Proximal humerus fracture

| Proximal humerus fracture | |
| ICD-10 | S42.2-S42.4 |
|---|---|
| ICD-9 | 812 |
| eMedicine | emerg/199 orthoped/271 orthoped/199 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
Overview[1][2]
The injuries of the ball-and-socket shoulder joint considered as the Proximal humerus fracture. It is more common among the elderly population following a low energy trauma such as falling. Meanwhile, A few people experience the axillary nerve damage such as reduced sensation around the middle deltoid and/or axillary artery involvement.
Historical Perspective
There are no reliable information regarding the historical perspective of the Proximal humerus fracture.
Causes[3][4][5]
The main etiology of the Proximal humerus fracture is thought to be an axial loading may be placed on a hyperpronated forearm during falling onto an outstretched hand (FOOSH) with an extended wrist and hyperpronated forearm and shoulder. Because at this posture the energy from the radius fracture transmitted towards the shoulder joint cause the fracture and/or dislocation of the humerus bone. As a person age, two factors cause higher risk of fractures:
- Weaker bones
- Greater risk of falling
Stress fractures as a common causes of fractures can be found due to the repeated stresses and strains. Importantly children having more physically active lifestyles than adults, are also prone to fractures. People with any underlying diseases such as osteoporosis, infection, or a tumor affecting their bones having a higher risk of fractures. As mentioned in previous chapters, this type of fracture is known as a pathological fracture. Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures.
Life-threatening Causes
- There are no life-threatening causes of Proximal humerus fracture , however complications resulting from Proximal humerus fracture is common.
Common Causes
Common causes of Proximal humerus fracture may include:
- Trauma (Fall on an outstretched hand)
Less Common Causes
Less common causes of Proximal humerus fracture include conditions that predisposes to fracture:
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | Osteoporosis and osteopenia. |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | Osteoporosis and osteopenia. |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | Falling of car accident to on side of humerus bone. |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
List the causes of the disease in alphabetical order:
Pathophysiology [6][7][8][9][10][11][3][12][13]
Mechanism
The Proximal humerus fracture is caused by a falling. The form and severity of this fracture depends on the position of the shoulder joint at the moment of hitting the ground. The width of this mentioned angle affects the localization of the fracture. Pronation, supination and abduction positions leads the direction of the force and the compression of carpus and different appearances of injury.
Pathophysiology
Its known that the Proximal humerus fracture in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture.
- The pattern of bone fracture and severity of injury depends on variety of factors such as:
- Patients age
- Patients Weight
- Patients past medical history specifically any bone diseases affecting the quality of bone (such as osteoporosis, malignancies)
- Energy of trauma
- Bone quality
- Position of the specific organ during the trauma
- The below-mentioned processes cause decreased bone mass density:
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Differentiating Proximal humerus fracture from other Diseases[14][15]
In the orthopedic medicine its important to know that the forearm fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. Other injuries such as possible shoulder fracture-dislocation; radial head or coronoid fractures or lateral collateral ligament injury. If the mechanism of injury suggests particularly low energy then the Osteoporosis should be considered. The pathological Fractures occurring in a bone with a tumor or Paget's disease) are rare but possible[3].
Also it should be noted that the both bone fractures can be complicated by acute compartment syndrome of the forearm. Signs suggesting compartment syndrome are pain on extension of digits, and marked edema[3].
As another important fact in orthopedic fracture is if both-bone fractures were found in pediatric which is common after accidental trauma, but it may also be the due to the of child abuse; and in these cases a careful attention and evaluation should be considered if a child abuse is suspected Differential Diagnoses for the Proximal humerus fracture:
- Shoulder Dislocation
- Elbow Fracture
- Clavicle Fracture
- Scapular Fracture
Epidemiology and Demographics[16][17]
The proximal humerus fractures account for 5% of all fractures in the Western countries. The proximal humerus fractures is the most common type of the humerus bonefracture , as well as the most common fracture at the shoulder girdle. After the distal radius fracture and vertebra fracture, the Proximal humerus fractures is the third most common osteoporotic fracture. Comparing to epidemiological data of the Japan and European countries, the incidence rates of humerus fractures are higher in the United states population.
