Ticlopidine: Difference between revisions
No edit summary |
m (Protected "Ticlopidine": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 206: | Line 206: | ||
====Hemorrhagic==== | ====Hemorrhagic==== | ||
Ticlopidine has been associated with increased bleeding, spontaneous posttraumatic bleeding and perioperative [[bleeding]] including, but not limited to, gastrointestinal bleeding. It has also been associated with a number of bleeding complications such as [[ecchymosis]], [[epistaxis]], [[hematuria]] and [[conjunctival hemorrhage]]. | Ticlopidine has been associated with increased bleeding, spontaneous posttraumatic bleeding and perioperative [[bleeding]] including, but not limited to, [[gastrointestinal bleeding]]. It has also been associated with a number of bleeding complications such as [[ecchymosis]], [[epistaxis]], [[hematuria]] and [[conjunctival hemorrhage]]. | ||
[[Intracerebral bleeding]] was rare in clinical trials in stroke patients with ticlopidine, with an incidence no greater than that seen with comparator agents (ticlopidine 0.5%, aspirin 0.6%, placebo 0.75%). It has also been reported postmarketing. | [[Intracerebral bleeding]] was rare in clinical trials in stroke patients with ticlopidine, with an incidence no greater than that seen with comparator agents (ticlopidine 0.5%, aspirin 0.6%, placebo 0.75%). It has also been reported postmarketing. | ||
| Line 459: | Line 459: | ||
[[Category:Cardiovascular Drugs]] | [[Category:Cardiovascular Drugs]] | ||
[[Category:Antiplatelet drugs]] | [[Category:Antiplatelet drugs]] | ||
[[Category:Thienopyridines]] | |||
Latest revision as of 17:16, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning
See full prescribing information for complete Boxed Warning.
Ticlopidine can cause life-threatening hematological adverse reactions, including neutropenia/agranulocytosis, thrombotic thrombocytopenic purpura (TTP) and aplastic anemia.
Neutropenia/Agranulocytosis: Among 2048 patients in clinical trials in stroke patients, there were 50 cases (2.4%) of neutropenia (less than 1200 neutrophils/mm3), and the neutrophil count was below 450/mm3 in 17 of these patients (0.8% of the total population). TTP: One case of thrombotic thrombocytopenic purpura was reported during clinical trials in stroke patients. Based on postmarketing data, US physicians reported about 100 cases between 1992 and 1997. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated TTP may be as high as one case in every 2000 to 4000 patients exposed. Aplastic Anemia: Aplastic anemia was not seen during clinical trials in stroke patients, but US physicians reported about 50 cases between 1992 and 1998. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated aplastic anemia may be as high as one case in every 4000 to 8000 patients exposed. Monitoring of Clinical and Hematologic Status: Severe hematological adverse reactions may occur within a few days of the start of therapy. The incidence of TTP peaks after about 3 to 4 weeks of therapy and neutropenia peaks at approximately 4 to 6 weeks. The incidence of aplastic anemia peaks after about 4 to 8 weeks of therapy. The incidence of the hematologic adverse reactions declines thereafter. Only a few cases of neutropenia, TTP, or aplastic anemia have arisen after more than 3 months of therapy. Hematological adverse reactions cannot be reliably predicted by any identified demographic or clinical characteristics. During the first 3 months of treatment, patients receiving ticlopidine must, therefore, be hematologically and clinically monitored for evidence of neutropenia or TTP. If any such evidence is seen, ticlopidine should be immediately discontinued. |
Overview
Ticlopidine is a platelet aggregation inhibitor that is FDA approved for the prophylaxis of thromboembolic stroke, and subacute stent thrombosis in patients undergoing successful coronary stent implantation.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include rash, abdominal pain, diarrhea, indigestion, loss of appetite, nausea, hemorrhage, leukopenia, dizziness.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Stroke
- Dosing Information
- Recommended dose: 250 mg bid taken with food.
Coronary Artery Stenting
- Dosing Information
- Recommended dose: 250 mg bid taken with food together with antiplatelet doses of aspirin for up to 30 days of therapy following successful stent implantation.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ticlopidine in adult patients.
Non–Guideline-Supported Use
Coronary artery bypass graft
- Dosing Information
Hemodialysis
- Dosing Information
- Recommended dose: 250 mg daily[3]
Acute Ischemic Heart Disease
- Dosing Information
- Recommended dose: 250 mg q12h[4]
Myocardial Infarction
- Dosing Information
- Recommended dose: 250 mg q12h[5]
Prophylaxis for Postoperative Thrombosis
- Dosing Information
- Recommended dose: 250 mg q12h 2 days before surgery until the seventh postoperative day[6]
Rheumatoid arthritis
- Dosing Information
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Ticlopidine FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ticlopidine in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ticlopidine in pediatric patients.
Contraindications
- Hypersensitivity to the drug
- Presence of hematopoietic disorders such as neutropenia and thrombocytopenia or a past history of either TTP or aplastic anemia.
