin B12.[22]
- Gastrointestinal signs: Upto 25% of people affected with pernicious anemia develop glossitis. The tongue appears red, "beefy" and smooth due to atrophy and blunting of the lingual papillae.[23]
Subacute combined degeneration

Laboratory findings
- The first step in diagnosis is a blood vitamin B12 level. Blood levels less than 200 pg/ml are seen in pernicious anemia.
- Intrinsic factor antibodies and Parietal cell antibodies.
- Low intrinsic factor level.[24]
- Gastric mucosal sampling shows parietal cell atrophy with antral sparing.[25]
- Increased level of gastrin.
- Increased levels of homocysteine and methylmalonyl-CoA.
- Decreased folate levels are seen due to "folate trapping" in the form of methyltetrahydrofolate.
Shilling Test
The Shilling test is no longer done to detect an IF deficiency but has historical importance. After a vitamin B12 deficiency is noted, the patient is given radioactively tagged cobalamin to take orally. Soon after this step, the patient is injected with unlabelled cobalamin intramuscularly. Urine is checked for radioactive cobalamin for the next 24 hours. In pernicious anemia, there is an intrinsic factor deficiency, therefore the orally consumed radioactive cobalamin will not be absorbed and can be detected in the urine. In the next step, the patient is given radioactive cobalamin along with intrinsic factor and their urine is checked for traces of radioactive cobalamin. Absence of radioactive cobalamin in the urine points to the deficiency of intrinsic factor in the patients stomach which is the cause of vitamin B12 deficiency[26]. If the cobalamin absorption does not increase even with intrinsic factor supplementation, patient can be given a course of antibiotics as bacterial overgrowth may hinder absorption.
Peripheral smear findings
- The most obvious peripheral smear finding is megaloblasts and macrocytes.
Megaloblastic anemia results due to the lagging behind of nuclear development when compared to cytoplasmic development. This is known as nuclear-cytoplasmic asynchrony. Such defective cells are destroyed in the bone marrow (intramedullary hemolysis).
- Decreased number of RBCs (erythopenia)
- Macrocytosis- the RBCs in pernicious anemia are very large. Macrocytosis is defined as cells that have an MCV >100 femtolitres (normal :80-100fL)
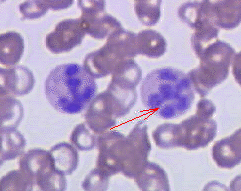
- Hypersegmented neutrophils : Neutrophils containing ≥ 6 lobes. [27]
- Poikilocytosis and anisocytosis
- Low reticulocyte count (reticulopenia)
- Howell-Jolly bodies
-
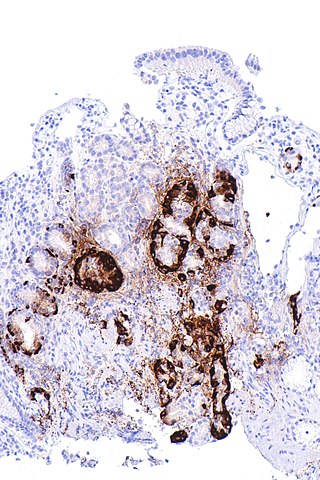
Atrophic gastritis
-
Hypersegmented neutrophil
Treatment
- Standard treatment for pernicious anemia is replacement of cobalamin via intramuscular injection. [28]
- 1000 mcg IM everyday for one week, followed by weekly injections the next month and then monthly once injections.
- Response to treatment is measured by an increase in reticulocyte count within 5 days of starting therapy.
- Patient also experience a sense of wellbeing shortly after beginning therapy.
- If reticulocytosis is not observed within the first week of therapy, other factors such as hypothyroidism, folate deficiency should be considered.
- Intramuscular therapy can be replaced by high dose oral therapy.[17]
- Neurological disease always warrants parenteral treatment.
- Within the first 3-4 weeks of treatment, marrow changes revert and there is resolution in macrocytosis.
- Most patients require lifelong monthly therapy.
- Routine follow up should be done with a CBC every few months.
- A small percentage of patients develop gastric carcinoma, particularly in the elderly. Regular surveillance helps in early detection and treatment. [29]
Prevention
- There is no primary preventive measure for pernicious anemia.
- Once sucessfully diagnosed and treated, patients with pernicious anemia are followed up every year for development of stomach cancer[30], or symptoms of anemia.
==References== Syed Hassan A. Kazmi BSc, MD [6]
Overview
Chronic myelogenous leukemia must be differentiated from leukemoid reaction, chronic neutrophilic leukemia, and acute myeloid leukemia.