Risk Factors [18][19][20]
There are different risk factors that presidpose patient for the Proximal humerus fracture that include:
- High-risk contact sports
- Higher age (elderly adults are higher prone to such fractures)
- Reduced bone density (osteoporosis)
- Direct blow
- Road / traffic accidents
- Falling on an outstretched hand with the forearm pronated
- Direct trauma to the arm/forearm
- Taking part in any rough or high-impact sport
- Street fights, gunshot wounds, and domestic violence, may also cause the Humerus fracture
- Road traffic accidents.
Classification [21][22][23]
| AO classification of proximal humerus fractures: | |
|---|---|
| type A: extra-articular unifocal (either tuberosity +/- surgical neck of the humerus) |
|
| type B: extra-articular bifocal (both tuberosities +/- surgical neck of the humerus or glenohumerus dislocation) |
|
| type C: extra-articular (anatomical neck) but compromise the vascular supply of the articular segment |
|
Neer classification of proximal humerus fractures consisted of :
- Number of fractured parts of the humerus bone:
- humerus head
- greater tuberosity
- lesser tuberosity
- humerus shaft
- Displacement fractured parts of the humerus bone:
- Displacement is on a per-part basis. A fracture part is considered displaced if angulation exceeds 45 degrees, or if the fracture is displaced by more than 1cm
| Neer classification of proximal humerus fractures | ||
|---|---|---|
One-part fracture70-80% |
|
|
Two-part fracture20% |
|
|
Three-part fracture5% |
|
|
Four-part fracture<1% |
|
Patients has non-operative poor outcome
the articular surface is no longer attached to any parts of the humerus it has a high incidence of osteonecrosis |
Screening[24]
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and postmenopausal and women.
Based on the US Preventive Services Task Force (USPSTF) there are three groups of patients need to be screened for the osteoporosis:
- · Men with no history of osteoporosis
- · Women with the age of 65≤ year old, with no previous history of pathological fracture due to the osteoporosis
- · Women with the age of <65 years, with 10-year fracture risk of not less than a 65-year-old white woman (who has not any other risk factor)
Accordingly women older than age of 50 are the main target for the osteoporosis screening. There is no specific recommendation to screen men for the osteoporosis.
The USPSTF recommendations from 2002 included:
Meanwhile, there are two major modalities for the osteoporosis screening:
- · Dual energy x-ray absorptiometry (DXA) of the hip and lumbar spine bones
- · Quantitative ultrasonography of the calcaneus
*It should be noted of the two above mentioned modalities for screening the ultrasonograhy is preferred to the DXA due to its lower cost, lower ionizing radiation, more availability.
After the primary evaluation of the osteoporosis, the further evaluation are required in some cases such as:
· Women with normal bone density or mild osteopenia: T-score of greater than −1.50 – should have screening for 15 years.
· Women with moderate osteopenia: T-score of −1.50 to −1.99 – should have screening for 5 years.
· Women with advanced osteopenia: T-score of −2.00 to −2.49 - should have screening for 1 year.
Natural History, Complications and Prognosis
Natural History [25]
In cases with untreated Proximal humerus fracture the malunion and deformity of arm can be occurred.
Complications [26]
The overall complication rate in the treatment of Humerus fracture were found in around 40% of cases:
- Neurovascular compromise: such as Ulna nerve damage
- Compartment syndrome
- Chronic disability of the DRUJ
- Physeal Injury
- Malunion of the radius
- Nonunion
- Infection
- Refracture following plate removal
- Posterior interosseois nerve (PIN) injury.
- Instability of the DRUJ
Prognosis [27][25]
Successful treatment of Proximal humerus fracture depends on the on-time interventions such as: reduction of the radius and DRUJ and the restoration of the forearm axis. The incidence of nonunion of Humerus fracture is very low. On the other hand, the rate of successful union following the open reduction of forearm fractures was reported around 98%. Previous researches showed that the loss of strength at the supination and pronation were found in 12.5% and 27.2%, respectively.
Diagnosis[28][29]
The diagnosis of a Proximal humerus fracture should be confirmed using a radiographic examination.
