Hernia: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (39 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{Hernia}} | {{Hernia}} | ||
{{CMG}}; {{AE}} {{EG}} | {{CMG}}; {{AE}} {{EG}}, {{Anmol}} | ||
' | ==Overview== | ||
A hernia is “the protrusion of an organ, organic part, or other bodily structure through the wall that usually contains it.<ref>{{cite book | title = Webster's new college dictionary | publisher = Houghton Mifflin Harcourt |page=531 | location = Boston | year = 2008 | isbn = 9780618396016 }}</ref> Hernias may be [[Congenital disorder|congenital]] or [[acquired]]. Based on the protruded body structure and the location of the protrusion, the hernia may be classified into [[Inguinal hernia|inguinal]], [[Femoral hernia|femoral]], [[Umbilical hernia|umbilical]], [[Diaphragmatic hernia|diaphragmatic]], [[Incisional hernia|incisional]], and other hernias. Different kinds of hernias, such as [[central nervous system|central nervous system (CNS)]], [[diaphragmatic hernia|diaphragmatic]], [[lumbar]], [[abdominal]], and [[pelvic]] hernias have to be differentiated on the basis of clinical manifestations. | |||
= | ==Classification== | ||
= | === Major classification of hernias in human body. === | ||
{{familytree/start | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | | | | |A01='''[[Hernia]]'''}} | {{familytree | | | | | | | | | | | | | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | | | | |A01='''[[Hernia]]'''}} | ||
{{familytree | | |,|-|-|-|-|-|v|-|-|-|-|-|-|-|+|-|-|-|v|-|-|-|-|-|-|-|-|-|.| | | | | | | | | | |}} | {{familytree | | | |,|-|-|-|v|-|-|-|v|-|-|-|-|-|-|-|+|-|-|-|v|-|-|-|-|-|-|-|-|-|.| | | | | | | | | | |}} | ||
{{familytree | | B01 | | | | B02 | | | | | | B03 | | B04 | | | | | | | | B05 | | | | | | | | | |B01='''''[[ | {{familytree | | | B01 | | B06 | | B02 | | | | | | B03 | | B04 | | | | | | | | B05 | | | | | | | | | |B01='''''[[CNS]]'''''|B02='''''[[diaphragmatic hernia|Diaphragmatic]]'''''|B03='''''[[Lumbar]]'''''|B04='''''[[Abdominal]]'''''|B05='''''[[Pelvic]]'''''|B06='''''[[Hiatal hernia|Hiatal]]'''''}} | ||
{{familytree | | |!| | | |,|-|^|-|.| | | |,|-|^|-|.| |!| |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | |}} | {{familytree | | | |!| | | |!| | | |!| | | | | | | |!| | | |!| | | | | | | | | |!| | | | | | | | | | |}} | ||
{{familytree | | | {{familytree | |,|-|^|-|.| |!| |,|-|^|-|.| | | |,|-|^|-|.| |!| |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | |}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | |}} | {{familytree | C01 | | C11 |!| C02 | | C03 | | C04 | | C05 |!| C06 | | C07 | | C08 | | C09 | | C10 | |C01=[[Brain hernia]]|C02=[[Morgagni hernia]]|C03=[[Bochdalek hernia]]|C04=[[Petit's hernia]]|C05=[[Grynfeltt's hernia]]|C06=[[Inguinal hernia]]|C07=[[Obturator hernia]]|C08=[[Perineal hernia]]|C09=[[Femoral hernia]]|C10=[[Sciatic hernia]]|C11=[[Lumbar disc herniation|Lumbar disc hernia]]}} | ||
{{familytree | {{familytree | | | | | | | |!| | | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | |}} | ||
{{familytree | | | | | | D01 | | D02 | | D03 | | D04 | | D05 | | D06 | | D07 | | D08 | {{familytree | | | | |,|-|-|^|-|.| | | |,|-|-|-|v|-|-|-|v|-|^|-|v|-|-|-|v|-|-|-|v|-|-|-|v|-|-|-|.| | |}} | ||
{{familytree | | | | D09 | | | D10 | | D01 | | D02 | | D03 | | D04 | | D05 | | D06 | | D07 | | D08 | |D01=[[Umbilical hernia]]|D02=[[Epigastric hernia]]|D03=[[Spigelian hernia]]|D04=[[Incisional hernia]]|D05=[[Amyand's hernia]]|D06=[[Alexis Littre|Littre's hernia]]|D07=[[August Gottlieb Richter|Richter's hernia]]|D08=[[Parastomal hernia]]|D09=[[Sliding hernias of the stomach|Sliding hernia]]|D10=Paraesophageal hernia}} | |||
{{familytree/end}} | {{familytree/end}} | ||
==Differential Diagnosis== | |||
* Different kinds of hernias, such as [[central nervous system|central nervous system (CNS)]], [[diaphragmatic hernia|diaphragmatic]], [[lumbar]], [[abdominal]], and [[pelvic]] hernias have to be differentiated upon various history, symptoms, and physical examination findings. | |||
<small> | |||
{| | {| | ||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |- style="background: #4479BA; color: #FFFFFF; text-align: center;" | ||
| Line 51: | Line 54: | ||
!ESR | !ESR | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | rowspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[CNS]] | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Brain hernia | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain hernia]]<ref name="pmid7627921">{{cite journal |vauthors=Fisher CM |title=Brain herniation: a revision of classical concepts |journal=Can J Neurol Sci |volume=22 |issue=2 |pages=83–91 |year=1995 |pmid=7627921 |doi= |url=}}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | + | ||
| style="background: #F5F5F5; padding: 5px;" |<nowiki>+</nowiki> | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" |[[Brain tissue]] herniation through [[foramen magnum]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Spinal disc herniation|Lumbar disc hernia]]<ref name="pmid20689695">{{cite journal| author=Schoenfeld AJ, Weiner BK| title=Treatment of lumbar disc herniation: Evidence-based practice. | journal=Int J Gen Med | year= 2010 | volume= 3 | issue= | pages= 209-14 | pmid=20689695 | doi= | pmc=2915533 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20689695 }} </ref> | ||
| style="background: # | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px; | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" |[[Nucleus pulposus]] herniation through [[Annulus fibrosus disci intervertebralis|annulus fibrosus]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Sliding hernia | | rowspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hiatal hernia|Hiatal]]<ref name="pmid21927653">{{cite journal| author=Hyun JJ, Bak YT| title=Clinical significance of hiatal hernia. | journal=Gut Liver | year= 2011 | volume= 5 | issue= 3 | pages= 267-77 | pmid=21927653 | doi=10.5009/gnl.2011.5.3.267 | pmc=3166665 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21927653 }} </ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Sliding hernias of the stomach|Sliding hernia]] | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" |[[Stomach]] herniation through [[diaphragm]] | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Paraesophageal hernia | ||
| style="background: # | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px; | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" |[[Esophagus]] herniation through [[diaphragm]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |- | ||
| | | rowspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Diaphragmatic hernia|Diaphragmatic]]<ref name="urlCongenital Diaphragmatic Hernia Overview - GeneReviews® - NCBI Bookshelf">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK1359/ |title=Congenital Diaphragmatic Hernia Overview - GeneReviews® - NCBI Bookshelf |format= |work= |accessdate=}}</ref> | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Morgagni hernia]] | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" |[[Congenital]] herniation of [[stomach]] through left side of [[diaphragm]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Bochdalek hernia]] | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | - | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; " |[[Congenital]] herniation of [[stomach]] through right anterior side of [[diaphragm]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | rowspan="7" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Abdominal]] | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Umbilical hernia]]<ref name="pmid14626398">{{cite journal| author=Gonzalez R, Mason E, Duncan T, Wilson R, Ramshaw BJ| title=Laparoscopic versus open umbilical hernia repair. | journal=JSLS | year= 2003 | volume= 7 | issue= 4 | pages= 323-8 | pmid=14626398 | doi= | pmc=3021337 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14626398 }}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px; " |[[Bowels]] herniation through [[umbilicus]] | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Epigastric hernia]]<ref name="pmid14533911">{{cite journal |vauthors=Muschaweck U |title=Umbilical and epigastric hernia repair |journal=Surg. Clin. North Am. |volume=83 |issue=5 |pages=1207–21 |year=2003 |pmid=14533911 |doi=10.1016/S0039-6109(03)00119-1 |url=}}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; " |[[Bowels]] herniation through [[Epigastric region|epigastric abdominal wall]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Spigelian hernia]]<ref name="pmid19547696">{{cite journal| author=Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M et al.| title=[Not Available]. | journal=J Minim Access Surg | year= 2008 | volume= 4 | issue= 4 | pages= 95-8 | pmid=19547696 | doi= | pmc=2699222 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19547696 }}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; " |[[Bowels]] herniation through lateral [[abdominal wall]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Amyand's hernia]]<ref name="pmid22879848">{{cite journal| author=Singal R, Gupta S| title="Amyand's Hernia" - Pathophysiology, Role of Investigations and Treatment. | journal=Maedica (Buchar) | year= 2011 | volume= 6 | issue= 4 | pages= 321-7 | pmid=22879848 | doi= | pmc=3391951 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22879848 }}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; " |[[Vermiform appendix|Appendix vermiformis]] herniation through [[abdominal wall]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Alexis Littre|Littre's hernia]]<ref name="pmid16553126">{{cite journal |vauthors=Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P |title=Littre hernia: surgical anatomy, embryology, and technique of repair |journal=Am Surg |volume=72 |issue=3 |pages=238–43 |year=2006 |pmid=16553126 |doi= |url=}}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; " |[[Meckel's diverticulum]] herniation through [[abdominal wall]] | ||
|- | |- | ||
| | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[August Gottlieb Richter|Richter's hernia]]<ref name="pmid16536253">{{cite journal |vauthors=Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P |title=Richter hernia: surgical anatomy and technique of repair |journal=Am Surg |volume=72 |issue=2 |pages=180–4 |year=2006 |pmid=16536253 |doi= |url=}}</ref> | ||
| style="background: # | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px; | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" |[[Bowels]] herniation and [[strangulation]] through [[abdominal wall]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Parastomal hernia]]<ref name="pmid25435825">{{cite journal| author=Gillern S, Bleier JI| title=Parastomal hernia repair and reinforcement: the role of biologic and synthetic materials. | journal=Clin Colon Rectal Surg | year= 2014 | volume= 27 | issue= 4 | pages= 162-71 | pmid=25435825 | doi=10.1055/s-0034-1394090 | pmc=4226750 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25435825 }}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" |[[Bowels]] herniation through [[stoma]] in the [[abdominal wall]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | rowspan="5" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pelvic]] | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Inguinal hernia]]<ref name="pmid18244999">{{cite journal| author=Jenkins JT, O'Dwyer PJ| title=Inguinal hernias. | journal=BMJ | year= 2008 | volume= 336 | issue= 7638 | pages= 269-72 | pmid=18244999 | doi=10.1136/bmj.39450.428275.AD | pmc=2223000 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18244999 }}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" |[[Bowels]] herniation through [[inguinal ring]] | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Obturator hernia]]<ref name="pmid12371643">{{cite journal |vauthors=Nakayama T, Kobayashi S, Shiraishi K, Nishiumi T, Mori S, Isobe K, Furuta Y |title=Diagnosis and treatment of obturator hernia |journal=Keio J Med |volume=51 |issue=3 |pages=129–32 |year=2002 |pmid=12371643 |doi= |url=}}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" |[[Viscera]] herniation through [[obturator canal]] | ||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Sciatic hernia | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Perineal hernia]]<ref name="pmid28673377">{{cite journal |vauthors=Levic K, Rosen KV, Bulut O, Bisgaard T |title=Low incidence of perineal hernia repair after abdominoperineal resection for rectal cancer |journal=Dan Med J |volume=64 |issue=7 |pages= |year=2017 |pmid=28673377 |doi= |url=}}</ref> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px; text-align: center;" | - | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" |[[Viscera]] herniation through [[pelvic floor]] | ||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Femoral hernia]]<ref name="pmid13595543">{{cite journal| author=LUDINGTON LG| title=Femoral hernia and its management, with particular reference to its occurrence following inguinal herniorrhaphy. | journal=Ann Surg | year= 1958 | volume= 148 | issue= 5 | pages= 823-6 | pmid=13595543 | doi= | pmc=1450902 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13595543 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px;" |[[Bowels]] herniation through [[femoral ring]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Sciatic hernia]]<ref name="pmid20197431">{{cite journal| author=Kandpal H, Madhusudhan KS| title=Sciatic hernia causing sciatica: MRI and MR neurography showing entrapment of sciatic nerve. | journal=Br J Radiol | year= 2010 | volume= 83 | issue= 987 | pages= e65-6 | pmid=20197431 | doi=10.1259/bjr/47866965 | pmc=3473559 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20197431 }}</ref> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; " |[[Viscera]] herniation through [[Sciatic notch|sciatic canal]] | |||
|} | |||
</small> | |||
==CNS Hernia== | |||
{| align="right" | |||
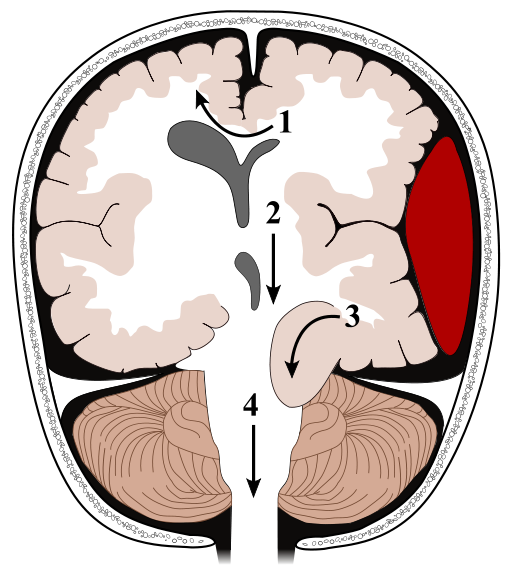
|[[image:512px-Brain herniation types.svg.png|thumb|260px|Different types of brain herniation - By User:Delldot, via Wikimedia Commons<ref>[<"http://www.gnu.org/copyleft/fdl.html">GFDL, <"http://creativecommons.org/licenses/by-sa/3.0/">CC-BY-SA-3.0 or <"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3ABrain_herniation_types.svg"></ref>]] | |||