Differential Diagnosis
Chronic myelogenous leukemia must be differentiated from:[31][32][33][34][35][36][37][38][39][40][41][31]
- Leukemoid reaction
- Basophils and eosinophils are almost always increased in chronic myelogenous leukemia
- Chronic neutrophilic leukemia
- Acute myeloid leukemia
- Thrombocytosis
- Chronic lymphoid leukemia
- Acute myeloid leukemia
- Juvenile myelomonocytic leukemia
- Chronic myelomonocytic leukemia
- Atypical CML
- Chronic eosinophilic leukemia
- Polycythemia vera
- Essential thrombocytosis
- The following table differentiates chronic myelogenous leukemia from other leukemias that may present with similar clinical features such as fever, fatigue, weight loss, recurrent infections and elevated leukocyte counts. The following are the differentials:
Differentiating Myeloproliferative Disorders
ABBREVIATIONS
N/A: Not available, NL: Normal, FISH: Fluorescence in situ hybridization, PCR: Polymerase chain reaction, LDH: Lactate dehydrogenase, PUD: Peptic ulcer disease, EPO: Erythropoietin, LFTs: Liver function tests, RFTs: Renal function tests, LAP: Leukocyte alkaline phosphatase, LAD: Leukocyte alkaline dehydrgenase, WBCs: White blood cells.
| Myeloproliferative neoplasms (MPN) | Clinical manifestations | Diagnosis | Other features | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | CBC & Peripheral smear | Bone marrow biopsy | Other investigations | |||||||||||
| WBCs | Hb | Plat- elets | |||||||||||||
| Leuko-cytes | Blasts | Left shift |
Baso- phils |
Eosino- phils |
Mono- cytes |
Others | |||||||||
| Chronic myeloid leukemia (CML), BCR-ABL1+[42][43] |
|
|
↑ | <2% | + | ↑ | ↑ | ↑ | N/A | ↓ | NL |
|
|
| |
| Chronic neutrophilic leukemia (CNL)[44][45][46] |
|
↑ | Minimal | + | NL | NL | NL | ↓ | ↓ |
|
|
| |||
| Polycythemia vera (PV)[47][48][49][50] |
|
|
NL or ↑ | None | - | ↑ or ↓ | NL or ↑ | NL | ↑↑ | NL |
|
| |||
| Primary myelofibrosis (PMF)[51][52][53][54] |
|
↓ | Erythroblasts | - | Absent | NL | NL | ↓ | ↓ |
|
| ||||
| Essential thrombocythemia (ET)[55][56][57] |
|
NL or ↑ |
None |
- |
↓ or absent |
NL |
NL |
|
↑↑ |
|
|||||
| Chronic eosinophilic leukemia, not otherwise specified (NOS)[58][59][60][61] |
|
↑ | Present | + | ↑ | ↑↑ | ↑ | ↓ | ↓ |
|
|
||||
| MPN, unclassifiable |
|
|
↑ | Variable | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↑ |
|
|
| |
| Mastocytosis[62][63][64][65] |
|
↑ | None | - | NL | ↑ | NL | ↓ | ↓ or ↑ |
|
| ||||
| Myeloid/lymphoid neoplasms with eosinophilia and rearrangement of PDGFRA, PDGFRB, or FGFR1, or with PCM1-JAK2[66][67][68][69] |
|
↑ | NL | - | NL | ↑ | ↑ |
|
NL | ↓ |
|
|
| ||
| B-lymphoblastic leukemia/lymphoma[70][71] | NL or ↑ | >25% | N/A | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ | ↓ | ↓ |
|
| |||||
| Myelodysplastic syndromes (MDS)[72][73] |
↓ | Variable | - | ↓ | ↓ | ↓ |
|
↓ | ↓ |
|
| ||||
| Acute myeloid leukemia (AML) and related neoplasms[74][75] |
|
|
NL or ↑ | ↑ | N/A | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
with dysplasia |
| ||
| Blastic plasmacytoid dendritic cell neoplasm[76][77][78][79] |
|
|
NL | ↑ | NL | NL | NL | ↓ | ↓ |
|
| ||||
| Myelodysplastic /myeloproliferative neoplasms (MDS/MPN) |
Chronic myelomonocytic leukemia (CMML)[80] |
|
↑ | < 20% | NL | ↑ | ↑↑ |
|
↓ | ↓ |
|
| |||
| Atypical chronic myeloid leukemia (aCML), BCR-ABL1-[83][84] |
|
|
↑ | <20% | + | <2% of WBCs | N/A | N/A |
|
↓ | ↓ |
|
|||
| Juvenile myelomonocytic leukemia (JMML)[85][86] |
|
↑ | ↑ | N/A | N/A | N/A | ↑ | ↓ | ↓ |
|
| ||||
| MDS/MPN with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T)[87][88][89] |
|
|
NL or ↑ | NL | - | NL | N/A | N/A | ↓ | ↑ |
|
| |||
| T-lymphoblastic leukemia/ lymphoma |
T-lymphoblastic leukemia/ lymphoma[90][91][92] |
|
↑ | >25% blasts (Leukemia) | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
|||
| Provisional entity: Natural killer (NK) cell lymphoblastic leukemia/lymph[93] |
|
↑ | ↑ | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
||||
| Provisional entity: Early T-cell precursor lymphoblastic leukemia[94][95] |
|
↑ | ↑ | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
||||
References
- ↑ Sinclair L (2008). "Recognizing, treating and understanding pernicious anaemia". J R Soc Med. 101 (5): 262–4. doi:10.1258/jrsm.2008.081006. PMC 2376267. PMID 18463283.