- Presence of a hemostatic disorder or active pathological bleeding (such as bleeding peptic ulcer or intracranial bleeding)
- Patients with severe liver impairment
Warnings
|
Warning
See full prescribing information for complete Boxed Warning.
Ticlopidine can cause life-threatening hematological adverse reactions, including neutropenia/agranulocytosis, thrombotic thrombocytopenic purpura (TTP) and aplastic anemia.
Neutropenia/Agranulocytosis: Among 2048 patients in clinical trials in stroke patients, there were 50 cases (2.4%) of neutropenia (less than 1200 neutrophils/mm3), and the neutrophil count was below 450/mm3 in 17 of these patients (0.8% of the total population). TTP: One case of thrombotic thrombocytopenic purpura was reported during clinical trials in stroke patients. Based on postmarketing data, US physicians reported about 100 cases between 1992 and 1997. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated TTP may be as high as one case in every 2000 to 4000 patients exposed. Aplastic Anemia: Aplastic anemia was not seen during clinical trials in stroke patients, but US physicians reported about 50 cases between 1992 and 1998. Based on an estimated patient exposure of 2 million to 4 million, and assuming an event reporting rate of 10% (the true rate is not known), the incidence of ticlopidine-associated aplastic anemia may be as high as one case in every 4000 to 8000 patients exposed. Monitoring of Clinical and Hematologic Status: Severe hematological adverse reactions may occur within a few days of the start of therapy. The incidence of TTP peaks after about 3 to 4 weeks of therapy and neutropenia peaks at approximately 4 to 6 weeks. The incidence of aplastic anemia peaks after about 4 to 8 weeks of therapy. The incidence of the hematologic adverse reactions declines thereafter. Only a few cases of neutropenia, TTP, or aplastic anemia have arisen after more than 3 months of therapy. Hematological adverse reactions cannot be reliably predicted by any identified demographic or clinical characteristics. During the first 3 months of treatment, patients receiving ticlopidine must, therefore, be hematologically and clinically monitored for evidence of neutropenia or TTP. If any such evidence is seen, ticlopidine should be immediately discontinued. |
General
- Ticlopidine should be used with caution in patients who may be at risk of increased bleeding from trauma, surgery or pathological conditions.
- If it is desired to eliminate the antiplatelet effects of ticlopidine prior to elective surgery, the drug should be discontinued 10 to 14 days prior to surgery.
- Several controlled clinical studies have found increased surgical blood loss in patients undergoing surgery during treatment with ticlopidine.
- In TASS and CATS it was recommended that patients have ticlopidine discontinued prior to elective surgery.
- Several hundred patients underwent surgery during the trials, and no excessive surgical bleeding was reported.
- Prolonged bleeding time is normalized within 2 hours after administration of 20 mg methylprednisolone IV.
- Platelet transfusions may also be used to reverse the effect of ticlopidine on bleeding.
- Because platelet transfusions may accelerate thrombosis in patients with TTP on ticlopidine, they should, if possible, be avoided.
GI Bleeding
- Ticlopidine prolongs template bleeding time.
- The drug should be used with caution in patients who have lesions with a propensity to bleed (such as ulcers).
- Drugs that might induce such lesions should be used with caution in patients on ticlopidine
Cholesterol Elevation
- Ticlopidine therapy causes increased serum cholesterol and triglycerides.
- Serum total cholesterol levels are increased 8% to 10% within 1 month of therapy and persist at that level.
- The ratios of the lipoprotein subfractions are unchanged.
Anticoagulant Drugs
- The tolerance and long-term safety of coadministration of ticlopidine with heparin, oral anticoagulants or fibrinolytic agents have not been established.
- In trials for cardiac stenting, patients received heparin and ticlopidine concomitantly for approximately 12 hours.
- If a patient is switched from an anticoagulant or fibrinolytic drug to ticlopidine, the former drug should be discontinued prior to ticlopidine administration.
Liver Function
- Ticlopidine therapy has been associated with elevations of alkaline phosphatase, bilirubin, and transaminases, which generally occurred within 1 to 4 months of therapy initiation.
- In controlled clinical trials in stroke patients, the incidence of elevated alkaline phosphatase (greater than two times upper limit of normal) was 7.6% in ticlopidine patients, 6% in placebo patients and 2.5% in aspirin patients.
- The incidence of elevated AST (SGOT) (greater than two times upper limit of normal) was 3.1% in ticlopidine patients, 4% in placebo patients and 2.1% in aspirin patients. No progressive increases were observed in closely monitored clinical trials (eg, no transaminase greater than 10 times the upper limit of normal was seen), but most patients with these abnormalities had therapy discontinued.
- Occasionally patients had developed minor elevations in bilirubin.
- Postmarketing experience includes rare individuals with elevations in their transaminases and bilirubin to >10X above the upper limits of normal.