[[image:Blausen 0484 HerniatedLumbarDisc.png|thumb|260px|Lumbar disc herniation - By BruceBlaus, via Wikimedia Commons<ref>Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. (Own work) [<"http://creativecommons.org/licenses/by/3.0">CC BY 3.0], <"https://commons.wikimedia.org/wiki/File%3ABlausen_0484_HerniatedLumbarDisc.png"></ref>]] | |||
|} | |} | ||
{| | ===Brain hernia=== | ||
*[[Brain hernia]] is most commonly due to increase in [[Intracranial pressure|intracranial pressure (ICP)]]. | |||
*The cardinal features of [[brain herniation]] is acute [[loss of consciousness]], ipsilateral [[pupillary dilation]], and contralateral [[hemiparesis]].<ref name="pmid26438459">{{cite journal| author=Stevens RD, Shoykhet M, Cadena R| title=Emergency Neurological Life Support: Intracranial Hypertension and Herniation. | journal=Neurocrit Care | year= 2015 | volume= 23 Suppl 2 | issue= | pages= S76-82 | pmid=26438459 | doi=10.1007/s12028-015-0168-z | pmc=4791176 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26438459 }}</ref> | |||
* There are 4 types of brain hernation: | |||
**'''Type 1:''' Subfalcine herniation | |||
**'''Type 2:''' Transalar herniation (ascending and descending) | |||
**'''Type 3:''' Transtentorial herniation (uncal herniation) | |||
**'''Type 4:''' Extracranial herniation | |||
''' | For more information about brain hernia '''[[Brain hernia|click here]]''' | ||
<br> | |||
<br> | |||
<br> | |||
| | <br> | ||
| | <br> | ||
<br> | |||
* | <br> | ||
| | |||
* [[ | |||
* | === Lumbar disc hernia === | ||
* [[Lumbar disc herniation|Lumbar disc hernia]] is related to old age, lack of [[physical activity]], and all the factors that may result in [[dehydration]] of [[intervertebral discs]]. | |||
* The cardinal features of [[lumbar disc herniation]] is [[radiculopathy]], decreased [[Deep tendon reflex|deep tendon reflexes]], and [[Atrophy|muscular atrophy]]. | |||
* The mainstay of treatment in [[Lumbar disc herniation|lumbar disc hernia]] is complete bed rest. | |||
* | * [[Neurosurgical]] interventions may be indicated in patients with refractory symptoms unresponsive to medical therapy.<ref name="urlHerniated Disc - National Library of Medicine - PubMed Health">{{cite web |url=https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024495/ |title=Herniated Disc - National Library of Medicine - PubMed Health |format= |work= |accessdate=}}</ref> | ||
For more information about lumbar disc hernia '''[[Spinal disc herniation|click here]]''' | |||
* [[ | <br> | ||
|- | <br> | ||
| | <br> | ||
| | <br> | ||
* | <br> | ||
<br> | |||
* [[ | <br> | ||
* [[ | |||
|- | == Diaphragmatic Hernia == | ||
| | |||
| | === Bochdalek hernia === | ||
* [[Bochdalek|Bochdalek hernia]] is the most common type (80-90%) of [[congenital diaphragmatic hernia]]. | |||
* [[Bochdalek hernia]] is herniation of [[stomach]] through posterior left side of the [[diaphragm]]. | |||
* If the [[Bochdalek hernia]] occurs [[in utero]], the [[neonate]] present with complications including [[pulmonary]] [[hypoplasia]] and even death.<ref name="pmid3718216">{{cite journal |vauthors=Newman BM, Afshani E, Karp MP, Jewett TC, Cooney DR |title=Presentation of congenital diaphragmatic hernia past the neonatal period |journal=Arch Surg |volume=121 |issue=7 |pages=813–6 |year=1986 |pmid=3718216 |doi= |url=}}</ref> | |||
For more information about Bochdalek hernia '''[[Bochdalek hernia|click here]]''' | |||
=== Morgagni hernia === | |||
* [[Morgagni hernia]] is less common (10-20%) than [[Congenital diaphragmatic hernia|Bochdalek congenital diaphragmatic hernia]]. | |||
* [[Morgagni hernia]] is most commonly retrosternal and on the right side of the [[diaphragm]]. | |||
* [[Morgagni hernia]] occurs in approximately 50 per 100,000 [[pregnancies]].<ref name="pmid12751867">{{cite journal |vauthors=Robnett-Filly B, Goldstein RB, Sampior D, Hom M |title=Morgagni hernia: a rare form of congenital diaphragmatic hernia |journal=J Ultrasound Med |volume=22 |issue=5 |pages=537–9 |year=2003 |pmid=12751867 |doi= |url=}}</ref> | |||
For more information about Morgagni hernia '''[[Morgagni hernia|click here]]''' | |||
== Hiatal Hernia == | |||
=== Sliding hernia === | |||
{| align="right" | |||
|[[image:256px-Hiatus hernia.svg.png|thumb|400px|Different types of hiatal herniation - By Mysid, via Wikimedia Commons<ref>[<"http://creativecommons.org/publicdomain/zero/1.0/deed.en">CC0], <"https://commons.wikimedia.org/wiki/File%3AHiatus_hernia.svg"></ref>]] | |||
|} | |||
==== Type I ==== | |||
* [[Hiatus hernia|Sliding hernia]] accounts for more than 95% of all cases of [[hiatal hernia]]. | |||
* [[Sliding hernias of the stomach|Sliding hernia]] is herniation of distal [[esophagus]] and also [[Cardia|gastric cardia]] into the [[Thoracic cavity|thoracic space]]. | |||
* Displacement of less than 2 cm is considered as [[Physiological|physiologic]] displacement, mostly occurred during [[swallow]] process. | |||
=== Paraesophageal hernias === | |||
==== Type II ==== | |||
* Type II of paraesophageal hernias is the classic herniation of a part of [[Fundus (stomach)|gastric fundus]], but not [[gastroesophageal junction]], into the [[thoracic cavity]]. | |||
* Without [[surgical]] repair and fixation of the herniated portion, it leads to incarceration and may lead to complications. | |||
==== Type III ==== | |||
* Type III of paraesophageal hernias is the combination of both type I and type II. | |||
* In type III, [[Fundus (stomach)|gastric fundus]] is herniated through the [[diaphragm]] along with [[gastroesophageal junction]]. | |||
==== Type IV ==== | |||
* The most severe form of the [[hiatal hernia]] is type IV, which consists of herniation of other [[abdominal]] organs along with [[stomach]] and distal [[esophagus]] into [[thoracic cavity]]. | |||
* Severe [[respiratory distress]] and [[dyspepsia]] may occur secondary to type IV paraesophageal hernia.<ref name="pmid21927653">{{cite journal| author=Hyun JJ, Bak YT| title=Clinical significance of hiatal hernia. | journal=Gut Liver | year= 2011 | volume= 5 | issue= 3 | pages= 267-77 | pmid=21927653 | doi=10.5009/gnl.2011.5.3.267 | pmc=3166665 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21927653 }}</ref> | |||
For more information about hiatal hernia '''[[Hiatal hernia|click here]]''' | |||
== Lumbar Hernia == | |||
{| align="right" | |||
|[[image:LumbarTriangle.jpg|thumb|600px|Lumbar triangles - Zyryab at English Wikipedia, via Wikimedia Commons<ref><"https://en.wikipedia.org/wiki/User:Zyryab" class="extiw" title="wikipedia:User:Zyryab">Zyryab at <"https://en.wikipedia.org/wiki/" class="extiw" title="wikipedia:">English Wikipedia [<"http://www.gnu.org/copyleft/fdl.html">GFDL, <"http://creativecommons.org/licenses/by-sa/3.0/">CC-BY-SA-3.0 or <"http://creativecommons.org/licenses/by/2.5">CC BY 2.5], <"https://commons.wikimedia.org/wiki/File%3ALumbarTriangle.jpg">via Wikimedia Commons</ref>]] | |||
