|
|
| (37 intermediate revisions by 14 users not shown) |
| Line 1: |
Line 1: |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]'''
| | __NOTOC__ |
| | | {| class="infobox" style="float:right;" |
| | |- |
| | | [[File:Siren.gif|30px|link=Wolff-Parkinson-White syndrome resident survival guide]]|| <br> || <br> |
| | | [[Wolff-Parkinson-White syndrome resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = Wolff-Parkinson-White syndrome | | | Name = Wolff-Parkinson-White syndrome | |
| Image = Wpw full ecg.jpg | | | Image = WPW_syndrome_2.jpg | |
| Caption = | | | Caption = | |
| DiseasesDB = 14186 |
| |
| ICD10 = {{ICD10|I|45|6|i|30}} |
| |
| ICD9 = {{ICD9|426.7}} |
| |
| ICDO = |
| |
| OMIM = 194200 |
| |
| MeshName = Wolff-Parkinson-White+Syndrome |
| |
| MeshNumber = C14.280.067.780.977 |
| |
| }} | | }} |
| {{Wolff-Parkinson-White syndrome}} | | {{Wolff-Parkinson-White syndrome}} |
| {{SI}} | | {{Patient}} |
| {{WikiDoc Cardiology Network Infobox}} | | |
| {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | | {{CMG}}; {{AE}} {{Sara.Zand}} {{CZ}}; [[User:Alonso Alvarado|Alonso Alvarado, M.D.]] |
| | |
| | {{SK}} WPW syndrome, WPW pattern |
|
| |
|
| ==[[Wolff-Parkinson-White syndrome overview|Overview]]== | | ==[[Wolff-Parkinson-White syndrome overview|Overview]]== |
| Line 22: |
Line 21: |
| ==[[Wolff-Parkinson-White syndrome historical perspective|Historical Perspective]]== | | ==[[Wolff-Parkinson-White syndrome historical perspective|Historical Perspective]]== |
|
| |
|
| ==[[Wolff-Parkinson-White syndrome classification scheme|Classification Scheme]]== | | ==[[Wolff-Parkinson-White syndrome classification scheme|Classification]]== |
| [[Wolff-Parkinson-White syndrome classification scheme#EKG Classification|EKG Classification]] | [[Wolff-Parkinson-White syndrome classification scheme#Variants of WPW|WPW Variants]] | | [[Wolff-Parkinson-White syndrome classification scheme#EKG Classification|EKG Classification]] | [[Wolff-Parkinson-White syndrome classification scheme#Variants of WPW|WPW Variants]] |
|
| |
|
| ==[[Wolff-Parkinson-White syndrome pathophysiology|Pathophysiology]]== | | ==[[Wolff-Parkinson-White syndrome pathophysiology|Pathophysiology]]== |
| | |
| | ==[[Wolff-Parkinson-White syndrome differential diagnosis|Differentiating Wolff-Parkinson-White syndrome from other Diseases]]== |
|
| |
|
| ==[[Wolff-Parkinson-White syndrome epidemiology and demographics|Epidemiology and Demographics]]== | | ==[[Wolff-Parkinson-White syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| ==[[Wolff-Parkinson-White syndrome differential diagnosis|Differential Diagnosis]]== | | ==[[Wolff-Parkinson-White syndrome risk factors|Risk Factors]]== |
| | |
| | ==[[Wolff-Parkinson-White syndrome natural history|Natural History, Complications and Prognosis]]== |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| [[Wolff-Parkinson-White syndrome diagnosis overview|Approach]] | [[Wolff-Parkinson-White syndrome EKG|EKG]] | [[Wolff-Parkinson-White syndrome EP studies|Electrophysiology studies]] | | [[Wolff-Parkinson-White syndrome diagnosis overview|Approach]] | [[Wolff-Parkinson-White syndrome history and symptoms|History and Symptoms]] | [[Wolff-Parkinson-White syndrome EKG|Electrocardiogram]] | [[Wolff-Parkinson-White syndrome EKG examples|EKG Examples]] | [[Wolff-Parkinson-White syndrome other diagnostic studies|Other Diagnostic Studies]] |
| | |
| ==Risk stratification==
| |
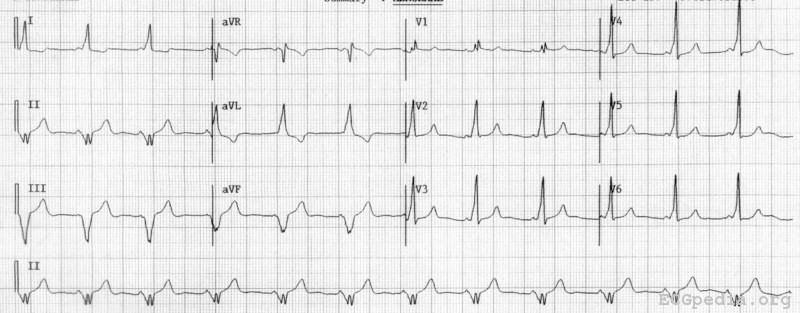
| [[Image:Wolff-Parkinson-White_syndrome_12_lead_EKG.png|thumb|right|200px|12 lead [[electrocardiogram|EKG]] of an individual with WPW syndrome. The accessory pathway is located in the left posteroseptal region.]] | |
| | |
| Treatment is based on risk stratification of the individual. Risk stratification is performed to determine which individuals with WPW syndrome are at risk for sudden cardiac death (SCD). Sudden cardiac death in these individuals is due to the propagation of an atrial arrhythmia to the ventricles at a very high rate.