- Based on postmarketing and clinical trial experience, liver function testing, including ALT, AST, and GGT, should be considered whenever liver dysfunction is suspected, particularly during the first 4 months of treatment.
Adverse Reactions
Clinical Trials Experience
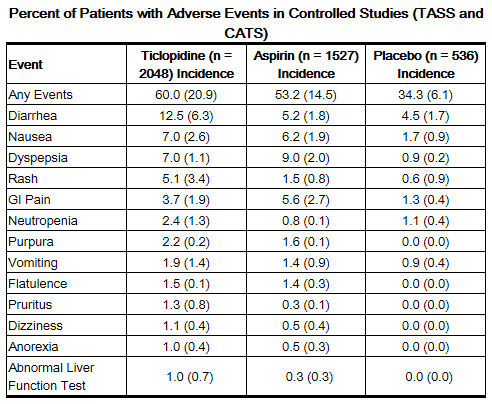
Adverse reactions in stroke patients were relatively frequent with over 50% of patients reporting at least one. Most (30% to 40%) involved the gastrointestinal tract. Most adverse effects are mild, but 21% of patients discontinued therapy because of an adverse event, principally diarrhea, rash, nausea, vomiting, GI pain and neutropenia. Most adverse effects occur early in the course of treatment, but a new onset of adverse effects can occur after several months.
The incidence rates of adverse events listed in the following table were derived from multicenter, controlled clinical trials in stroke patients described above comparing ticlopidine, placebo and aspirin over study periods of up to 5.8 years. Adverse events considered by the investigator to be probably drug-related that occurred in at least 1% of patients treated with ticlopidine are shown in the following table:
Hematological
Neutropenia
Neutropenia may occur suddenly. Bone marrow examination typically shows a reduction in white blood cell precursors. After withdrawal of ticlopidine, the neutrophil count usually rises to >1200/mm3 within 1 to 3 weeks.
Thrombocytopenia
Rarely, thrombocytopenia may occur in isolation or together with neutropenia.
Thrombotic Thrombocytopenic Purpura (TTP)
TTP is characterized by thrombocytopenia, microangiopathic hemolytic anemia (schistocytes [fragmented RBCs] seen on peripheral smear), neurological findings, renal dysfunction, and fever. The signs and symptoms can occur in any order, in particular, clinical symptoms may precede laboratory findings by hours or days. With prompt treatment (often including plasmapheresis), 70% to 80% of patients will survive with minimal or no sequelae. Because platelet transfusions may accelerate thrombosis in patients with TTP on ticlopidine, they should, if possible, be avoided.
Aplastic Anemia
Aplastic anemia is characterized by anemia, thrombocytopenia and neutropenia together with a bone marrow examination that shows decreases in the precursor cells for red blood cells, white blood cells, and platelets. Patients may present with signs or symptoms suggestive of infection, in association with low white blood cell and platelet counts. Prompt treatment, which may include the use of drugs to stimulate the bone marrow, can minimize the mortality associated with aplastic anemia.
Other Hematological Effects
Rare cases of agranulocytosis, pancytopenia, or leukemia have been reported in postmarketing experience, some of which have been fatal. All forms of hematological adverse reactions are potentially fatal.
Gastrointestinal
Ticlopidine therapy has been associated with a variety of gastrointestinal complaints including diarrhea and nausea. The majority of cases are mild, but about 13% of patients discontinued therapy because of these. They usually occur within 3 months of initiation of therapy and typically are resolved within 1 to 2 weeks without discontinuation of therapy. If the effect is severe or persistent, therapy should be discontinued. In some cases of severe or bloody diarrhea, colitis was later diagnosed.
Hemorrhagic
Ticlopidine has been associated with increased bleeding, spontaneous posttraumatic bleeding and perioperative bleeding including, but not limited to, gastrointestinal bleeding. It has also been associated with a number of bleeding complications such as ecchymosis, epistaxis, hematuria and conjunctival hemorrhage.
Intracerebral bleeding was rare in clinical trials in stroke patients with ticlopidine, with an incidence no greater than that seen with comparator agents (ticlopidine 0.5%, aspirin 0.6%, placebo 0.75%). It has also been reported postmarketing.
Rash
Ticlopidine has been associated with a maculopapular or urticarial rash (often with pruritus). Rash usually occurs within 3 months of initiation of therapy with a mean onset time of 11 days. If drug is discontinued, recovery occurs within several days. Many rashes do not recur on drug rechallenge. There have been rare reports of severe rashes, including Stevens-Johnson syndrome, erythema multiforme and exfoliative dermatitis.