|} | |||
=== Petit's hernia === | |||
* Inferior [[lumbar]] region has a triangle formed by the [[iliac crest]], the margins of the [[latissimus dorsi muscle]], and [[Abdominal external oblique muscle|external abdominal oblique muscles]]. | |||
* [[Petit's hernia]] is defined as herniation of [[retroperitoneal]] fat through [[internal oblique muscle]] [[aponeurosis]] within the inferior lumbar triangle. | |||
* [[Petit's hernia]] commonly occurs on the left side and in males. | |||
* [[Strangulation]] rarely occurs in [[Petit's hernia]], because of wide herniation neck. | |||
=== Grynfeltt's hernia === | |||
* Superior [[lumbar]] region has a triangle formed formed medially by the [[quadratus lumborum muscle]], laterally by the internal abdominal oblique muscle, and superiorly by the 12th rib. | |||
* [[Grynfeltt's hernia]] is defined as herniation of retroperitoneal fat through transversalis muscle [[aponeurosis]] within the superior lumbar triangle. | |||
* The mainstay of treatment for lumbar hernias is surgery fixation.<ref name="pmid28944339">{{cite journal| author=Başak F, Hasbahçeci M, Canbak T, Acar A, Şişik A, Baş G et al.| title=Lumbar (Petit's) hernia: A rare entity. | journal=Turk J Surg | year= 2017 | volume= 33 | issue= 3 | pages= 220-221 | pmid=28944339 | doi=10.5152/UCD.2015.2986 | pmc=5602318 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28944339 }}</ref> | |||
<br> | |||
== Abdominal Hernia == | |||
{| align="right" | |||
|[[image:Ernia Ombelicale.jpg|thumb|300px|Umbilical hernia - By Rocco_Cusari, via Wikimedia Commons<ref>[<"https://creativecommons.org/licenses/by-sa/2.5">CC BY-SA 2.5], <"https://commons.wikimedia.org/wiki/File%3AErnia_Ombelicale.jpg"></ref>]] | |||
[[image:Hernia epigástrica.png|thumb|300px|Epigastric hernia - By PacoPeramo (Own work), via Wikimedia Commons<ref>[<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3AHernia_epig%C3%A1strica.png"></ref>]] | |||
[[image:Hernia spiegheli 01.JPG|thumb|300px|Spigelian hernia - By AfroBrazilian (Own work), via Wikimedia Commons<ref>[<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0 or <"http://www.gnu.org/copyleft/fdl.html">GFDL], <"https://commons.wikimedia.org/wiki/File%3AHernia_spiegheli_01.JPG"></ref>]] | |||
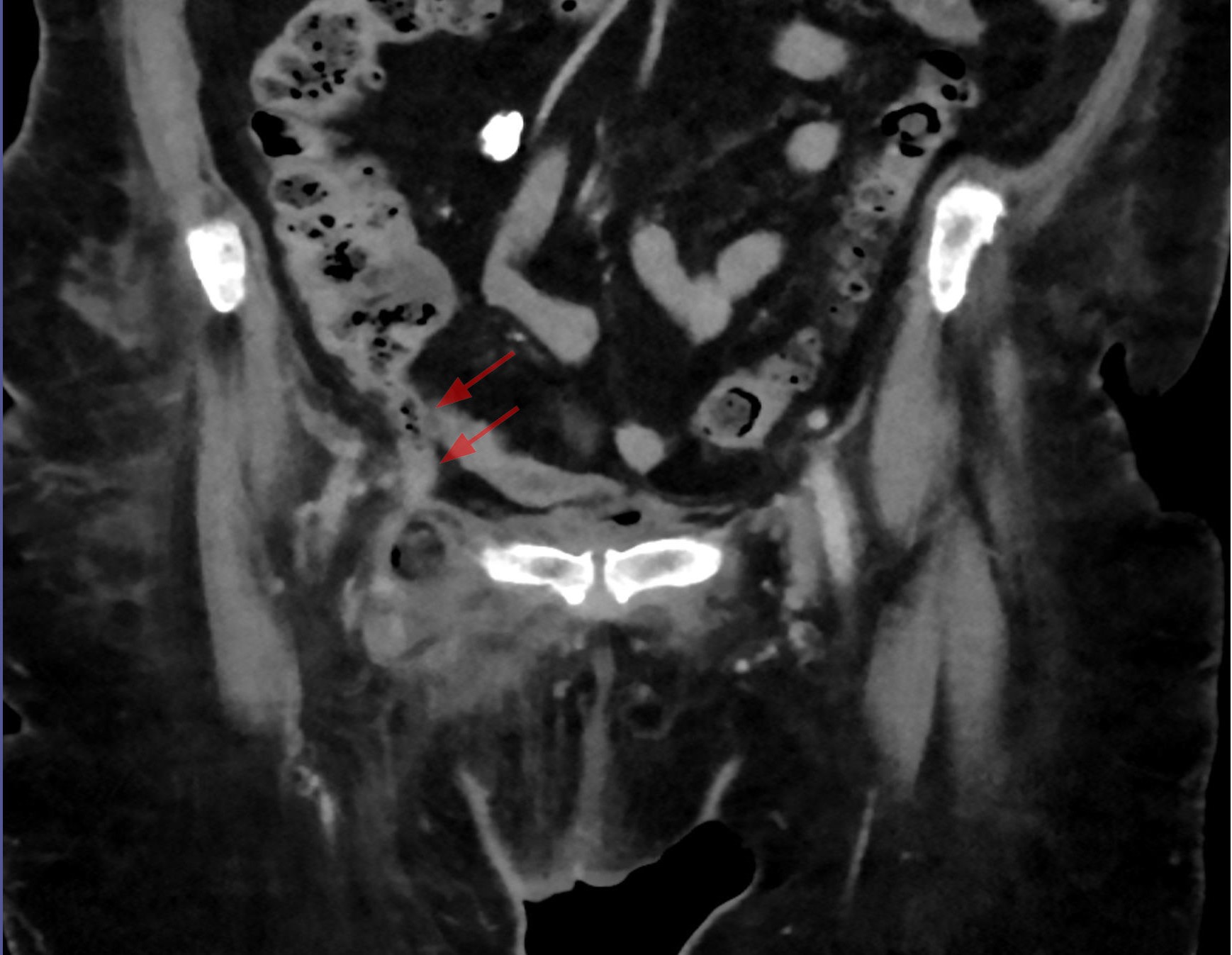
[[image:De Garengeot-Hernie mit Appendizitis - CT axial und coronar - 001.jpg|thumb|300px|Amyand's hernia: presence of appendix vermiformis (red arrows) in inguinal hernia - By Hellerhoff (Own work), via Wikimedia Commons<ref>[<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3ADe_Garengeot-Hernie_mit_Appendizitis_-_CT_axial_und_coronar_-_001.jpg"></ref>]] | |||
|} | |} | ||
=== Umbilical hernia === | |||
* [[Umbilical hernia]] consists of 6% of all [[abdominal]] hernias in adults. | |||
* The mainstay of treatment for [[umbilical hernia]] is surgery, including [[Mesh|Mesh repair]], Mayo repair, and [[Laparoscopic surgery|laparoscopic repair]]. | |||
* [[Strangulation]] and incarceration are very rare in [[umbilical hernia]].<ref name="pmid15972174">{{cite journal |vauthors=Polat C, Dervisoglu A, Senyurek G, Bilgin M, Erzurumlu K, Ozkan K |title=Umbilical hernia repair with the prolene hernia system |journal=Am. J. Surg. |volume=190 |issue=1 |pages=61–4 |year=2005 |pmid=15972174 |doi=10.1016/j.amjsurg.2004.09.021 |url=}}</ref> | |||
For more information about umbilical hernia '''[[Umbilical hernia|click here]]''' | |||
<br> | |||
<br> | |||
=== Epigastric hernia === | |||
* [[Epigastric hernia]] is accounted for 0.5-5% of hernias. | |||
* [[Epigastric hernia]] is a kind of [[abdominal wall]] herniation which is caused by weakness or defect in upper [[abdominal muscles]] or [[tendons]]. | |||
* The herniated contents are mostly [[vascular]] structures and properitoneal fat, rarely [[Abdominal|abdominal viscera]].<ref name="pmid25667986">{{cite journal| author=Grella R, Razzano S, Lamberti R, Trojaniello B, D'Andrea F, Nicoletti GF| title=Combined epigastric hernia repair and mini-abdominoplasty. Case report. | journal=Int J Surg Case Rep | year= 2015 | volume= 8C | issue= | pages= 111-3 | pmid=25667986 | doi=10.1016/j.ijscr.2014.10.033 | pmc=4353989 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25667986 }}</ref> | |||
<br> | |||
=== Spigelian hernia === | |||
* [[Spigelian hernia]] is caused by a defect in [[anterior abdominal wall]]. It is also named “[[spontaneous lateral ventral hernia]]” or “hernia of semilunar line”. | |||
* The mainstay of treatment for [[Spigelian hernia]] is surgery, can be done [[Laparoscopic surgery|laparoscopically]] or total exteraperitoneal repair method. | |||
* Incarceration and secondary [[bowel obstruction]] are the probable [[complications]] of [[Spigelian hernia]].<ref name="pmid19547696">{{cite journal| author=Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M et al.| title=[Not Available]. | journal=J Minim Access Surg | year= 2008 | volume= 4 | issue= 4 | pages= 95-8 | pmid=19547696 | doi= | pmc=2699222 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19547696 }}</ref> | |||
<br> | |||
=== Incisional hernia === | |||
* [[Incisional hernia]] occurs in 20% of patients [[Postoperative complication|postoperatively]]. | |||
* The common risk factors for patients with [[Post operative complications|postoperative]] [[incisional hernia]] include [[obesity]], [[diabetes]], emergency surgery, [[Wound dehiscence|postoperative wound dehiscence]], [[smoking]], and post-operative wound infection. | |||
* The mainstay of treatment for [[incisional hernia]] is open [[abdominal]] fixation [[surgery]].<ref name="pmid16719992">{{cite journal| author=Kingsnorth A| title=The management of incisional hernia. | journal=Ann R Coll Surg Engl | year= 2006 | volume= 88 | issue= 3 | pages= 252-60 | pmid=16719992 | doi=10.1308/003588406X106324 | pmc=1963672 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16719992 }}</ref> | |||
<br> | |||
=== Amyand's hernia === | |||
* [[Amyand's hernia]] is a kind of [[inguinal hernia]] which contains [[Vermiform appendix|appendix vermiformis]]. | |||
* The incidence of [[Amyand's hernia]] is approximately 0.19% to 1.7% of all reported hernias. | |||
* The [[strangulation]] and infarction are common complications of [[Amyand's hernia]].<ref name="pmid24473371">{{cite journal| author=Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR| title=Amyand's hernia: a review. | journal=Med Sci Monit | year= 2014 | volume= 20 | issue= | pages= 140-6 | pmid=24473371 | doi=10.12659/MSM.889873 | pmc=3915004 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24473371 }}</ref> | |||
<br> | |||
=== Littre's hernia === | |||
* Littre's hernia is incarcerated [[Meckel's diverticulum]] in [[Femoral hernia|femoral]], [[Inguinal hernia|inguinal]], or [[umbilical hernia]]. | |||
* Littre's hernia is a very rare condition, reported only in 50 cases till date. | |||