- ↑ SMITH EL (1948). "Purification of anti-pernicious anaemia factors from liver". Nature. 161 (4095): 638. doi:10.1038/161638a0. PMID 18856623.
- ↑ Miles LM, Allen E, Clarke R, Mills K, Uauy R, Dangour AD (2017). "Impact of baseline vitamin B12 status on the effect of vitamin B12 supplementation on neurologic function in older people: secondary analysis of data from the OPEN randomised controlled trial". Eur J Clin Nutr. 71 (10): 1166–1172. doi:10.1038/ejcn.2017.7. PMID 28225050.
- ↑ Watanabe F (2007). "Vitamin B12 sources and bioavailability". Exp Biol Med (Maywood). 232 (10): 1266–74. doi:10.3181/0703-MR-67. PMID 17959839.
- ↑ Jung SB, Nagaraja V, Kapur A, Eslick GD (2015). "Association between vitamin B12 deficiency and long-term use of acid-lowering agents: a systematic review and meta-analysis". Intern Med J. 45 (4): 409–16. doi:10.1111/imj.12697. PMID 25583062.
- ↑ 6.0 6.1 Del Corral A, Carmel R (1990). "Transfer of cobalamin from the cobalamin-binding protein of egg yolk to R binder of human saliva and gastric juice". Gastroenterology. 98 (6): 1460–6. doi:10.1016/0016-5085(90)91076-i. PMID 2110915.
- ↑ Harrington DJ (2017). "Laboratory assessment of vitamin B12 status". J Clin Pathol. 70 (2): 168–173. doi:10.1136/jclinpath-2015-203502. PMID 27169753.
- ↑ Tinelli C, Di Pino A, Ficulle E, Marcelli S, Feligioni M (2019). "Hyperhomocysteinemia as a Risk Factor and Potential Nutraceutical Target for Certain Pathologies". Front Nutr. 6: 49. doi:10.3389/fnut.2019.00049. PMC 6491750. PMID 31069230.
- ↑ Callaghan JM, Khan MA, Alderuccio F, van Driel IR, Gleeson PA, Toh BH (1993). "Alpha and beta subunits of the gastric H+/K(+)-ATPase are concordantly targeted by parietal cell autoantibodies associated with autoimmune gastritis". Autoimmunity. 16 (4): 289–95. doi:10.3109/08916939309014648. PMID 7517707.
- ↑ Toh BH, Sentry JW, Alderuccio F (2000). "The causative H+/K+ ATPase antigen in the pathogenesis of autoimmune gastritis". Immunol Today. 21 (7): 348–54. doi:10.1016/s0167-5699(00)01653-4. PMID 10871877.
- ↑ Schade SG, Abels J, Schilling RF (1967). "Studies on antibody to intrinsic factor". J Clin Invest. 46 (4): 615–20. doi:10.1172/JCI105563. PMC 442045. PMID 6021209.
- ↑ Green R, Datta Mitra A (2017). "Megaloblastic Anemias: Nutritional and Other Causes". Med Clin North Am. 101 (2): 297–317. doi:10.1016/j.mcna.2016.09.013. PMID 28189172.
- ↑ Heidelbaugh JJ (2013). "Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications". Ther Adv Drug Saf. 4 (3): 125–33. doi:10.1177/2042098613482484. PMC 4110863. PMID 25083257.
- ↑ Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ; et al. (2016). "Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study". J Clin Endocrinol Metab. 101 (4): 1754–61. doi:10.1210/jc.2015-3754. PMC 4880159. PMID 26900641.
- ↑ Zulfiqar AA, Andres E (2017). "Association pernicious anemia and autoimmune polyendocrinopathy: a retrospective study". J Med Life. 10 (4): 250–253. PMC 5771255. PMID 29362601.
- ↑ Carmel R (1996). "Prevalence of undiagnosed pernicious anemia in the elderly". Arch Intern Med. 156 (10): 1097–100. PMID 8638997.
- ↑ 17.0 17.1 Andres E, Serraj K (2012). "Optimal management of pernicious anemia". J Blood Med. 3: 97–103. doi:10.2147/JBM.S25620. PMC 3441227. PMID 23028239.
- ↑ Gordon MM, Brada N, Remacha A, Badell I, del Río E, Baiget M; et al. (2004). "A genetic polymorphism in the coding region of the gastric intrinsic factor gene (GIF) is associated with congenital intrinsic factor deficiency". Hum Mutat. 23 (1): 85–91. doi:10.1002/humu.10297. PMID 14695536.