Less Frequent Adverse Reactions (Probably Related)
Clinical adverse experiences occurring in 0.5% to 1.0% of stroke patients in controlled trials include:
- Digestive System: GI fullness
- Skin and Appendages: urticaria
- Nervous System: headache
- Hemostatic System: epistaxis
- Special Senses: tinnitus
Postmarketing Experience
In addition, rarer, relatively serious and potentially fatal events associated with the use of ticlopidine have also been reported from postmarketing experience:
- Hemolytic anemia with reticulocytosis
- Immune thrombocytopenia
- Hepatitis
- Hepatocellular jaundice
- Cholestatic jaundice
- Hepatic necrosis
- Hepatic failure
- Peptic ulcer
- Renal failure
- Nephrotic syndrome
- Hyponatremia
- Vasculitis
- Sepsis
- Allergic reactions (including angioedema, allergic pneumonitis, and anaphylaxis)
- Systemic lupus (positive ANA)
- Peripheral neuropathy
- Serum sickness
- Arthropathy
- Myositis
Drug Interactions
Therapeutic doses of ticlopidine caused a 30% increase in the plasma half-life of antipyrine and may cause analogous effects on similarly metabolized drugs. Therefore, the dose of drugs metabolized by hepatic microsomal enzymes with low therapeutic ratios or being given to patients with hepatic impairment may require adjustment to maintain optimal therapeutic blood levels when starting or stopping concomitant therapy with ticlopidine. Studies of specific drug interactions yielded the following results:
Aspirin and other NSAIDs
Ticlopidine potentiates the effect of aspirin or other NSAIDs on platelet aggregation. The safety of concomitant use of ticlopidine and NSAIDs has not been established. The safety of concomitant use of ticlopidine and aspirin beyond 30 days has not been established. Aspirin did not modify the ticlopidine-mediated inhibition of ADP-induced platelet aggregation, but ticlopidine potentiated the effect of aspirin on collagen-induced platelet aggregation. Caution should be exercised in patients who have lesions with a propensity to bleed, such as ulcers. Long-term concomitant use of aspirin and ticlopidine is not recommended.
Antacids
Administration of ticlopidine after antacids resulted in an 18% decrease in plasma levels of ticlopidine.
Cimetidine
Chronic administration of cimetidine reduced the clearance of a single dose of ticlopidine by 50%.
Digoxin
Coadministration of ticlopidine with digoxin resulted in a slight decrease (approximately 15%) in digoxin plasma levels. Little or no change in therapeutic efficacy of digoxin would be expected.
Theophylline
In normal volunteers, concomitant administration of ticlopidine resulted in a significant increase in the theophylline elimination half-life from 8.6 to 12.2 hours and a comparable reduction in total plasma clearance of theophylline.
Phenobarbital
In 6 normal volunteers, the inhibitory effects of ticlopidine on platelet aggregation were not altered by chronic administration of phenobarbital.
Phenytoin
In vitro studies demonstrated that ticlopidine does not alter the plasma protein binding of phenytoin. However, the protein binding interactions of ticlopidine and its metabolites have not been studied in vivo. Several cases of elevated phenytoin plasma levels with associated somnolence and lethargy have been reported following coadministration with ticlopidine. Caution should be exercised in coadministering this drug with ticlopidine, and it may be useful to remeasure phenytoin blood concentrations.
Propranolol
In vitro studies demonstrated that ticlopidine does not alter the plasma protein binding of propranolol. However, the protein binding interactions of ticlopidine and its metabolites have not been studied in vivo. Caution should be exercised in coadministering this drug with ticlopidine.
Other Concomitant Therapy
Although specific interaction studies were not performed, in clinical studies ticlopidine was used concomitantly with beta blockers, calcium channel blockers and diuretics without evidence of clinically significant adverse interactions.
Food Interaction
The oral bioavailability of ticlopidine is increased by 20% when taken after a meal. Administration of ticlopidine with food is recommended to maximize gastrointestinal tolerance. In controlled trials in stroke patients, ticlopidine was taken with meals.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B
Teratology studies have been conducted in mice (doses up to 200 mg/kg/day), rats (doses up to 400 mg/kg/day) and rabbits (doses up to 200 mg/kg/day). Doses of 400 mg/kg in rats, 200 mg/kg/day in mice and 100 mg/kg in rabbits produced maternal toxicity, as well as fetal toxicity, but there was no evidence of a teratogenic potential of ticlopidine. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of a human response, this drug should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS): B1
Drugs which have been taken by only a limited number of pregnant women and women of childbearing age, without an increase in the frequency of malformation or other direct or indirect harmful effects on the human fetus having been observed. Studies in animals have not shown evidence of an increased occurrence of fetal damage.
Labor and Delivery
There is no FDA guidance on use of Ticlopidine during labor and delivery.
Nursing Mothers
Studies in rats have shown ticlopidine is excreted in the milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from ticlopidine, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
Clearance of ticlopidine is somewhat lower in elderly patients and trough levels are increased. The major clinical trials with ticlopidine in stroke patients were conducted in an elderly population with an average age of 64 years. Of the total number of patients in the therapeutic trials, 45% of patients were over 65 years old and 12% were over 75 years old. No overall differences in effectiveness or safety were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Ticlopidine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ticlopidine with respect to specific racial populations.
Renal Impairment
Patients with mildly (Ccr 50 to 80 mL/min) or moderately (Ccr 20 to 50 mL/min) impaired renal function were compared to normal subjects (Ccr 80 to 150 mL/min) in a study of the pharmacokinetic and platelet pharmacodynamic effects of ticlopidine (250 mg bid) for 11 days. Concentrations of unchanged ticlopidine were measured after a single 250-mg dose and after the final 250-mg dose on Day 11.
AUC values of ticlopidine increased by 28% and 60% in mild and moderately impaired patients, respectively, and plasma clearance decreased by 37% and 52%, respectively, but there were no statistically significant differences in ADP-induced platelet aggregation. In this small study (26 patients), bleeding times showed significant prolongation only in the moderately impaired patients.
Hepatic Impairment
Since ticlopidine is metabolized by the liver, dosing of ticlopidine or other drugs metabolized in the liver may require adjustment upon starting or stopping concomitant therapy. Because of limited experience in patients with severe hepatic disease, who may have bleeding diatheses, the use of ticlopidine is not recommended in this population
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ticlopidine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ticlopidine in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
Starting just before initiating treatment and continuing through the third month of therapy, patients receiving ticlopidine must be monitored every 2 weeks. Because of ticlopidine’s long plasma half-life, patients who discontinue ticlopidine during this 3-month period should continue to be monitored for 2 weeks after discontinuation. More frequent monitoring, and monitoring after the first 3 months of therapy, is necessary only in patients with clinical signs (eg, signs or symptoms suggestive of infection) or laboratory signs (eg, neutrophil count less than 70% of the baseline count, decrease in hematocrit or platelet count) that suggest incipient hematological adverse reactions.
Clinically, fever might suggest neutropenia, TTP, or aplastic anemia; TTP might also be suggested by weakness, pallor, petechiae or purpura, dark urine (due to blood, bile pigments, or hemoglobin) or jaundice, or neurological changes. Patients should be told to discontinue ticlopidine and to contact the physician immediately upon the occurrence of any of these findings.
Laboratory monitoring should include a complete blood count, with special attention to the absolute neutrophil count (WBC x % neutrophils), platelet count, and the appearance of the peripheral smear. Ticlopidine is occasionally associated with thrombocytopenia unrelated to TTP or aplastic anemia. Any acute, unexplained reduction in hemoglobin or platelet count should prompt further investigation for a diagnosis of TTP, and the appearance of schistocytes (fragmented RBCs) on the smear should be treated as presumptive evidence of TTP. A simultaneous decrease in platelet count and WBC count should prompt further investigation for a diagnosis of aplastic anemia. If there are laboratory signs of TTP or aplastic anemia, or if the neutrophil count is confirmed to be <1200/mm3, then ticlopidine should be discontinued immediately.
IV Compatibility
There is limited information regarding the compatibility of Ticlopidine and IV administrations.
Overdosage
One case of deliberate overdosage with ticlopidine has been reported by a foreign postmarketing surveillance program. A 38-year-old male took a single 6000-mg dose of ticlopidine hydrochloride (equivalent to 24 standard 250-mg tablets). The only abnormalities reported were increased bleeding time and increased SGPT. No special therapy was instituted and the patient recovered without sequelae.
Single oral doses of ticlopidine at 1600 mg/kg and 500 mg/kg were lethal to rats and mice, respectively. Symptoms of acute toxicity were GI hemorrhage, convulsions, hypothermia, dyspnea, loss of equilibrium and abnormal gait.
Pharmacology

| |

| |
Ticlopidine
| |
| Systematic (IUPAC) name | |
| 5-(2-chlorobenzyl)-4,5,6,7-tetrahydrothieno[3,2-c]pyridine | |
| Identifiers | |
| CAS number | |
| ATC code | B01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 263.786 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | >80% |
| Protein binding | 98% |
| Metabolism | Hepatic |
| Half life |
|
| Excretion | Renal and fecal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral |
Mechanism of Action
When taken orally, ticlopidine hydrochloride causes a time- and dose-dependent inhibition of both platelet aggregation and release of platelet granule constituents, as well as a prolongation of bleeding time. The intact drug has no significant in vitro activity at the concentrations attained in vivo; and, although analysis of urine and plasma indicates at least 20 metabolites, no metabolite which accounts for the activity of ticlopidine has been isolated.
Ticlopidine hydrochloride, after oral ingestion, interferes with platelet membrane function by inhibiting ADP-induced platelet-fibrinogen binding and subsequent platelet-platelet interactions. The effect on platelet function is irreversible for the life of the platelet, as shown both by persistent inhibition of fibrinogen binding after washing platelets ex vivo and by inhibition of platelet aggregation after resuspension of platelets in buffered medium.