History and Symptoms[30][31][32]
The related signs and symptoms include:
- Deformity
- Skin lacerations
- Weak pulse
- Open fractures
- Bruising
- Swelling
- Stiffness
- Inability to move
- Pain in touch
- Loss of function of the forearm
- Difficulties in detection of pulses
- Radial nerve damage
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site (distal-third radial fracture site and at the wrist joint). This injury should be confirmed using a radiographic evaluations. Also, patients may loss the pinch mechanism between their thumb and their index finger which can be due to the paralysis of the flexor pollicis longus (FPL) and flexor digitorum profundus (FDP).
Physical Examination[33][34][35][36][37][38]
The related signs and symptoms include:
- Edema of the shoulder
- Most of the time the edema will be a non-pitting edema
- Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of shoulder
- Bruising
- As a manifestation of internal injury to the local vessels by trauma or fractures bone
- Decrease in range of motion
- Movement of the fractures limb will be painful if possible at all
- Tenderness
- Deformity
- Fractured bone deformity may be touchable in the internal side of the forearm if the fracture is displaced
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the forearm. In polytrauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored.
Physical examination of patients with Proximal humerus fracture is usually remarkable for swelling, tenderness, bruises, ecchymosis, deformity and restricted range of motion of the wrist.
Appearance of the Patient [39]
- Patients with Proximal humerus fracture usually appears normal unless the patients had a high energy trauma causing the open wound fracture.
Vital Signs
- Weak pulse may be seen when associated with polytrauma.
- Low blood pressure with normal pulse pressure may be present due to compound fracture with blood loss.
Skin
- Skin examination of patients with Proximal humerus fracture includes:
HEENT