- ↑ Cattan D (2011). "Pernicious anemia: what are the actual diagnosis criteria?". World J Gastroenterol. 17 (4): 543–4. doi:10.3748/wjg.v17.i4.543. PMC 3027024. PMID 21274387.
- ↑ Seynabou F, Fatou Samba Diago N, Oulimata Diop D, Abibatou Fall S, Nafissatou D (2016). "Biermer anemia: Hematologic characteristics of 66 patients in a Clinical Hematology Unit at Senegal". Med Sante Trop. 26 (4): 402–407. doi:10.1684/mst.2016.0625. PMID 28073728.
- ↑ Han L, Wu S, Han F, Gu X (2015). "Insights into the molecular mechanisms of methylmalonic acidemia using microarray technology". Int J Clin Exp Med. 8 (6): 8866–79. PMC 4538064. PMID https://www.ncbi.nlm.nih.gov/pubmed/26309541 Check
|pmid=value (help). - ↑ Choi C, Kim T, Park KD, Lim OK, Lee JK (2019). "Subacute Combined Degeneration Caused by Nitrous Oxide Intoxication: A Report of Two Cases". Ann Rehabil Med. 43 (4): 530–534. doi:10.5535/arm.2019.43.4.530. PMC 6734019 Check
|pmc=value (help). PMID 31499607. - ↑ Stoopler ET, Kuperstein AS (2013). "Glossitis secondary to vitamin B12 deficiency anemia". CMAJ. 185 (12): E582. doi:10.1503/cmaj.120970. PMC 3761039. PMID 23359038.
- ↑ Lahner E, Annibale B (2009). "Pernicious anemia: new insights from a gastroenterological point of view". World J Gastroenterol. 15 (41): 5121–8. doi:10.3748/wjg.15.5121. PMC 2773890. PMID 19891010.
- ↑ Korman MG, Strickland RG, Hansky J (1972). "The functional 'G' cell mass in atrophic gastritis". Gut. 13 (5): 349–51. doi:10.1136/gut.13.5.349. PMC 1412218. PMID 5036089.
- ↑ "StatPearls". 2020. PMID 29939561.
- ↑ Farrelly SJ, O'Connor KA (2017). "Hypersegmented neutrophils and oval macrocytes in the setting of B12 deficiency and pancytopaenia". BMJ Case Rep. 2017. doi:10.1136/bcr-2016-218508. PMC 5612428. PMID 28821482.
- ↑ Annibale B, Lahner E, Fave GD (2011). "Diagnosis and management of pernicious anemia". Curr Gastroenterol Rep. 13 (6): 518–24. doi:10.1007/s11894-011-0225-5. PMID 21947876.
- ↑ Murphy G, Dawsey SM, Engels EA, Ricker W, Parsons R, Etemadi A; et al. (2015). "Cancer Risk After Pernicious Anemia in the US Elderly Population". Clin Gastroenterol Hepatol. 13 (13): 2282-9.e1-4. doi:10.1016/j.cgh.2015.05.040. PMC 4655146. PMID 26079040.
- ↑ Venerito M, Link A, Rokkas T, Malfertheiner P (2016). "Gastric cancer - clinical and epidemiological aspects". Helicobacter. 21 Suppl 1: 39–44. doi:10.1111/hel.12339. PMID 27531538.
- ↑ 31.0 31.1 Gajendra S, Gupta R, Chandgothia M, Kumar L, Gupta R, Chavan SM (2014). "Chronic Neutrophilic Leukemia with V617F JAK2 Mutation". Indian J Hematol Blood Transfus. 30 (2): 139–42. doi:10.1007/s12288-012-0203-6. PMC 4022913. PMID 24839370.
- ↑ Kanegae MP, Ximenes VF, Falcão RP, Colturato VA, de Mattos ER, Brunetti IL; et al. (2007). "Chemiluminescent determination of leukocyte alkaline phosphatase: an advantageous alternative to the cytochemical assay". J Clin Lab Anal. 21 (2): 91–6. doi:10.1002/jcla.20140. PMID 17385676.
- ↑ Jabbour E, Kantarjian H (2014). "Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management". Am J Hematol. 89 (5): 547–56. doi:10.1002/ajh.23691. PMID 24729196.
- ↑ Niemeyer CM, Kratz C (November 2003). "Juvenile myelomonocytic leukemia". Curr Oncol Rep. 5 (6): 510–5. PMID 14521811.
- ↑ Hernández JM, del Cañizo MC, Cuneo A, García JL, Gutiérrez NC, González M, Castoldi G, San Miguel JF (April 2000). "Clinical, hematological and cytogenetic characteristics of atypical chronic myeloid leukemia". Ann. Oncol. 11 (4): 441–4. PMID 10847463.