* [[Bowel obstruction]] and local inflammation are the possible [[complications]].<ref name="pmid28597002">{{cite journal| author=Malling B, Karlsen AA, Hern J| title=Littre Hernia: A Rare Case of an Incarcerated Meckel's Diverticulum. | journal=Ultrasound Int Open | year= 2017 | volume= 3 | issue= 2 | pages= E91-E92 | pmid=28597002 | doi=10.1055/s-0043-102179 | pmc=5462611 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28597002 }}</ref> | |||
<br> | |||
=== Richter's hernia === | |||
* Richter's hernia is first described in 1598. | |||
* Richter's hernia is the incarceration of a part of [[bowel]] in [[Femoral hernia|femoral]], [[Inguinal hernia|inguinal]], or [[umbilical hernia]]. | |||
* Since the high rates of [[Strangulation|strangulations]] and [[bowels]] infarctions, the [[mortality rate]] is very high and emergency surgical intervention is mandatory.<ref name="pmid8542091">{{cite journal |vauthors=Kadirov S, Sayfan J, Friedman S, Orda R |title=Richter's hernia--a surgical pitfall |journal=J. Am. Coll. Surg. |volume=182 |issue=1 |pages=60–2 |year=1996 |pmid=8542091 |doi= |url=}}</ref> | |||
<br> | |||
=== Parastomal hernia === | |||
* [[Parastomal hernia]] is a common complication of [[colostomy]] or [[ileostomy]], actually a type of [[incisional hernia]] related to them. | |||
* [[Parastomal hernia]] is classified into 4 subtpes: | |||
** '''[[Interstitial]]:''' The hernial sac lies within the layers of the [[abdominal wall]]. | |||
** '''[[Subcutaneous]]:''' The hernial sac lies in the [[subcutaneous]] plane. | |||
** '''Intrastomal:''' The hernial sac penetrates into a spout [[ileostomy]]. | |||
** '''Peristomal ([[prolapse]]):''' The hernial sac lies within a prolapsing stoma.<ref name="pmid12854101">{{cite journal |vauthors=Carne PW, Robertson GM, Frizelle FA |title=Parastomal hernia |journal=Br J Surg |volume=90 |issue=7 |pages=784–93 |year=2003 |pmid=12854101 |doi=10.1002/bjs.4220 |url=}}</ref> | |||
<br> | |||
== Pelvic Hernia == | |||
=== Inguinal hernia === | |||
* [[Inguinal hernia]] accounts for 75% of all hernias. [[Inguinal hernia]] repair is one of the most common [[surgeries]] in US (28 per 100,000 individuals). | |||
* [[Inguinal hernia]] is a bulging [[lump]] in [[Groin area|groin region]], presents commonly without [[pain]] or [[Inflammation|local inflammation]]. | |||
* [[Inguinal hernias]] classification is as follows: | |||
** '''[[Direct inguinal hernia|Direct hernia]]:''' The hernia sac herniates directly through the posterior wall of the [[inguinal canal]]. | |||
** '''[[Indirect inguinal hernia|Indirect hernia]]:''' The hernia sac herniates through the [[internal inguinal ring]] alongside the [[spermatic cord]].<ref name="pmid18244999">{{cite journal| author=Jenkins JT, O'Dwyer PJ| title=Inguinal hernias. | journal=BMJ | year= 2008 | volume= 336 | issue= 7638 | pages= 269-72 | pmid=18244999 | doi=10.1136/bmj.39450.428275.AD | pmc=2223000 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18244999 }}</ref> | |||
For more information about inguinal hernia '''[[Inguinal hernia|click here]]''' | |||
=== Obturator hernia === | |||
* Less than 1% of all hernias are [[obturator hernia]], and majority of times occurs in elderly women with [[chronic disease]]. | |||
* [[Obturator hernia]] is herniation of [[small intestine]] through [[obturator canal]], therefore mechanical [[small intestine]] obstruction is the most common complication. | |||
* The most common symptoms of [[obturator hernia]] are [[groin]] and proximal [[thigh]] pain.<ref name="pmid3413651">{{cite journal |vauthors=Bjork KJ, Mucha P, Cahill DR |title=Obturator hernia |journal=Surg Gynecol Obstet |volume=167 |issue=3 |pages=217–22 |year=1988 |pmid=3413651 |doi= |url=}}</ref> | |||
=== Perineal hernia === | |||
* [[Perineal hernia]] is herniation of [[intraperitoneal]] or [[Extraperitoneal fat|extraperitoneal]] contents through a [[congenital]] or acquired defect of the [[pelvic diaphragm]]. | |||
* [[Perineal hernia]] may be anterior or posterior to the [[Perineal membrane|superficial perineal muscles]]. | |||
* Majority of the times [[Perineal hernia|perineal hernias]] are [[congenital]] condition, while acquired [[Perineal hernia|perineal hernias]] are [[incisional hernia]] secondary to major [[pelvic]] surgeries (e.g., [[abdominoperineal resection]] of the anorectum and [[pelvic exenteration]]).<ref name="pmid20506875">{{cite journal |vauthors=Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P |title=Perineal hernia: surgical anatomy, embryology, and technique of repair |journal=Am Surg |volume=76 |issue=5 |pages=474–9 |year=2010 |pmid=20506875 |doi= |url=}}</ref> | |||
=== Femoral hernia === | |||
* [[Femoral hernia]] is the condition in which [[bowels]] herniate through [[femoral triangle]] medial to [[Femoral vein|femoral vessels]]. | |||
* The classification of [[Femoral hernia|femoral hernias]] into prevascular and retrovascular hernias is based on their position related to [[Femoral vein|femoral vessels]]. | |||
* [[Strangulation]] and incarceration of [[Femoral hernia|femoral hernias]] are common.<ref name="pmid18724783">{{cite journal| author=Paquet M, Penney J, Boerboom D| title=Lateral femoral hernias in a line of FVB/NHsd mice: a new confounding lesion linked to genetic background? | journal=Comp Med | year= 2008 | volume= 58 | issue= 4 | pages= 395-8 | pmid=18724783 | doi= | pmc=2706040 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18724783 }}</ref> | |||
For more information about femoral hernia '''[[Femoral hernia|click here]]''' | |||
=== Sciatic hernia === | |||
* [[Sciatic hernia]] is a rare herniation of [[bowels]] through the [[Greater sciatic foramen|greater]] or [[lesser sciatic foramen]]. | |||
* The [[symptoms]] and [[Physical examination|physical examinations]] are very similar to [[obturator hernia]]. | |||
* [[Swelling]] of [[gluteal region]], severe [[pelvic pain]] and local [[paresthesia]] are the common symptoms of [[sciatic hernia]]. | |||
* The mainstay of treatment is [[surgery]] and includes transabdominal and transgluteal approaches.<ref name="pmid21935810">{{cite journal |vauthors=Rather SA, Dar TI, Malik AA, Parray FQ, Ahmad M, Asrar S |title=Sciatic hernia clinically mimicking obturator hernia, missed by ultrasonography: case report |journal=Ulus Travma Acil Cerrahi Derg |volume=17 |issue=3 |pages=277–9 |year=2011 |pmid=21935810 |doi= |url=}}</ref> | |||
=References= | =References= | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
<references /> | |||
[[Category:Medicine]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Emergency medicine]] | |||
Latest revision as of 22:08, 29 July 2020
|
Hernia Landing page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2], Anmol Pitliya, M.B.B.S. M.D.[3]
Overview
A hernia is “the protrusion of an organ, organic part, or other bodily structure through the wall that usually contains it.[1] Hernias may be congenital or acquired. Based on the protruded body structure and the location of the protrusion, the hernia may be classified into inguinal, femoral, umbilical, diaphragmatic, incisional, and other hernias. Different kinds of hernias, such as central nervous system (CNS), diaphragmatic, lumbar, abdominal, and pelvic hernias have to be differentiated on the basis of clinical manifestations.