Structure
Ticlopidine hydrochloride is a platelet aggregation inhibitor. Chemically it is 5-[(2-chlorophenyl)methyl]-4,5,6,7-tetrahydrothieno [3,2-c] pyridine hydrochloride. The structural formula is:

Ticlopidine hydrochloride is a white crystalline solid. It is freely soluble in water and self-buffers to a pH of 3.6. It also dissolves freely in methanol, is sparingly soluble in methylene chloride and ethanol, slightly soluble in acetone and insoluble in a buffer solution of pH 6.3.
Pharmacodynamics
In healthy volunteers over the age of 50, substantial inhibition (over 50%) of ADP-induced platelet aggregation is detected within 4 days after administration of ticlopidine hydrochloride 250 mg bid, and maximum platelet aggregation inhibition (60% to 70%) is achieved after 8 to 11 days. Lower doses cause less, and more delayed, platelet aggregation inhibition, while doses above 250 mg bid give little additional effect on platelet aggregation but an increased rate of adverse effects. The dose of 250 mg bid is the only dose that has been evaluated in controlled clinical trials.
After discontinuation of ticlopidine hydrochloride, bleeding time and other platelet function tests return to normal within 2 weeks, in the majority of patients.
At the recommended therapeutic dose (250 mg bid), ticlopidine hydrochloride has no known significant pharmacological actions in man other than inhibition of platelet function and prolongation of the bleeding time.
Pharmacokinetics
After oral administration of a single 250-mg dose, ticlopidine hydrochloride is rapidly absorbed with peak plasma levels occurring at approximately 2 hours after dosing and is extensively metabolized. Absorption is greater than 80%. Administration after meals results in a 20% increase in the AUC of ticlopidine.
Ticlopidine hydrochloride displays nonlinear pharmacokinetics and clearance decreases markedly on repeated dosing. In older volunteers the apparent half-life of ticlopidine after a single 250-mg dose is about 12.6 hours; with repeat dosing at 250 mg bid, the terminal elimination half-life rises to 4 to 5 days and steady-state levels of ticlopidine hydrochloride in plasma are obtained after approximately 14 to 21 days.
Ticlopidine hydrochloride binds reversibly (98%) to plasma proteins, mainly to serum albumin and lipoproteins. The binding to albumin and lipoproteins is nonsaturable over a wide concentration range. Ticlopidine also binds to alpha-1 acid glycoprotein. At concentrations attained with the recommended dose, only 15% or less ticlopidine in plasma is bound to this protein.
Ticlopidine hydrochloride is metabolized extensively by the liver; only trace amounts of intact drug are detected in the urine. Following an oral dose of radioactive ticlopidine hydrochloride administered in solution, 60% of the radioactivity is recovered in the urine and 23% in the feces. Approximately 1/3 of the dose excreted in the feces is intact ticlopidine hydrochloride, possibly excreted in the bile. Ticlopidine hydrochloride is a minor component in plasma (5%) after a single dose, but at steady-state is the major component (15%). Approximately 40% to 50% of the radioactive metabolites circulating in plasma are covalently bound to plasma proteins, probably by acylation.
Clearance of ticlopidine decreases with age. Steady-state trough values in elderly patients (mean age 70 years) are about twice those in younger volunteer populations.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year oral carcinogenicity study in rats, ticlopidine at daily doses of up to 100 mg/kg (610 mg/m2) was not tumorigenic. For a 70-kg person (1.73 m2 body surface area) the dose represents 14 times the recommended clinical dose on a mg/kg basis and two times the clinical dose on body surface area basis. In a 78-week oral carcinogenicity study in mice, ticlopidine at daily doses up to 275 mg/kg (1180 mg/m2) was not tumorigenic. The dose represents 40 times the recommended clinical dose on a mg/kg basis and four times the clinical dose on body surface area basis.
Ticlopidine was not mutagenic in vitro in the Ames test, the rat hepatocyte DNA-repair assay, or the Chinese-hamster fibroblast chromosomal aberration test; or in vivo in the mouse spermatozoid morphology test, the Chinese-hamster micronucleus test, or the Chinese-hamster bone-marrow-cell sister-chromatid exchange test. Ticlopidine was found to have no effect on fertility of male and female rats at oral doses up to 400 mg/kg/day.
Clinical Studies
Stroke Patients
The effect of ticlopidine on the risk of stroke and cardiovascular events was studied in two multicenter, randomized, double-blind trials.