- ↑ Oliver JW, Deol I, Morgan DL, Tonk VS (December 1998). "Chronic eosinophilic leukemia and hypereosinophilic syndromes. Proposal for classification, literature review, and report of a case with a unique chromosomal abnormality". Cancer Genet. Cytogenet. 107 (2): 111–7. PMID 9844604.
- ↑ Bain BJ (October 1996). "Eosinophilic leukaemias and the idiopathic hypereosinophilic syndrome". Br. J. Haematol. 95 (1): 2–9. PMID 8857931.
- ↑ Krämer A (October 2008). "JAK2-V617F and BCR-ABL--double jeopardy?". Leuk. Res. 32 (10): 1489–90. doi:10.1016/j.leukres.2008.03.011. PMID 18439674.
- ↑ Elliott MA (May 2004). "Chronic neutrophilic leukemia: a contemporary review". Curr. Hematol. Rep. 3 (3): 210–7. PMID 15087070.
- ↑ Gotlib J, Maxson JE, George TI, Tyner JW (September 2013). "The new genetics of chronic neutrophilic leukemia and atypical CML: implications for diagnosis and treatment". Blood. 122 (10): 1707–11. doi:10.1182/blood-2013-05-500959. PMC 3765056. PMID 23896413.
- ↑ Westbrook CA, Hooberman AL, Spino C, Dodge RK, Larson RA, Davey F, Wurster-Hill DH, Sobol RE, Schiffer C, Bloomfield CD (December 1992). "Clinical significance of the BCR-ABL fusion gene in adult acute lymphoblastic leukemia: a Cancer and Leukemia Group B Study (8762)". Blood. 80 (12): 2983–90. PMID 1467514.
- ↑ Savage DG, Szydlo RM, Goldman JM (January 1997). "Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period". Br. J. Haematol. 96 (1): 111–6. PMID 9012696.
- ↑ Thompson PA, Kantarjian HM, Cortes JE (October 2015). "Diagnosis and Treatment of Chronic Myeloid Leukemia in 2015". Mayo Clin. Proc. 90 (10): 1440–54. doi:10.1016/j.mayocp.2015.08.010. PMC 5656269. PMID 26434969.
- ↑ Szuber N, Tefferi A (February 2018). "Chronic neutrophilic leukemia: new science and new diagnostic criteria". Blood Cancer J. 8 (2): 19. doi:10.1038/s41408-018-0049-8. PMC 5811432. PMID 29440636.
- ↑ Maxson JE, Tyner JW (February 2017). "Genomics of chronic neutrophilic leukemia". Blood. 129 (6): 715–722. doi:10.1182/blood-2016-10-695981. PMC 5301820. PMID 28028025.
- ↑ Menezes J, Cigudosa JC (2015). "Chronic neutrophilic leukemia: a clinical perspective". Onco Targets Ther. 8: 2383–90. doi:10.2147/OTT.S49688. PMC 4562747. PMID 26366092.
- ↑ Vannucchi AM, Guglielmelli P, Tefferi A (March 2018). "Polycythemia vera and essential thrombocythemia: algorithmic approach". Curr. Opin. Hematol. 25 (2): 112–119. doi:10.1097/MOH.0000000000000402. PMID 29194068.
- ↑ Pillai AA, Babiker HM. PMID 30252337. Missing or empty
|title=(help) - ↑ Tefferi A, Barbui T (January 2019). "Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management". Am. J. Hematol. 94 (1): 133–143. doi:10.1002/ajh.25303. PMID 30281843.
- ↑ Rumi E, Cazzola M (February 2017). "Diagnosis, risk stratification, and response evaluation in classical myeloproliferative neoplasms". Blood. 129 (6): 680–692. doi:10.1182/blood-2016-10-695957. PMC 5335805. PMID 28028026.
- ↑ Cervantes F, Correa JG, Hernandez-Boluda JC (May 2016). "Alleviating anemia and thrombocytopenia in myelofibrosis patients". Expert Rev Hematol. 9 (5): 489–96. doi:10.1586/17474086.2016.1154452. PMID 26891375.
- ↑ Hoffman, Ronald (2018). Hematology : basic principles and practice. Philadelphia, PA: Elsevier. ISBN 9780323357623.
- ↑ Michiels JJ, Bernema Z, Van Bockstaele D, De Raeve H, Schroyens W (March 2007). "Current diagnostic criteria for the chronic myeloproliferative disorders (MPD) essential thrombocythemia (ET), polycythemia vera (PV) and chronic idiopathic myelofibrosis (CIMF)". Pathol. Biol. 55 (2): 92–104. doi:10.1016/j.patbio.2006.06.002. PMID 16919893.
