Statin induced myopathy medical therapy
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby
|
Statin induced myopathy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Statin induced myopathy medical therapy On the Web |
|
American Roentgen Ray Society Images of Statin induced myopathy medical therapy |
|
Risk calculators and risk factors for Statin induced myopathy medical therapy |
Overview
When symptoms of myopathy or elevation of creatine kinase occur in the setting of a patient taking statins, the majority of patients may safely continue the treatment with statins. The decision on whether the patient can discontinue or continue statins depends on two factors: the severity of the symptoms and the severity of the increase in the creatine kinase level. Statins can be safely continued when the symptoms are tolerable and the creatine kinase is elevated less than 5 times the upper limits of normal. Otherwise, if the creatine kinase level is higher than five times the upper limit of normal or if the symptoms are intolerable regardless of the level of creatine kinse, statins should be stopped for a certain period of time and restarted again with lower doses or with different types of statins. The role of vitamin D and coenzyme Q10 is still controversial in the management of statin induced myopathy as no studies support their use yet.[1][2][3]<
Treatment
The decision on whether the patient can discontinue or continue statin depends on two factors:
- The severity of the symptoms
- The increase in the creatine kinase level.
Tolerable Symptoms with Absent or Mild Elevation of Creatine Kinase<5ULN
- If statin had been stopped, may often be resumed[4].
- Continue statin[5]
- Consider lowering the dose of statin, adjust the optimal dose of statin depending on the symptoms of the patient
Tolerable Symptoms with Absent or Mild Elevation of Creatine Kinase>5ULN or with Rhabdomyolysis
- Discontinue statin
- Ensure an appropriate management for rhabdomyolysis if present by good hydration and follow up[1]
- Resume the treatment with statin once the symptoms are resolved. Modify the treatment regimen as follows:
- Monitor creatinine kinase levels.
Intolerable Symptoms
Discontinue statin regardless of the level of the creatine kinase.[1]
Resume the treatment with statin once the symptoms are resolved. Modify the treatment regimen as follows:
- Reduce the dosage of statin
- Reduce the frequency of dosing[7]
- Alternate day dosing, especially of atorvastatin and rosuvastatin[8]
- Twice weekly dosing with longer half lives statins[6]
- Rosuvastatin once a week at 2.5 mg to 20 mg a week (mean 10 +/- 4 mg)[9]
- Different type of statin.[1]
- Monitor creatinine kinase levels.
Recurrence of Symptoms
If the symptoms recur despite appropriate management consider combination therapy with ezetimibe:
- Rosuvastatin: daily, low dose (2.5-5 mg/day) or alternate-day dose or weekly[10]
- Atorvastatin: either alternate-day dose (5-10 mg) or 10 mg twice weekly[11]
Other lipid lowering drugs[12]
Lifestyle changes including diet and exercise
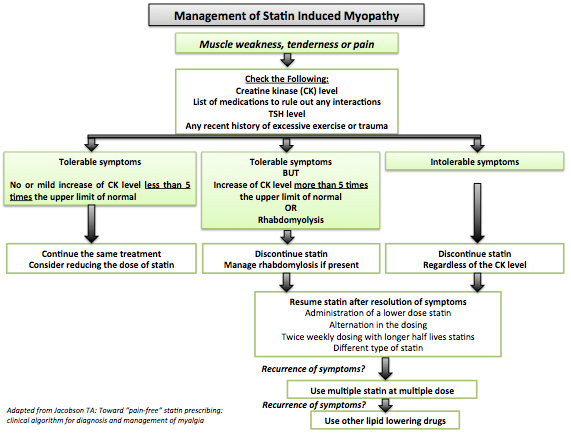
- Shown below is an image summarizing the management plan for statin induced myopathy.[13]
Vitamin D
Several studies have evaluated the role of vitamin D in statin induced myopathy. The results have shown so far no significant relation between the vitamin D level and statin induced myopathy; however, the results of other studies are still pending. Hence, it is not recommended yet to take vitamin D as part of a treatment for statin induced myopathy. Nevertheless, it is important to check for the vitamin D level as vitamin D deficiency is common and it can cause symptoms of myalgia independently from statin use.[3][14]
Coenzyme Q10
- Coenzyme Q10 is found in complex I or II of the electron transport chain and it plays a role as an antioxidant in mitochondrial lipid membrane. Coenzyme Q10 also inhibits apoptosis induced by statins.[15]
- As statins inhibit the synthesis of cholesterol by decreasing the production of mevalonate, a precursor for both cholesterol and coenzyme Q10, they cause coenzyme Q10 deficiency and subsequent mitochondrial dysfunction.[5]
- No current data supports the use of ubiquinone (coenzyme Q10) use for the treatment of statin induced myalgia[16][17]. However, it was proven to be safe to be used but with uncertain efficiency. More evidence based studies are required to provide recommendations for or against its use.[2]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Harper CR, Jacobson TA (2010). "Evidence-based management of statin myopathy". Curr Atheroscler Rep. 12 (5): 322–30. doi:10.1007/s11883-010-0120-9. PMID 20628837.
- ↑ 2.0 2.1 Wyman M, Leonard M, Morledge T (2010). "Coenzyme Q10: a therapy for hypertension and statin-induced myalgia?". Cleve Clin J Med. 77 (7): 435–42. doi:10.3949/ccjm.77a.09078. PMID 20601617.
- ↑ 3.0 3.1 Linde R, Peng L, Desai M, Feldman D (2010). "The role of vitamin D and SLCO1B1*5 gene polymorphism in statin-associated myalgias". Dermatoendocrinol. 2 (2): 77–84. doi:10.4161/derm.2.2.13509. PMC 3081682. PMID 21547103.
- ↑ Zhang H, Plutzky J, Skentzos S, Morrison F, Mar P, Shubina M; et al. (2013). "Discontinuation of statins in routine care settings: a cohort study". Ann Intern Med. 158 (7): 526–34. doi:10.7326/0003-4819-158-7-201304020-00004. PMC 3692286. PMID 23546564.
- ↑ 5.0 5.1 Blaier O, Lishner M, Elis A (2011). "Managing statin-induced muscle toxicity in a lipid clinic". J Clin Pharm Ther. 36 (3): 336–41. doi:10.1111/j.1365-2710.2011.01254.x. PMID 21414023.
- ↑ 6.0 6.1 Gadarla M, Kearns AK, Thompson PD (2008). "Efficacy of rosuvastatin (5 mg and 10 mg) twice a week in patients intolerant to daily statins". Am J Cardiol. 101 (12): 1747–8. doi:10.1016/j.amjcard.2008.02.061. PMID 18549851.
- ↑ Mancini GB, Tashakkor AY, Baker S, Bergeron J, Fitchett D, Frohlich J; et al. (2013). "Diagnosis, prevention, and management of statin adverse effects and intolerance: Canadian Working Group Consensus update". Can J Cardiol. 29 (12): 1553–68. doi:10.1016/j.cjca.2013.09.023. PMID 24267801.
- ↑ Awad K, Mikhailidis DP, Toth PP, Jones SR, Moriarty P, Lip GYH; et al. (2017). "Efficacy and Safety of Alternate-Day Versus Daily Dosing of Statins: a Systematic Review and Meta-Analysis". Cardiovasc Drugs Ther. 31 (4): 419–431. doi:10.1007/s10557-017-6743-0. PMID 28741244.
- ↑ Ruisinger JF, Backes JM, Gibson CA, Moriarty PM (2009). "Once-a-week rosuvastatin (2.5 to 20 mg) in patients with a previous statin intolerance". Am J Cardiol. 103 (3): 393–4. doi:10.1016/j.amjcard.2008.09.095. PMID 19166695.
- ↑ Athyros VG, Tziomalos K, Kakafika AI, Koumaras H, Karagiannis A, Mikhailidis DP (2008). "Effectiveness of ezetimibe alone or in combination with twice a week Atorvastatin (10 mg) for statin intolerant high-risk patients". Am J Cardiol. 101 (4): 483–5. doi:10.1016/j.amjcard.2007.09.096. PMID 18312762.
- ↑ Rivers SM, Kane MP, Busch RS, Bakst G, Hamilton RA (2007). "Colesevelam hydrochloride-ezetimibe combination lipid-lowering therapy in patients with diabetes or metabolic syndrome and a history of statin intolerance". Endocr Pract. 13 (1): 11–6. doi:10.4158/EP.13.1.11. PMID 17360295.
- ↑ Lu Z, Kou W, Du B, et al.: Effect of Xuezhikang, an extract from red yeast Chinese rice, on coronary events in a Chinese population with previous myocardial infarction. Am J Cardiol 2008, 101:1689–1693.
- ↑ Jacobson TA: Toward “pain-free” statin prescribing: clinical algorithm for diagnosis and management of myalgia [see comment]. Mayo Clin Proc 2008, 83:687–700.
- ↑ Calvo MS, Whiting SJ (2003). "Prevalence of vitamin D insufficiency in Canada and the United States: importance to health status and efficacy of current food fortification and dietary supplement use". Nutr Rev. 61 (3): 107–13. PMID 12723644.
- ↑ Baker, S.K. & Tarnopolsky, M.A. (2001). Statin myopathies: pathophysiologic and clinical perspectives. Clin. Invest. Med., 24(5): 258-272.
- ↑ Schaars CF, Stalenhoef AF (2008). "Effects of ubiquinone (coenzyme Q10) on myopathy in statin users". Curr Opin Lipidol. 19 (6): 553–7. doi:10.1097/MOL.0b013e3283168ecd. PMID 18957876.
- ↑ Levy HB, Kohlhaas HK (2006). "Considerations for supplementing with coenzyme Q10 during statin therapy". Ann Pharmacother. 40 (2): 290–4. doi:10.1345/aph.1G409. PMID 16449543.