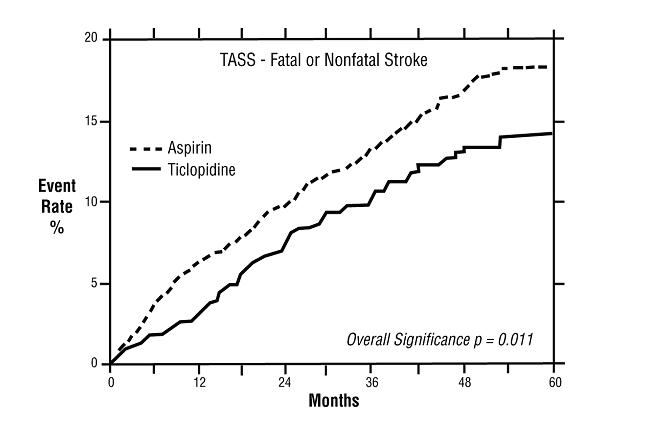
Study in Patients Experiencing Stroke Precursors
In a trial comparing ticlopidine and aspirin (The Ticlopidine Aspirin Stroke Study or TASS), 3069 patients (1987 men, 1082 women) who had experienced such stroke precursors as transient ischemic attack (TIA), transient monocular blindness (amaurosis fugax), reversible ischemic neurological deficit or minor stroke, were randomized to ticlopidine 250 mg bid or aspirin 650 mg bid. The study was designed to follow patients for at least 2 years and up to 5 years.
Over the duration of the study, ticlopidine significantly reduced the risk of fatal and nonfatal stroke by 24% (p =.011) from 18.1 to 13.8 per 100 patients followed for 5 years, compared to aspirin. During the first year, when the risk of stroke is greatest, the reduction in risk of stroke (fatal and nonfatal) compared to aspirin was 48%; the reduction was similar in men and women.
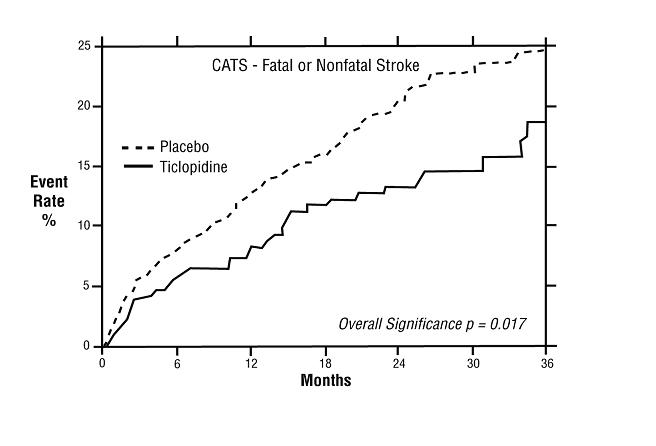
Study in Patients Who Had a Completed Atherothrombotic Stroke
In a trial comparing ticlopidine with placebo (The Canadian American Ticlopidine Study or CATS) 1073 patients who had experienced a previous atherothrombotic stroke were treated with ticlopidine 250 mg bid or placebo for up to 3 years.
Ticlopidine significantly reduced the overall risk of stroke by 24% (p=.017) from 24.6 to 18.6 per 100 patients followed for 3 years, compared to placebo. During the first year the reduction in risk of fatal and nonfatal stroke over placebo was 33%.
Stent Patients
The ability of ticlopidine to reduce the rate of thrombotic events after the placement of coronary artery stents has been studied in five randomized trials, one of substantial size (Stent Anticoagulation Restenosis Study or STARS) described below, and four smaller studies. In these trials, ticlopidine 250 mg bid with ASA (dose range from 100 mg bid to 325 mg qd) was compared to aspirin alone or to anticoagulant therapy plus aspirin. The trials enrolled patients undergoing both planned (elective) and unplanned coronary stent placement. The types of stents used, the use of intravascular ultrasound, and the use of high-pressure stent deployment varied among the trials, although all patients in STARS received a Palmaz-Schatz stent. The primary efficacy endpoints of the trials were similar, and included death, myocardial infarction and the need for repeat coronary angioplasty or CABG. All trials followed patients for at least 30 days.
In STARS, patients were randomized to receive one of three regimens for 4 weeks: aspirin alone, aspirin plus coumadin, or aspirin plus ticlopidine. Therapy was initiated following successful coronary stent placement. The primary endpoint was the incidence of stent thrombosis, defined as death, Q-Wave MI, or angiographic thrombus within the stented vessel demonstrated at the time of documented ischemia requiring emergent revascularization. The incidence rates for the primary endpoint and its components at 30 days are shown in the table below.

The use of ticlopidine plus aspirin did not affect the rate of non-Q-wave MIs when compared with aspirin alone or aspirin plus anticoagulants in STARS.
The use of ticlopidine plus aspirin was associated with a lower rate of recurrent cardiovascular events when compared with aspirin alone or aspirin plus anticoagulants in the other four randomized trials.
The rate of serious bleeding complications and neutropenia in STARS are shown in the table below. There were no cases of thrombotic thrombocytopenic purpura (TTP) or aplastic anemia reported in 1346 patients who received ticlopidine plus aspirin in the five randomized trials.