- ↑ Hoffman, Ronald (2018). Hematology : basic principles and practice. Philadelphia, PA: Elsevier. ISBN 9780323357623.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID http://dx.doi.org/10.1182/blood-2007-04-083501 Check
|pmid=value (help). - ↑ Daniel A. Arber, Attilio Orazi, Robert Hasserjian, Jurgen Thiele, Michael J. Borowitz, Michelle M. Le Beau, Clara D. Bloomfield, Mario Cazzola & James W. Vardiman (2016). "The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia". Blood. 127 (20): 2391–2405. doi:10.1182/blood-2016-03-643544. PMID 27069254. Unknown parameter
|month=ignored (help) - ↑ A. Tefferi, R. Fonseca, D. L. Pereira & H. C. Hoagland (2001). "A long-term retrospective study of young women with essential thrombocythemia". Mayo Clinic proceedings. 76 (1): 22–28. doi:10.4065/76.1.22. PMID 11155408. Unknown parameter
|month=ignored (help) - ↑ Vidyadharan S, Joseph B, Nair SP (2016). "Chronic Eosinophilic Leukemia Presenting Predominantly with Cutaneous Manifestations". Indian J Dermatol. 61 (4): 437–9. doi:10.4103/0019-5154.185716. PMC 4966405. PMID 27512192.
- ↑ Hofmans M, Delie A, Vandepoele K, Van Roy N, Van der Meulen J, Philippé J, Moors I (2018). "A case of chronic eosinophilic leukemia with secondary transformation to acute myeloid leukemia". Leuk Res Rep. 9: 45–47. doi:10.1016/j.lrr.2018.04.001. PMC 5993353. PMID 29892549.
- ↑ Yamada Y, Rothenberg ME, Cancelas JA (2006). "Current concepts on the pathogenesis of the hypereosinophilic syndrome/chronic eosinophilic leukemia". Transl Oncogenomics. 1: 53–63. PMC 3642145. PMID 23662039.
- ↑ Kim TH, Gu HJ, Lee WI, Lee J, Yoon HJ, Park TS (September 2016). "Chronic eosinophilic leukemia with FIP1L1-PDGFRA rearrangement". Blood Res. 51 (3): 204–206. doi:10.5045/br.2016.51.3.204. PMID 27722133.
- ↑ Carter MC, Metcalfe DD, Komarow HD (February 2014). "Mastocytosis". Immunol Allergy Clin North Am. 34 (1): 181–96. doi:10.1016/j.iac.2013.09.001. PMC 3863935. PMID 24262698.
- ↑ Macri A, Cook C. PMID 29494109. Missing or empty
|title=(help) - ↑ Lladó AC, Mihon CE, Silva M, Galzerano A (2014). "Systemic mastocytosis - a diagnostic challenge". Rev Bras Hematol Hemoter. 36 (3): 226–9. doi:10.1016/j.bjhh.2014.03.003. PMC 4109736. PMID 25031064.
- ↑ Valent P, Akin C, Metcalfe DD (March 2017). "Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts". Blood. 129 (11): 1420–1427. doi:10.1182/blood-2016-09-731893. PMC 5356454. PMID 28031180.
- ↑ Kumar, Kirthi R.; Chen, Weina; Koduru, Prasad R.; Luu, Hung S. (2015). "Myeloid and Lymphoid Neoplasm With Abnormalities of FGFR1 Presenting With Trilineage Blasts and RUNX1 Rearrangement". American Journal of Clinical Pathology. 143 (5): 738–748. doi:10.1309/AJCPUD6W1JLQQMNA. ISSN 1943-7722.
- ↑ Paolo Strati, Guilin Tang, Dzifa Y. Duose, Saradhi Mallampati, Rajyalakshmi Luthra, Keyur P. Patel, Mohammad Hussaini, Abu-Sayeef Mirza, Rami S. Komrokji, Stephen Oh, John Mascarenhas, Vesna Najfeld, Vivek Subbiah, Hagop Kantarjian, Guillermo Garcia-Manero, Srdan Verstovsek & Naval Daver (2018). "Myeloid/lymphoid neoplasms with FGFR1 rearrangement". Leukemia & lymphoma. 59 (7): 1672–1676. doi:10.1080/10428194.2017.1397663. PMID 29119847. Unknown parameter
|month=ignored (help) - ↑ Ximena Montenegro-Garreaud, Roberto N. Miranda, Alexandra Reynolds, Guilin Tang, Sa A. Wang, Mariko Yabe, Wei Wang, Lianghua Fang, Carlos E. Bueso-Ramos, Pei Lin, L. Jeffrey Medeiros & Xinyan Lu (2017). "Myeloproliferative neoplasms with t(8;22)(p11.2;q11.2)/BCR-FGFR1: a meta-analysis of 20 cases shows cytogenetic progression with B-lymphoid blast phase". Human pathology. 65: 147–156. doi:10.1016/j.humpath.2017.05.008. PMID 28551329. Unknown parameter
|month=ignored (help) - ↑ Paola Villafuerte-Gutierrez, Montserrat Lopez Rubio, Pilar Herrera & Eva Arranz (2018). "A Case of Myeloproliferative Neoplasm with BCR-FGFR1 Rearrangement: Favorable Outcome after Haploidentical Allogeneic Transplantation". Case reports in hematology. 2018: 5724960. doi:10.1155/2018/5724960. PMID 30647980.