| |
| | |
| A good history should be taken to determine whether an individual has factors suggestive of a previous episode of unexplained [[syncope]] (fainting) or [[palpitations]] (sudden awareness of one's own, usually irregular, heartbeat). These may be due to earlier episodes of a tachycardia associated with the accessory pathway.
| |
| | |
| Individuals with WPW syndrome in whom the delta waves disappear with increases in the heart rate are considered at lower risk of SCD. This is because the loss of the delta wave shows that the accessory pathway cannot conduct electrical impulses at a high rate (in the anterograde direction). These individuals will typically not have fast conduction down the accessory pathway during episodes of atrial fibrillation.
| |
| | |
| Risk stratification is best performed via [[programmed electrical stimulation]] (PES) in the [[cardiac electrophysiology]] lab. This is an invasive procedure, in which the rate of impulse propagation via the accessory pathway is determined by stimulating the atria and by inducing transient [[atrial fibrillation]].
| |
| | |
| High risk features that may be present during PES include an effective refractory period of the accessory pathway less than 270 ms, multiple pathways, septal location of pathway, and inducibility of supraventricular tachycardia. Individuals with any of these high risk features are generally considered at increased risk for SCD and should be treated accordingly.<ref name = Pappone_et_al_2003>{{cite journal
| |
| | author=Pappone C, Santinelli V, Manguso F, Augello G, Santinelli O, Vicedomini G, Gulletta S, Mazzone P, Tortoriello V, Pappone A, Dicandia C, Rosanio S.
| |
| | title=A randomized study of prophylactic catheter ablation in asymptomatic patients with the Wolff-Parkinson-White syndrome
| |
| | journal=New England Journal of Medicine
| |
| | volume=349
| |
| | issue=19
| |
| | year=2003
| |
| | pages=1803-11
| |
| | id=PMID 14602878
| |
| | url = http://content.nejm.org/cgi/content/full/349/19/1803
| |
| | format = free registration required }}</ref>
| |
| | |
| It is unclear whether invasive risk stratification (with programmed electrical stimulation) is necessary in the asymptomatic individual.<ref name = Cambell_et_al_2003>{{cite journal
| |
| | author=Campbell RM, Strieper MJ, Frias PA, Collins KK, Van Hare GF, Dubin AM
| |
| | title=Survey of current practice of pediatric electrophysiologists for asymptomatic Wolff-Parkinson-White syndrome
| |
| | journal=Pediatrics
| |
| | volume=111| issue=3| year=2003| pages=e245-7
| |
| | id=PMID 12612279
| |
| | url = http://pediatrics.aappublications.org/cgi/content/full/111/3/e245
| |
| }}</ref> While some groups advocate PES for risk stratification in all individuals under 35 years old, others only offer it to individuals who have history suggestive of a [[tachycardia|tachyarrhythmia]], since the incidence of sudden death is so low.<ref name = Munger_et_al_1993 /><ref name = Fitzsimmons_et_al_2001 />
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Acutely, people with WPW who are experiencing a tachydysrhythmia may require electrical [[cardioversion]] if their condition is critical, or, if more stable, medical treatment may be used. Patients with atrial fibrillation and rapid ventricular response are often treated with [[amiodarone]] or [[procainamide]] to stabilize their heart rate. Adenosine and other AV node blockers should be avoided in Atrial fibriliiatin with WPW; this inlcudes adenosine, diltiazem, verapamil,other calcium channel blockers and Beta-blockers. Patients with a rapid heart beat with narrow [[QRS complex]]es (circus movement tachycardias) may also be cardioverted, alternatively, [[adenosine]] may be administered if equipment for cardioversion is immediately available as a backup.