How Supplied
Ticlopidine tablets are available as white to off-white, oval, film-coated, unscored, 250 mg tablets, debossed with “93” on one side and “154”on the other. They are packaged in bottles of 100 (NDC 42291-803-01)
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
Storage
Store at controlled room temperature, between 20° and 25°C (68° and 77°F).
Images
Drug Images
{{#ask: Page Name::Ticlopidine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Ticlopidine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patients should be told that a decrease in the number of white blood cells (neutropenia) or platelets (thrombocytopenia) can occur with ticlopidine, especially during the first 3 months of treatment and that neutropenia, if it is severe, can result in an increased risk of infection. They should be told it is critically important to obtain the scheduled blood tests to detect neutropenia or thrombocytopenia. Patients should also be reminded to contact their physicians if they experience any indication of infection such as fever, chills, or sore throat, any of which might be a consequence of neutropenia. Thrombocytopenia may be part of a syndrome called TTP. Symptoms and signs of TTP, such as fever, weakness, difficulty speaking, seizures, yellowing of skin or eyes, dark or bloody urine, pallor or petechiae (pinpoint hemorrhagic spots on the skin), should be reported immediately.
All patients should be told that it may take them longer than usual to stop bleeding when they take ticlopidine and that they should report any unusual bleeding to their physician. Patients should tell physicians and dentists that they are taking ticlopidine before any surgery is scheduled and before any new drug is prescribed.
Patients should be told to promptly report side effects of ticlopidine such as severe or persistent diarrhea, skin rashes or subcutaneous bleeding or any signs of cholestasis, such as yellow skin or sclera, dark urine, or light-colored stools.
Patients should be told to take ticlopidine with food or just after eating in order to minimize gastrointestinal discomfort.
Precautions with Alcohol
Alcohol-Ticlopidine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Ticlid
- Ticlopidine
Look-Alike Drug Names
- Ticlid - Tequin
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ M. E. Rothlin, N. Pfluger, K. Speiser, N. Goebel, H. P. Krayenbuhl, W. Steinbrunn, M. Turina & A. Senning (1985). "Platelet inhibitors versus anticoagulants for prevention of aorto-coronary bypass graft occlusion". European heart journal. 6 (2): 168–175. PMID 3891348. Unknown parameter
|month=ignored (help) - ↑ R. Limet, J. L. David, P. Magotteaux, M. P. Larock & P. Rigo (1987). "Prevention of aorta-coronary bypass graft occlusion. Beneficial effect of ticlopidine on early and late patency rates of venous coronary bypass grafts: a double-blind study". The Journal of thoracic and cardiovascular surgery. 94 (5): 773–783. PMID 3312825. Unknown parameter
|month=ignored (help) - ↑ S. Milutinovic, V. Gasparovic, E. Milutinovic & J. Buturovic-Ponikvar (1993). "Ticlopidine improves dialysis clearance of solutes in uremic patients by reducing blood clotting in dialyser fibers". The International journal of artificial organs. 16 (5): 249–252. PMID 8354583. Unknown parameter
|month=ignored (help) - ↑ F. Balsano, P. Rizzon, F. Violi, D. Scrutinio, C. Cimminiello, F. Aguglia, C. Pasotti & G. Rudelli (1990). "Antiplatelet treatment with ticlopidine in unstable angina. A controlled multicenter clinical trial. The Studio della Ticlopidina nell'Angina Instabile Group". Circulation. 82 (1): 17–26. PMID 2194694. Unknown parameter
|month=ignored (help) - ↑ J. B. Knudsen, E. Kjoller, K. Skagen & J. Gormsen (1985). "The effect of ticlopidine on platelet functions in acute myocardial infarction. A double blind controlled trial". Thrombosis and haemostasis. 53 (3): 332–336. PMID 3901391. Unknown parameter
|month=ignored (help) - ↑ E. J. Brommer (1981). "The effect of Ticlopidine upon platelet function, haemorrhage and post-operative thrombosis in patients undergoing suprapubic prostatectomy". The Journal of international medical research. 9 (3): 203–210. PMID 7238995.
- ↑ M. G. Grimaldi (1985). "Long-term low dose ticlopidine treatment in rheumatoid arthritis: effects on serum sulphydryl levels, technetium index, erythrocyte sedimentation rate, and clinical disease activity". European journal of clinical pharmacology. 29 (2): 165–168. PMID 3000794.
- ↑ G. Ciuffetti, A. Ciacca, M. Mercuri, R. Lombardini, G. Maragoni & A. M. Scarponi (1989). "Correlation between clinical and laboratory findings when the whole blood filterability rate is modified by ticlopidine in the treatment of rheumatoid arthritis". British journal of rheumatology. 28 (5): 424–427. PMID 2790405. Unknown parameter
|month=ignored (help)
{{#subobject:
|Label Page=Ticlopidine |Label Name=Ticlopidine label.jpg
}}
{{#subobject:
|Label Page=Ticlopidine |Label Name=Ticlopidine FDA panel.png
}}