- HEENT examination of patients with Proximal humerus fracture usually normal.
Neck
- Neck examination of patients with Proximal humerus fracture is usually normal
Lungs
- Pulmonary examination of patients with Proximal humerus fracture usually normal
Heart
- Cardiovascular examination of patients with Proximal humerus fracture usually normal
Abdomen
- Abdominal examination of patients with Proximal humerus fracture usually normal
Back
- Back examination of patients with Proximal humerus fracture usually normal
Genitourinary
- Genitourinary examination of patients with Proximal humerus fracture usually normal
Neuromuscular
- Neuromuscular examination of patients with Proximal humerus fracture is usually normal
- However, some patients may develop neuropraxia of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger.
Laboratory Findings [40]
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the Proximal humerus fracture. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis.
Laboratory tests for the diagnosis of osteoporosis are:
- Complete blood count (CBC)
- Serum total calcium level
- Serum Ionized calcium level
- Serum phosphate level
- Serum alkaline phosphatase level
- Serum 25-(OH)-vitamin D level
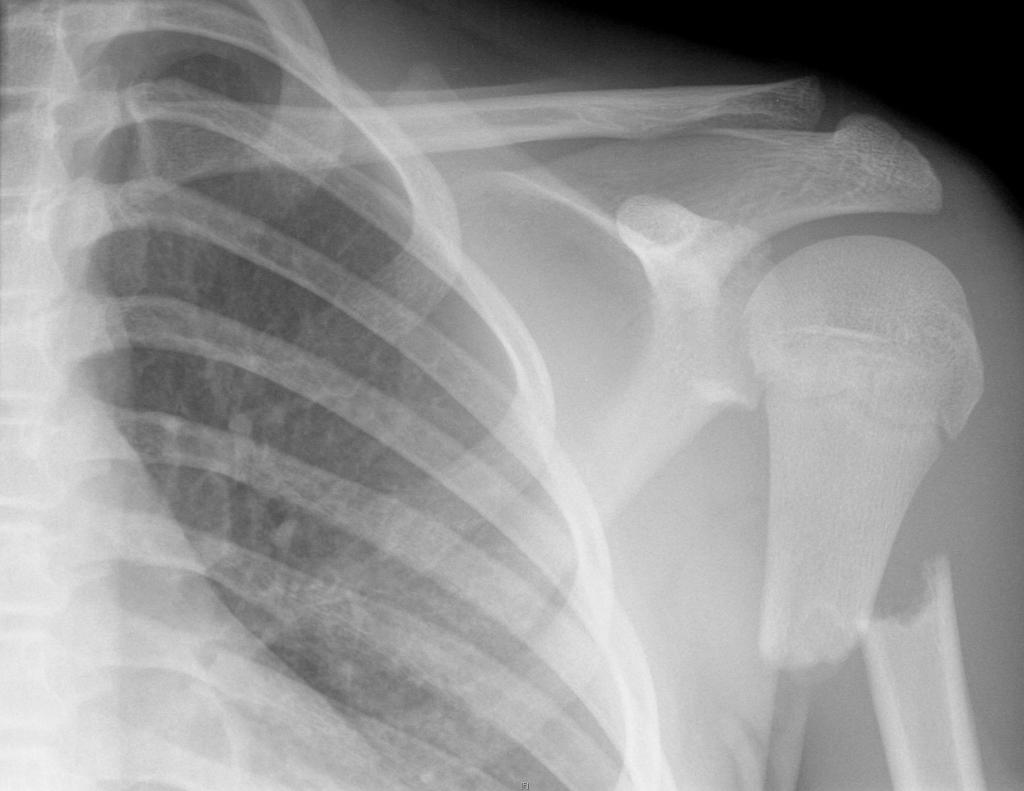
X Ray [41][42]
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the forearm. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the elbow and wrist joint in the radiographs of Humerus fracture to ensure that the distal radioulnar joint injuries are not missed.
CT [43][44][45][46][42]
- CT-scan in the case of the Humerus fractureis the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made.
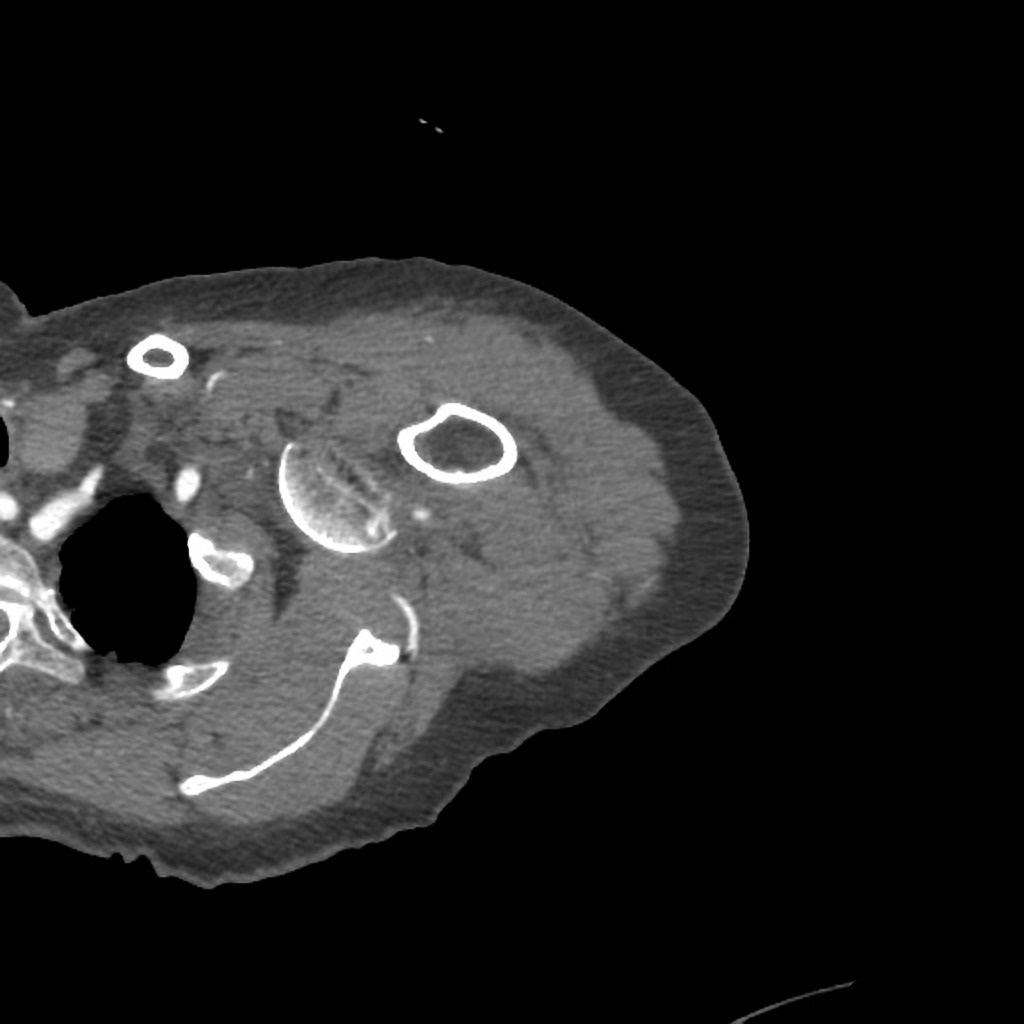
-
Axial bone window- Complex, heavily comminuted proximal humerus fracture-dislocation. Off-ended surgical neck of humerus fracture with complete anterior displacement of the humerus head, which is dislocated from the glenoid anteriorly. Avulsion fracture of the greater tuberosity. Glenohumerus lipohemarthrosis. Surrounding fat stranding.