- ↑ Kamiya-Matsuoka C, Garciarena P, Amin HM, Tremont-Lukats IW, de Groot JF (December 2013). "B lymphoblastic leukemia/lymphoma presenting as seventh cranial nerve palsy". Neurol Clin Pract. 3 (6): 532–534. doi:10.1212/CPJ.0b013e3182a78ef0. PMC 6082360. PMID 30107017.
- ↑ Zhang X, Rastogi P, Shah B, Zhang L (September 2017). "B lymphoblastic leukemia/lymphoma: new insights into genetics, molecular aberrations, subclassification and targeted therapy". Oncotarget. 8 (39): 66728–66741. doi:10.18632/oncotarget.19271. PMC 5630450. PMID 29029550.
- ↑ Germing U, Kobbe G, Haas R, Gattermann N (November 2013). "Myelodysplastic syndromes: diagnosis, prognosis, and treatment". Dtsch Arztebl Int. 110 (46): 783–90. doi:10.3238/arztebl.2013.0783. PMC 3855821. PMID 24300826.
- ↑ Gangat N, Patnaik MM, Tefferi A (January 2016). "Myelodysplastic syndromes: Contemporary review and how we treat". Am. J. Hematol. 91 (1): 76–89. doi:10.1002/ajh.24253. PMID 26769228.
- ↑ Islam A, Catovsky D, Goldman JM, Galton DA (September 1985). "Bone marrow biopsy changes in acute myeloid leukaemia. I: Observations before chemotherapy". Histopathology. 9 (9): 939–57. PMID 3864727.
- ↑ Orazi A (2007). "Histopathology in the diagnosis and classification of acute myeloid leukemia, myelodysplastic syndromes, and myelodysplastic/myeloproliferative diseases". Pathobiology. 74 (2): 97–114. doi:10.1159/000101709. PMID 17587881.
- ↑ F. Julia, T. Petrella, M. Beylot-Barry, M. Bagot, D. Lipsker, L. Machet, P. Joly, O. Dereure, M. Wetterwald, M. d'Incan, F. Grange, J. Cornillon, G. Tertian, E. Maubec, P. Saiag, S. Barete, I. Templier, F. Aubin & S. Dalle (2013). "Blastic plasmacytoid dendritic cell neoplasm: clinical features in 90 patients". The British journal of dermatology. 169 (3): 579–586. doi:10.1111/bjd.12412. PMID 23646868. Unknown parameter
|month=ignored (help) - ↑ Livio Pagano, Caterina Giovanna Valentini, Alessandro Pulsoni, Simona Fisogni, Paola Carluccio, Francesco Mannelli, Monia Lunghi, Gianmatteo Pica, Francesco Onida, Chiara Cattaneo, Pier Paolo Piccaluga, Eros Di Bona, Elisabetta Todisco, Pellegrino Musto, Antonio Spadea, Alfonso D'Arco, Stefano Pileri, Giuseppe Leone, Sergio Amadori & Fabio Facchetti (2013). "Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study". Haematologica. 98 (2): 239–246. doi:10.3324/haematol.2012.072645. PMID 23065521. Unknown parameter
|month=ignored (help) - ↑ Joseph D. Khoury (2018). "Blastic Plasmacytoid Dendritic Cell Neoplasm". Current hematologic malignancy reports. 13 (6): 477–483. doi:10.1007/s11899-018-0489-z. PMID 30350260. Unknown parameter
|month=ignored (help) - ↑ Shinichiro Sukegawa, Mamiko Sakata-Yanagimoto, Ryota Matsuoka, Haruka Momose, Yusuke Kiyoki, Masayuki Noguchi, Naoya Nakamura, Rei Watanabe, Manabu Fujimoto, Yasuhisa Yokoyama, Hidekazu Nishikii, Takayasu Kato, Manabu Kusakabe, Naoki Kurita, Naoshi Obara, Yuichi Hasegawa & Shigeru Chiba (2018). "[Blastic plasmacytoid dendritic cell neoplasm accompanied by chronic myelomonocytic leukemia successfully treated with azacitidine]". [[[Rinsho ketsueki] The Japanese journal of clinical hematology]]. 59 (12): 2567–2573. doi:10.11406/rinketsu.59.2567. PMID 30626790.
- ↑ Patnaik MM, Tefferi A (June 2016). "Chronic myelomonocytic leukemia: 2016 update on diagnosis, risk stratification, and management". Am. J. Hematol. 91 (6): 631–42. doi:10.1002/ajh.24396. PMID 27185207.