| | [[Wolff-Parkinson-White syndrome risk stratification|Risk Stratification]] | [[Wolff-Parkinson-White syndrome medical therapy|Medical Therapy]] | [[Wolff-Parkinson-White syndrome drug prophylaxis|Drug Prophylaxis]] | [[Wolff-Parkinson-White syndrome treatment algorithm|Management Algorithm]] |
| | |
| The definitive treatment of WPW syndrome is a destruction of the abnormal electrical pathway by radiofrequency [[catheter ablation]]. This procedure is performed almost exclusively by [[cardiac electrophysiology|cardiac electrophysiologists]]. Radiofrequency catheter ablation is not performed in all individuals with WPW syndrome because there are inherent risks involved in the procedure.
| |
| Adeosine is contraindicated for patients in atrial fibrillation or atrial flutter with a history of WPW
| |
| | |
| When performed by an experienced electrophysiologist, radiofrequency ablation has a high success rate.<ref name = Pappone_et_al_1993>{{cite journal
| |
| | author=Pappone C, Lamberti F, Santomauro M, Stabile G, De Simone A, Turco P, Pannain S, Loricchio ML, Rotunno R, Chiariello M
| |
| | title = Ablation of paroxysmal tachycardia in Wolff-Parkinson-White syndrome
| |
| | journal=Cardiologia
| |
| | volume=38| issue=12 Suppl 1| year=1993| pages=189-97
| |
| | id=PMID 8020017
| |
| | language = Italian }}</ref> If radiofrequency catheter ablation is successfully performed, the patient is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.<ref name = Pappone_et_al_1993 /> The one caveat is that individuals with underlying [[Ebstein's anomaly]] may develop additional accessory pathways during progression of their disease.
| |
| | |
| ===Circus Movement Tachycardias===
| |
| * Rapid heart rate is most likely due to CMT or atrial fibrillation.
| |
| * Palpitations are usually regular during a CMT, irregularly with atrial fib.
| |
| * Some patients report that their attacks of CMT may be broken by vagal maneuvers.
| |
| * A 24 hr holter should be done in those patients with a suspicion of WPW to assess the mode of initiation, and to determine the type (CMT vs afib).
| |
| * If the patients quality of life is affected and the holter is negative, then EP studies should be done.
| |
| * If there is an inability to induce CMT at EP then it is very unlikely that this is the arrhythmia that the patient is experiencing outside the hospital. Inability to induce CMT obviously does not exclude that the patient is experiencing afib.
| |
| * If the patient presents in a rapid rhythm, you should first try vagal maneuvers to terminate a CMT.
| |
| * The most likely arrhythmia on a statistical basis is a CMT with the AP conducting in a retrograde fashion. If the AP is incorporated in a retrograde fashion then there are often retrograde P waves apparent following the QRS, with a PR interval longer than the RP'interval.
| |
| * If the patient is known to have WPW and has a regular tachycardia thought to be a CMT, then verapamil should be the first drug used. If verapamil is not available, then use propranolol IV. Both terminate the CMT by prolonging the refractory period at the AV node.
| |
| * Digitalis has been used, however some patients may dev afib with this, and dig may abbreviate the refractory period of the AP resulting in higher ventricular rates during the afib. Therefore the use of dig is not recommended.
| |
| * If drugs affecting the AV node are not effective, then drugs that affect the accessory pathway are used such as procainamide or disopyramide.
| |
| * If the above fail to terminate the tachycardia or if the patient is tolerating the tachycardia poorly, then the patient should be paced out of it or cardioverted. Pacing is safer in patients on multiple drugs.
| |
| | |
| === Atrial Fibrillation ===
| |
| # Patients can experience high rates during afib because of conduction over the accessory pathway which can have a very short refractory period.
| |
| # Mean ventricular rates in these patients range from 160 to 300 BPM.