-
Axial C+ arterial phase- Complex, heavily comminuted proximal humerus fracture-dislocation. Off-ended surgical neck of humerus fracture with complete anterior displacement of the humerushead, which is dislocated from the glenoid anteriorly. Avulsion fracture of the greater tuberosity. Glenohumerus lipohemarthrosis. Surrounding fat stranding.
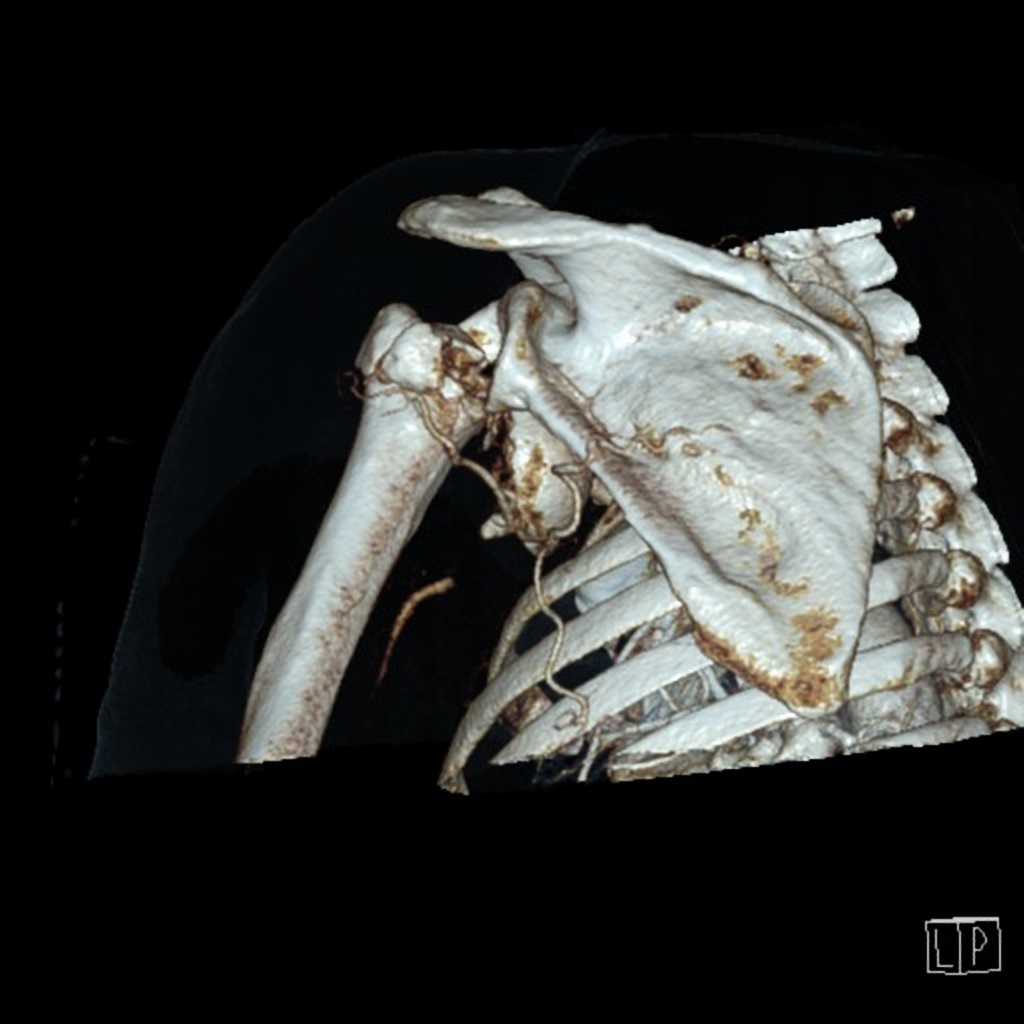
-
3D VRT- Complex, heavily comminuted proximal humerus fracture-dislocation. Off-ended surgical neck of humerus fracture with complete anterior displacement of the humerus head, which is dislocated from the glenoid anteriorly. Avulsion fracture of the greater tuberosity. Glenohumerus lipohemarthrosis. Surrounding fat stranding.