Classification
Major classification of hernias in human body.
Differential Diagnosis
- Different kinds of hernias, such as central nervous system (CNS), diaphragmatic, lumbar, abdominal, and pelvic hernias have to be differentiated upon various history, symptoms, and physical examination findings.
| Location | Diseases | History and Symptoms | Physical Examination | Laboratory Findings | Definition | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neurological | GI | Neurological | GI | ||||||||||||
| Confusion | Paresthesia | Dysphagia | Heartburn | Nausea | Bowel habits | Loss of Consciousness | Straight leg raise (SLR) | Mass protrusion | Tenderness/Rebound tenderness | Leukocytosis | CRP | ESR | |||
| CNS | Brain hernia[2] | + | + | + | - | + | - | + | - | - | - | - | - | - | Brain tissue herniation through foramen magnum |
| Lumbar disc hernia[3] | - | + | - | - | - | - | - | + | - | - | - | - | - | Nucleus pulposus herniation through annulus fibrosus | |
| Hiatal[4] | Sliding hernia | - | - | + | + | + | - | - | - | - | - | - | + | - | Stomach herniation through diaphragm |
| Paraesophageal hernia | - | - | + | + | + | - | - | - | - | - | - | - | - | Esophagus herniation through diaphragm | |
| Diaphragmatic[5] | Morgagni hernia | - | - | + | - | + | - | - | - | - | - | - | - | - | Congenital herniation of stomach through left side of diaphragm |
| Bochdalek hernia | - | - | + | - | + | - | - | - | - | - | - | - | - | Congenital herniation of stomach through right anterior side of diaphragm | |
| Abdominal | Umbilical hernia[6] | - | - | - | - | + | + | - | - | + | + | + | + | - | Bowels herniation through umbilicus |
| Epigastric hernia[7] | - | - | - | + | + | + | - | - | + | + | + | + | - | Bowels herniation through epigastric abdominal wall | |
| Spigelian hernia[8] | - | - | - | - | + | + | - | - | + | + | + | + | - | Bowels herniation through lateral abdominal wall | |
| Amyand's hernia[9] | - | - | - | - | + | + | - | - | + | + | + | + | - | Appendix vermiformis herniation through abdominal wall | |
| Littre's hernia[10] | - | - | - | - | + | + | - | - | + | + | + | + | - | Meckel's diverticulum herniation through abdominal wall | |
| Richter's hernia[11] | - | - | - | - | + | + | - | - | + | + | + | + | + | Bowels herniation and strangulation through abdominal wall | |
| Parastomal hernia[12] | - | - | - | - | + | + | - | - | + | + | + | + | + | Bowels herniation through stoma in the abdominal wall | |
| Pelvic | Inguinal hernia[13] | - | - | - | - | - | + | - | - | + | + | - | - | - | Bowels herniation through inguinal ring |
| Obturator hernia[14] | - | + | - | - | - | + | - | - | - | + | - | - | - | Viscera herniation through obturator canal | |
| Perineal hernia[15] | - | - | - | - | - | + | - | - | + | + | + | - | - | Viscera herniation through pelvic floor | |
| Femoral hernia[16] | - | + | - | - | - | + | - | - | + | + | - | - | - | Bowels herniation through femoral ring | |
| Sciatic hernia[17] | - | + | - | - | - | + | - | + | - | + | + | - | + | Viscera herniation through sciatic canal | |
CNS Hernia
  |
Brain hernia
- Brain hernia is most commonly due to increase in intracranial pressure (ICP).
- The cardinal features of brain herniation is acute loss of consciousness, ipsilateral pupillary dilation, and contralateral hemiparesis.[20]
- There are 4 types of brain hernation:
- Type 1: Subfalcine herniation
- Type 2: Transalar herniation (ascending and descending)
- Type 3: Transtentorial herniation (uncal herniation)
- Type 4: Extracranial herniation
For more information about brain hernia click here
Lumbar disc hernia
- Lumbar disc hernia is related to old age, lack of physical activity, and all the factors that may result in dehydration of intervertebral discs.
- The cardinal features of lumbar disc herniation is radiculopathy, decreased deep tendon reflexes, and muscular atrophy.
- The mainstay of treatment in lumbar disc hernia is complete bed rest.
- Neurosurgical interventions may be indicated in patients with refractory symptoms unresponsive to medical therapy.[21]
For more information about lumbar disc hernia click here
Diaphragmatic Hernia
Bochdalek hernia
- Bochdalek hernia is the most common type (80-90%) of congenital diaphragmatic hernia.
- Bochdalek hernia is herniation of stomach through posterior left side of the diaphragm.
- If the Bochdalek hernia occurs in utero, the neonate present with complications including pulmonary hypoplasia and even death.[22]
For more information about Bochdalek hernia click here
Morgagni hernia
- Morgagni hernia is less common (10-20%) than Bochdalek congenital diaphragmatic hernia.
- Morgagni hernia is most commonly retrosternal and on the right side of the diaphragm.
- Morgagni hernia occurs in approximately 50 per 100,000 pregnancies.[23]
For more information about Morgagni hernia click here
Hiatal Hernia
Sliding hernia
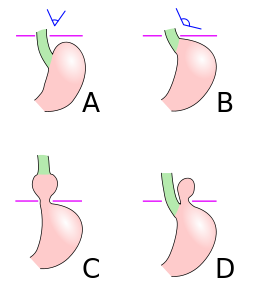 |
Type I
- Sliding hernia accounts for more than 95% of all cases of hiatal hernia.
- Sliding hernia is herniation of distal esophagus and also gastric cardia into the thoracic space.