| |
| # During these attacks there is not only the risk of hemodynamic compromise but also a risk of degenerate into VF.
| |
| # As a rule dig should be avoided in these patients.
| |
| # Cardioversion is the tx of choice. If the patient is receiving drugs that promote asystole following electrical cardioversion (e.g. verapamil, beta-blockers, and probably amiodarone) then a temporary pacer should be positioned in the RV before the cardioversion.
| |
| # If the ventricular rate during the afib is not > 200, then you could try procainamide, disopyramide, or quinidine which may prolong the refractory period of the accessory pathway.
| |
| | |
| === Drug Prophylaxis In The Patient With Proven Tachyarrhythmias ===
| |
| # Should receive prophylactic treatment if the arrhythmia is poorly tolerated.
| |
| # In Wellen's experience amiodarone is the most effective in preventing attacks of paroxysmal tachycardia in patients with WPW. Otherwise he recommends quinidine, disopyramide, procainamide or propranolol alone or in combination.
| |
| # For those patients with life-threatening rates during afib, Wellen's recommends amiodarone as prophylaxis which prolongs the AP refractory period. Quinidine is an alternative, but is less effective.
| |
| # These patients should undergo EP studies to assess the adequacy of treatment.
| |
| # These authors state that the refractory period of the AP can shorten in the presence of sympathetic stimulation and advocate the addition of a beta blocker.
| |
| | |
| === Approach to the Patient with a Questionable EKG ===
| |
| # As mentioned previously, the diagnosis can be difficult in those patients c normal EKGs at rest.
| |
| # In some patients the diagnosis can be made with the following noninvasive procedures:
| |
| #* CSP to increase the AV nodal delay therefore enhancing conduction over the accessory pathway.
| |
| #* IV procainamide may cause QRS abnormality to disappear by prolonging conduction down the AP.
| |
| #* β-blockers, verapamil, digoxin may also facilitate the conduction down the accessory pathway
| |
| | |
| ==== Intractable Tachyarrhythmias in WPW ====
| |
| In patients with afib with rapid ventricular response then surgical interruption should be considered.
| |
| | |
| | |
| <div align="left">
| |
| <gallery heights="175" widths="175">
| |
| Image:Puzzle_2005_8_285_fig1.jpg|Figure 1: A 24 years old man with Mahaim type of preexcitation
| |
| Image:Puzzle_2005_8_285_fig2.jpg|Figure 2: The same patient after Mahaim bundle ablation
| |
| </gallery>
| |
| </div>
| |
| | |
| ==References==
| |
| {{reflist|2}}
| |
| | |
| ==Additional Resources==
| |
| * Adapted from The Wolff-Parkinson-White Syndrome, Wellens et al, Cardiac Arrhythmias, Mandel, Second Edition, Lippincott.
| |
|
| |
|
| ==Related Chapters== | | ==Related Chapters== |
| Line 139: |
Line 46: |
| * [[Electrocardiogram]] | | * [[Electrocardiogram]] |
| * [[Electrophysiologic study]] | | * [[Electrophysiologic study]] |
|
| |
| ==External links==
| |
| * [http://heartcenter.seattlechildrens.org/conditions_treated/wolff_parkinson_white_syndrome.asp Wolff-Parkinson-White syndrome information] from Seattle Children's Hospital Heart Center
| |
|
| |
|
| {{Electrocardiography}} | | {{Electrocardiography}} |
| {{SIB}}
| |
|
| |
|
| | [[Category:Best pages]] |
| | [[Category:Cardiology]] |
| | [[Category:Disease]] |
| [[Category:Genetic disorders]] | | [[Category:Genetic disorders]] |
| [[Category:Electrophysiology]] | | [[Category:Electrophysiology]] |
| [[Category:Cardiology]] | | [[Category:Arrhythmia]] |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |
| | | [[Category:Up-To-Date]] |
| [[de:Wolff-Parkinson-White-Syndrom]]
| | [[Category:Up-To-Date Cardiology]] |
| [[fr:Syndrome de Wolff-Parkinson-White]]
| |
| [[it:Sindrome di Wolff-Parkinson-White]]
| |
| [[ja:WPW症候群]]
| |
| [[pl:Zespół Wolffa-Parkinsona-White'a]]
| |
| [[pt:Wolff-Parkinson-White]] | |
| [[tr:Wolf-Parkinson-White Sendromu]] | |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |