Pyloric stenosis surgery
|
Pyloric stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pyloric stenosis surgery On the Web |
|
American Roentgen Ray Society Images of Pyloric stenosis surgery |
|
Risk calculators and risk factors for Pyloric stenosis surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Mohamadmostafa Jahansouz M.D.[2]
Overview
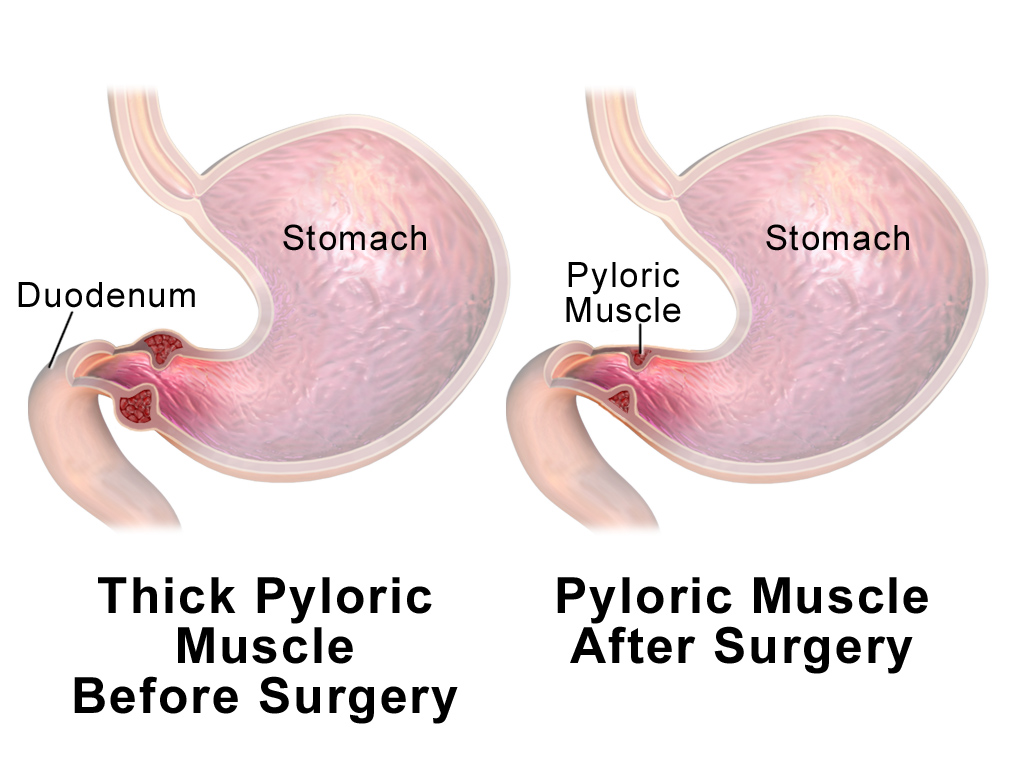
Infantile pyloric stenosis is typically managed with surgery. Ranstedt's extramuscular pyloromyotomy is the gold standard of treatment. After the surgery, once the stomach can empty into the duodenum, feeding can be started. There is occasionally recurrence in the immediate post-operative period, but the condition generally has no long-term impact on the child's future.
Indications
Surgery is the mainstay of treatment for infantile pyloric stenosis.[1]
Surgery
- Definitive treatment for infantile pyloric stenosis is with surgical pyloromyotomy.[2][3]
- This is a relatively straightforward surgery that can be done through a single larger incision or laparoscopically (through several tiny incision*s), depending on the surgeon's experience and preference.
- Ranstedt's extramuscular pyloromyotomy is the gold standard of treatment.[4]
- After the surgery, once the stomach can empty into the duodenum, feeding can be started.
- There is occasionally recurrence in the immediate post-operative period, but the condition generally has no long-term impact on the child's future.
| hvfye6nokpQ|500}} |
References
- ↑ Sparrow, Charles A. (1921). "Congenital Hypertrophic Pyloric Stenosis". The Boston Medical and Surgical Journal. 185 (8): 235–238. doi:10.1056/NEJM192108251850805. ISSN 0096-6762.
- ↑ Greason KL, Thompson WR, Downey EC, Lo Sasso B (1995). "Laparoscopic pyloromyotomy for infantile hypertrophic pyloric stenosis: report of 11 cases". J Pediatr Surg. 30 (11): 1571–4. PMID 8583327.
- ↑ Levine D, Edwards DK (1992). "The olive on end: a useful variant of the "shoulder" sign in the barium X-ray diagnosis of idiopathic hypertrophic pyloric stenosis". Pediatr Radiol. 22 (4): 275–6. PMID 1523050.
- ↑ Chalya PL, Manyama M, Kayange NM, Mabula JB, Massenga A (2015). "Infantile hypertrophic pyloric stenosis at a tertiary care hospital in Tanzania: a surgical experience with 102 patients over a 5-year period". BMC Res Notes. 8: 690. doi:10.1186/s13104-015-1660-4. PMC 4652415. PMID 26581339.