- Displacement of less than 2 cm is considered as physiologic displacement, mostly occurred during swallow process.
Paraesophageal hernias
Type II
- Type II of paraesophageal hernias is the classic herniation of a part of gastric fundus, but not gastroesophageal junction, into the thoracic cavity.
- Without surgical repair and fixation of the herniated portion, it leads to incarceration and may lead to complications.
Type III
- Type III of paraesophageal hernias is the combination of both type I and type II.
- In type III, gastric fundus is herniated through the diaphragm along with gastroesophageal junction.
Type IV
- The most severe form of the hiatal hernia is type IV, which consists of herniation of other abdominal organs along with stomach and distal esophagus into thoracic cavity.
- Severe respiratory distress and dyspepsia may occur secondary to type IV paraesophageal hernia.[4]
For more information about hiatal hernia click here
Lumbar Hernia
 |
Petit's hernia
- Inferior lumbar region has a triangle formed by the iliac crest, the margins of the latissimus dorsi muscle, and external abdominal oblique muscles.
- Petit's hernia is defined as herniation of retroperitoneal fat through internal oblique muscle aponeurosis within the inferior lumbar triangle.
- Petit's hernia commonly occurs on the left side and in males.
- Strangulation rarely occurs in Petit's hernia, because of wide herniation neck.
Grynfeltt's hernia
- Superior lumbar region has a triangle formed formed medially by the quadratus lumborum muscle, laterally by the internal abdominal oblique muscle, and superiorly by the 12th rib.
- Grynfeltt's hernia is defined as herniation of retroperitoneal fat through transversalis muscle aponeurosis within the superior lumbar triangle.
- The mainstay of treatment for lumbar hernias is surgery fixation.[26]
Abdominal Hernia
    |
Umbilical hernia
- Umbilical hernia consists of 6% of all abdominal hernias in adults.
- The mainstay of treatment for umbilical hernia is surgery, including Mesh repair, Mayo repair, and laparoscopic repair.
- Strangulation and incarceration are very rare in umbilical hernia.[31]
For more information about umbilical hernia click here
Epigastric hernia
- Epigastric hernia is accounted for 0.5-5% of hernias.
- Epigastric hernia is a kind of abdominal wall herniation which is caused by weakness or defect in upper abdominal muscles or tendons.
- The herniated contents are mostly vascular structures and properitoneal fat, rarely abdominal viscera.[32]
Spigelian hernia
- Spigelian hernia is caused by a defect in anterior abdominal wall. It is also named “spontaneous lateral ventral hernia” or “hernia of semilunar line”.
- The mainstay of treatment for Spigelian hernia is surgery, can be done laparoscopically or total exteraperitoneal repair method.
- Incarceration and secondary bowel obstruction are the probable complications of Spigelian hernia.[8]
Incisional hernia
- Incisional hernia occurs in 20% of patients postoperatively.
- The common risk factors for patients with postoperative incisional hernia include obesity, diabetes, emergency surgery, postoperative wound dehiscence, smoking, and post-operative wound infection.
- The mainstay of treatment for incisional hernia is open abdominal fixation surgery.[33]
Amyand's hernia
- Amyand's hernia is a kind of inguinal hernia which contains appendix vermiformis.
- The incidence of Amyand's hernia is approximately 0.19% to 1.7% of all reported hernias.
- The strangulation and infarction are common complications of Amyand's hernia.[34]
Littre's hernia
- Littre's hernia is incarcerated Meckel's diverticulum in femoral, inguinal, or umbilical hernia.
- Littre's hernia is a very rare condition, reported only in 50 cases till date.
- Bowel obstruction and local inflammation are the possible complications.[35]
Richter's hernia
- Richter's hernia is first described in 1598.
- Richter's hernia is the incarceration of a part of bowel in femoral, inguinal, or umbilical hernia.
- Since the high rates of strangulations and bowels infarctions, the mortality rate is very high and emergency surgical intervention is mandatory.[36]
Parastomal hernia
- Parastomal hernia is a common complication of colostomy or ileostomy, actually a type of incisional hernia related to them.
- Parastomal hernia is classified into 4 subtpes:
- Interstitial: The hernial sac lies within the layers of the abdominal wall.
- Subcutaneous: The hernial sac lies in the subcutaneous plane.
- Intrastomal: The hernial sac penetrates into a spout ileostomy.
- Peristomal (prolapse): The hernial sac lies within a prolapsing stoma.[37]
Pelvic Hernia
Inguinal hernia
- Inguinal hernia accounts for 75% of all hernias. Inguinal hernia repair is one of the most common surgeries in US (28 per 100,000 individuals).
- Inguinal hernia is a bulging lump in groin region, presents commonly without pain or local inflammation.
- Inguinal hernias classification is as follows:
- Direct hernia: The hernia sac herniates directly through the posterior wall of the inguinal canal.
- Indirect hernia: The hernia sac herniates through the internal inguinal ring alongside the spermatic cord.[13]
For more information about inguinal hernia click here
Obturator hernia
- Less than 1% of all hernias are obturator hernia, and majority of times occurs in elderly women with chronic disease.
- Obturator hernia is herniation of small intestine through obturator canal, therefore mechanical small intestine obstruction is the most common complication.
- The most common symptoms of obturator hernia are groin and proximal thigh pain.[38]
Perineal hernia
- Perineal hernia is herniation of intraperitoneal or extraperitoneal contents through a congenital or acquired defect of the pelvic diaphragm.
- Perineal hernia may be anterior or posterior to the superficial perineal muscles.
- Majority of the times perineal hernias are congenital condition, while acquired perineal hernias are incisional hernia secondary to major pelvic surgeries (e.g., abdominoperineal resection of the anorectum and pelvic exenteration).[39]
Femoral hernia
- Femoral hernia is the condition in which bowels herniate through femoral triangle medial to femoral vessels.
- The classification of femoral hernias into prevascular and retrovascular hernias is based on their position related to femoral vessels.
- Strangulation and incarceration of femoral hernias are common.[40]
For more information about femoral hernia click here
Sciatic hernia
- Sciatic hernia is a rare herniation of bowels through the greater or lesser sciatic foramen.
- The symptoms and physical examinations are very similar to obturator hernia.
- Swelling of gluteal region, severe pelvic pain and local paresthesia are the common symptoms of sciatic hernia.
- The mainstay of treatment is surgery and includes transabdominal and transgluteal approaches.[41]
References
- ↑ Webster's new college dictionary. Boston: Houghton Mifflin Harcourt. 2008. p. 531. ISBN 9780618396016.
- ↑ Fisher CM (1995). "Brain herniation: a revision of classical concepts". Can J Neurol Sci. 22 (2): 83–91. PMID 7627921.
- ↑ Schoenfeld AJ, Weiner BK (2010). "Treatment of lumbar disc herniation: Evidence-based practice". Int J Gen Med. 3: 209–14. PMC 2915533. PMID 20689695.
- ↑ 4.0 4.1 Hyun JJ, Bak YT (2011). "Clinical significance of hiatal hernia". Gut Liver. 5 (3): 267–77. doi:10.5009/gnl.2011.5.3.267. PMC 3166665. PMID 21927653.
- ↑ "Congenital Diaphragmatic Hernia Overview - GeneReviews® - NCBI Bookshelf".
- ↑ Gonzalez R, Mason E, Duncan T, Wilson R, Ramshaw BJ (2003). "Laparoscopic versus open umbilical hernia repair". JSLS. 7 (4): 323–8. PMC 3021337. PMID 14626398.
- ↑ Muschaweck U (2003). "Umbilical and epigastric hernia repair". Surg. Clin. North Am. 83 (5): 1207–21. doi:10.1016/S0039-6109(03)00119-1. PMID 14533911.
- ↑ 8.0 8.1 Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M; et al. (2008). "[Not Available]". J Minim Access Surg. 4 (4): 95–8. PMC 2699222. PMID 19547696.