- ↑ Parikh SA, Tefferi A (June 2012). "Chronic myelomonocytic leukemia: 2012 update on diagnosis, risk stratification, and management". Am. J. Hematol. 87 (6): 610–9. doi:10.1002/ajh.23203. PMID 22615103.
- ↑ Benton CB, Nazha A, Pemmaraju N, Garcia-Manero G (August 2015). "Chronic myelomonocytic leukemia: Forefront of the field in 2015". Crit. Rev. Oncol. Hematol. 95 (2): 222–42. doi:10.1016/j.critrevonc.2015.03.002. PMC 4859155. PMID 25869097.
- ↑ Dao KH, Tyner JW (2015). "What's different about atypical CML and chronic neutrophilic leukemia?". Hematology Am Soc Hematol Educ Program. 2015: 264–71. doi:10.1182/asheducation-2015.1.264. PMC 5266507. PMID 26637732.
- ↑ Muramatsu H, Makishima H, Maciejewski JP (February 2012). "Chronic myelomonocytic leukemia and atypical chronic myeloid leukemia: novel pathogenetic lesions". Semin. Oncol. 39 (1): 67–73. doi:10.1053/j.seminoncol.2011.11.004. PMC 3523950. PMID 22289493.
- ↑ Aricò M, Biondi A, Pui CH (July 1997). "Juvenile myelomonocytic leukemia". Blood. 90 (2): 479–88. PMID 9226148.
- ↑ Hasle H (March 1994). "Myelodysplastic syndromes in childhood--classification, epidemiology, and treatment". Leuk. Lymphoma. 13 (1–2): 11–26. doi:10.3109/10428199409051647. PMID 8025513.
- ↑ Patnaik MM, Tefferi A (March 2017). "Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis (RARS-T): 2017 update on diagnosis, risk-stratification, and management". Am. J. Hematol. 92 (3): 297–310. doi:10.1002/ajh.24637. PMID 28188970.
- ↑ Alshaban A, Padilla O, Philipovskiy A, Corral J, McAlice M, Gaur S (2018). "Lenalidomide induced durable remission in a patient with MDS/MPN-with ring sideroblasts and thrombocytosis with associated 5q- syndrome". Leuk Res Rep. 10: 37–40. doi:10.1016/j.lrr.2018.08.001. PMID 30186759.
- ↑ Bouchla A, Papageorgiou SG, Tsakiraki Z, Glezou E, Pavlidis G, Stavroulaki G, Bazani E, Foukas P, Pappa V (2018). "Plasmablastic Lymphoma in an Immunocompetent Patient with MDS/MPN with Ring Sideroblasts and Thrombocytosis-A Case Report". Case Rep Hematol. 2018: 2525070. doi:10.1155/2018/2525070. PMC 6247723. PMID 30524760.
- ↑ You MJ, Medeiros LJ, Hsi ED (September 2015). "T-lymphoblastic leukemia/lymphoma". Am. J. Clin. Pathol. 144 (3): 411–22. doi:10.1309/AJCPMF03LVSBLHPJ. PMID 26276771.
- ↑ Patel KJ, Latif SU, de Calaca WM (March 2009). "An unusual presentation of precursor T cell lymphoblastic leukemia/lymphoma with cholestatic jaundice: case report". J Hematol Oncol. 2: 12. doi:10.1186/1756-8722-2-12. PMC 2663564. PMID 19284608.
- ↑ Elreda L, Sandhu M, Sun X, Bekele W, Cohen AJ, Shah M (2014). "T-cell lymphoblastic leukemia/lymphoma: relapse 16 years after first remission". Case Rep Hematol. 2014: 359158. doi:10.1155/2014/359158. PMC 4005062. PMID 24822133.
- ↑ Sedick Q, Alotaibi S, Alshieban S, Naheet KB, Elyamany G (2017). "Natural Killer Cell Lymphoblastic Leukaemia/Lymphoma: Case Report and Review of the Recent Literature". Case Rep Oncol. 10 (2): 588–595. doi:10.1159/000477843. PMID 28868017.
- ↑ Jain N, Lamb AV, O'Brien S, Ravandi F, Konopleva M, Jabbour E, Zuo Z, Jorgensen J, Lin P, Pierce S, Thomas D, Rytting M, Borthakur G, Kadia T, Cortes J, Kantarjian HM, Khoury JD (April 2016). "Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype". Blood. 127 (15): 1863–9. doi:10.1182/blood-2015-08-661702. PMC 4915808. PMID 26747249.
- ↑ Haydu JE, Ferrando AA (July 2013). "Early T-cell precursor acute lymphoblastic leukaemia". Curr. Opin. Hematol. 20 (4): 369–73. doi:10.1097/MOH.0b013e3283623c61. PMC 3886681. PMID 23695450.