- ↑ Singal R, Gupta S (2011). ""Amyand's Hernia" - Pathophysiology, Role of Investigations and Treatment". Maedica (Buchar). 6 (4): 321–7. PMC 3391951. PMID 22879848.
- ↑ Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P (2006). "Littre hernia: surgical anatomy, embryology, and technique of repair". Am Surg. 72 (3): 238–43. PMID 16553126.
- ↑ Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P (2006). "Richter hernia: surgical anatomy and technique of repair". Am Surg. 72 (2): 180–4. PMID 16536253.
- ↑ Gillern S, Bleier JI (2014). "Parastomal hernia repair and reinforcement: the role of biologic and synthetic materials". Clin Colon Rectal Surg. 27 (4): 162–71. doi:10.1055/s-0034-1394090. PMC 4226750. PMID 25435825.
- ↑ 13.0 13.1 Jenkins JT, O'Dwyer PJ (2008). "Inguinal hernias". BMJ. 336 (7638): 269–72. doi:10.1136/bmj.39450.428275.AD. PMC 2223000. PMID 18244999.
- ↑ Nakayama T, Kobayashi S, Shiraishi K, Nishiumi T, Mori S, Isobe K, Furuta Y (2002). "Diagnosis and treatment of obturator hernia". Keio J Med. 51 (3): 129–32. PMID 12371643.
- ↑ Levic K, Rosen KV, Bulut O, Bisgaard T (2017). "Low incidence of perineal hernia repair after abdominoperineal resection for rectal cancer". Dan Med J. 64 (7). PMID 28673377.
- ↑ LUDINGTON LG (1958). "Femoral hernia and its management, with particular reference to its occurrence following inguinal herniorrhaphy". Ann Surg. 148 (5): 823–6. PMC 1450902. PMID 13595543.
- ↑ Kandpal H, Madhusudhan KS (2010). "Sciatic hernia causing sciatica: MRI and MR neurography showing entrapment of sciatic nerve". Br J Radiol. 83 (987): e65–6. doi:10.1259/bjr/47866965. PMC 3473559. PMID 20197431.
- ↑ [<"http://www.gnu.org/copyleft/fdl.html">GFDL, <"http://creativecommons.org/licenses/by-sa/3.0/">CC-BY-SA-3.0 or <"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3ABrain_herniation_types.svg">
- ↑ Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. (Own work) [<"http://creativecommons.org/licenses/by/3.0">CC BY 3.0], <"https://commons.wikimedia.org/wiki/File%3ABlausen_0484_HerniatedLumbarDisc.png">
- ↑ Stevens RD, Shoykhet M, Cadena R (2015). "Emergency Neurological Life Support: Intracranial Hypertension and Herniation". Neurocrit Care. 23 Suppl 2: S76–82. doi:10.1007/s12028-015-0168-z. PMC 4791176. PMID 26438459.
- ↑ "Herniated Disc - National Library of Medicine - PubMed Health".
- ↑ Newman BM, Afshani E, Karp MP, Jewett TC, Cooney DR (1986). "Presentation of congenital diaphragmatic hernia past the neonatal period". Arch Surg. 121 (7): 813–6. PMID 3718216.
- ↑ Robnett-Filly B, Goldstein RB, Sampior D, Hom M (2003). "Morgagni hernia: a rare form of congenital diaphragmatic hernia". J Ultrasound Med. 22 (5): 537–9. PMID 12751867.
- ↑ [<"http://creativecommons.org/publicdomain/zero/1.0/deed.en">CC0], <"https://commons.wikimedia.org/wiki/File%3AHiatus_hernia.svg">
- ↑ <"https://en.wikipedia.org/wiki/User:Zyryab" class="extiw" title="wikipedia:User:Zyryab">Zyryab at <"https://en.wikipedia.org/wiki/" class="extiw" title="wikipedia:">English Wikipedia [<"http://www.gnu.org/copyleft/fdl.html">GFDL, <"http://creativecommons.org/licenses/by-sa/3.0/">CC-BY-SA-3.0 or <"http://creativecommons.org/licenses/by/2.5">CC BY 2.5], <"https://commons.wikimedia.org/wiki/File%3ALumbarTriangle.jpg">via Wikimedia Commons
- ↑ Başak F, Hasbahçeci M, Canbak T, Acar A, Şişik A, Baş G; et al. (2017). "Lumbar (Petit's) hernia: A rare entity". Turk J Surg. 33 (3): 220–221. doi:10.5152/UCD.2015.2986. PMC 5602318. PMID 28944339.
- ↑ [<"https://creativecommons.org/licenses/by-sa/2.5">CC BY-SA 2.5], <"https://commons.wikimedia.org/wiki/File%3AErnia_Ombelicale.jpg">
- ↑ [<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3AHernia_epig%C3%A1strica.png">
- ↑ [<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0 or <"http://www.gnu.org/copyleft/fdl.html">GFDL], <"https://commons.wikimedia.org/wiki/File%3AHernia_spiegheli_01.JPG">
- ↑ [<"https://creativecommons.org/licenses/by-sa/3.0">CC BY-SA 3.0], <"https://commons.wikimedia.org/wiki/File%3ADe_Garengeot-Hernie_mit_Appendizitis_-_CT_axial_und_coronar_-_001.jpg">
- ↑ Polat C, Dervisoglu A, Senyurek G, Bilgin M, Erzurumlu K, Ozkan K (2005). "Umbilical hernia repair with the prolene hernia system". Am. J. Surg. 190 (1): 61–4. doi:10.1016/j.amjsurg.2004.09.021. PMID 15972174.
- ↑ Grella R, Razzano S, Lamberti R, Trojaniello B, D'Andrea F, Nicoletti GF (2015). "Combined epigastric hernia repair and mini-abdominoplasty. Case report". Int J Surg Case Rep. 8C: 111–3. doi:10.1016/j.ijscr.2014.10.033. PMC 4353989. PMID 25667986.
- ↑ Kingsnorth A (2006). "The management of incisional hernia". Ann R Coll Surg Engl. 88 (3): 252–60. doi:10.1308/003588406X106324. PMC 1963672. PMID 16719992.
- ↑ Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR (2014). "Amyand's hernia: a review". Med Sci Monit. 20: 140–6. doi:10.12659/MSM.889873. PMC 3915004. PMID 24473371.
- ↑ Malling B, Karlsen AA, Hern J (2017). "Littre Hernia: A Rare Case of an Incarcerated Meckel's Diverticulum". Ultrasound Int Open. 3 (2): E91–E92. doi:10.1055/s-0043-102179. PMC 5462611. PMID 28597002.
- ↑ Kadirov S, Sayfan J, Friedman S, Orda R (1996). "Richter's hernia--a surgical pitfall". J. Am. Coll. Surg. 182 (1): 60–2. PMID 8542091.
- ↑ Carne PW, Robertson GM, Frizelle FA (2003). "Parastomal hernia". Br J Surg. 90 (7): 784–93. doi:10.1002/bjs.4220. PMID 12854101.
- ↑ Bjork KJ, Mucha P, Cahill DR (1988). "Obturator hernia". Surg Gynecol Obstet. 167 (3): 217–22. PMID 3413651.
- ↑ Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P (2010). "Perineal hernia: surgical anatomy, embryology, and technique of repair". Am Surg. 76 (5): 474–9. PMID 20506875.
- ↑ Paquet M, Penney J, Boerboom D (2008). "Lateral femoral hernias in a line of FVB/NHsd mice: a new confounding lesion linked to genetic background?". Comp Med. 58 (4): 395–8. PMC 2706040. PMID 18724783.
- ↑ Rather SA, Dar TI, Malik AA, Parray FQ, Ahmad M, Asrar S (2011). "Sciatic hernia clinically mimicking obturator hernia, missed by ultrasonography: case report". Ulus Travma Acil Cerrahi Derg. 17 (3): 277–9. PMID 21935810.