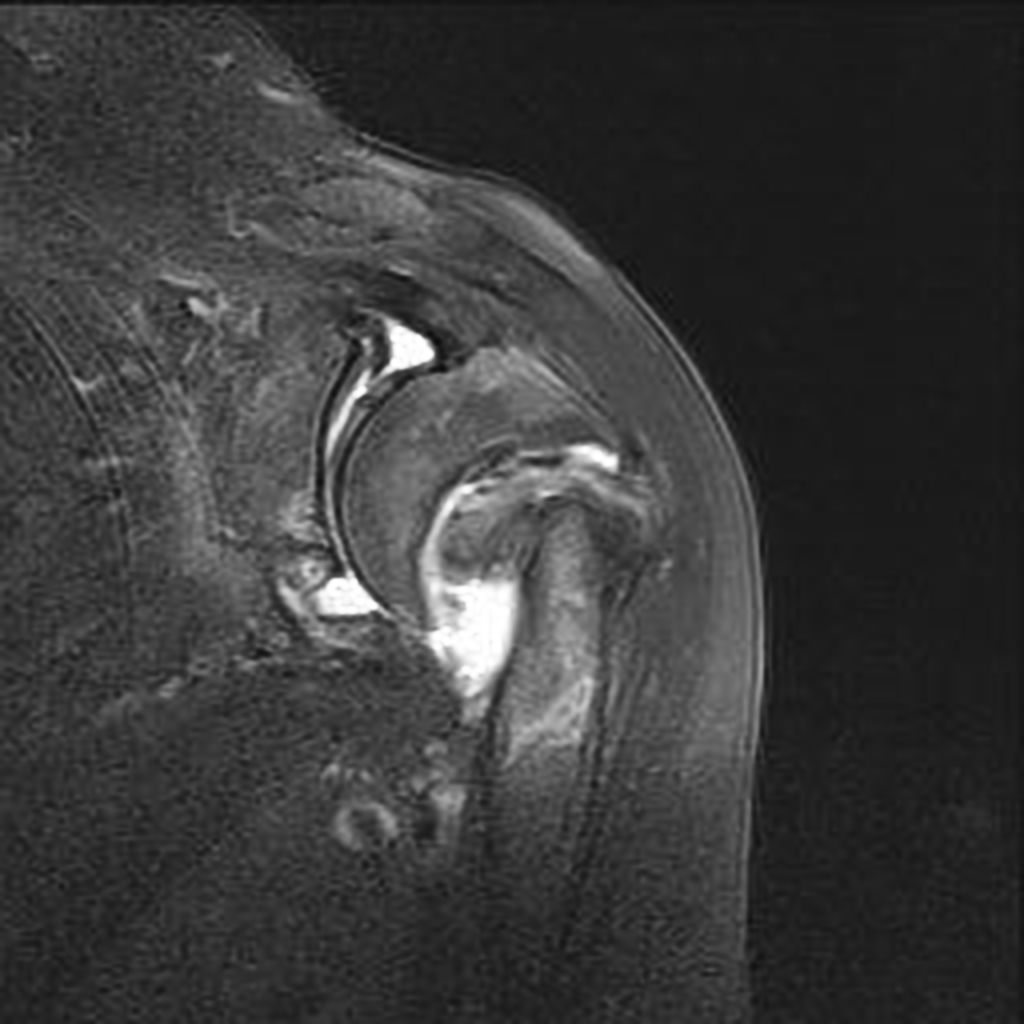
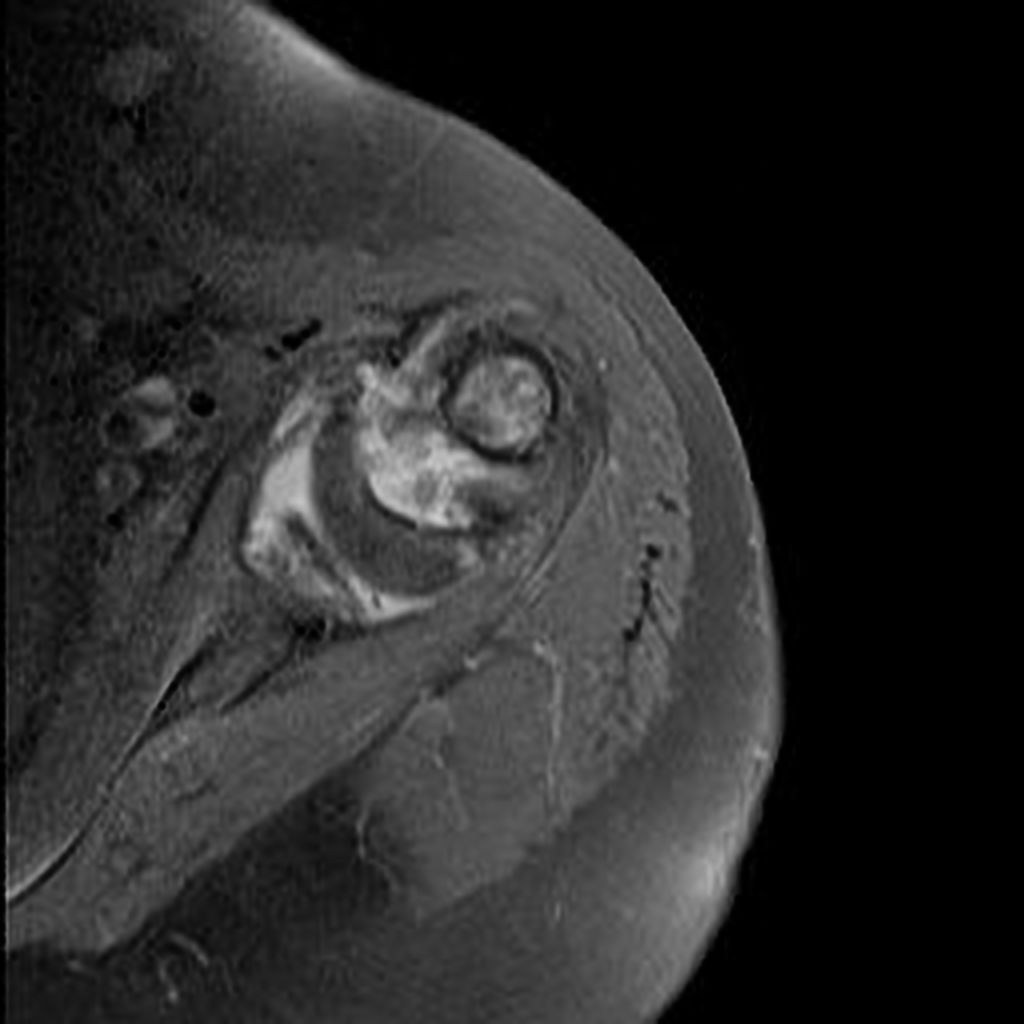
MRI [47][48][42]
- Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely.
- MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the Proximal humeral fracture, but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated forearm fractures.
- Meanwhile, the MRI can be useful in in following mentioned evaluations:
- Evaluation of occult fractures
- Evaluation of the post-traumatic or avascular necrosis of carpal bones
- Evaluation of tendons
- Evaluation of nerve
- Evaluation of carpal tunnel syndrome
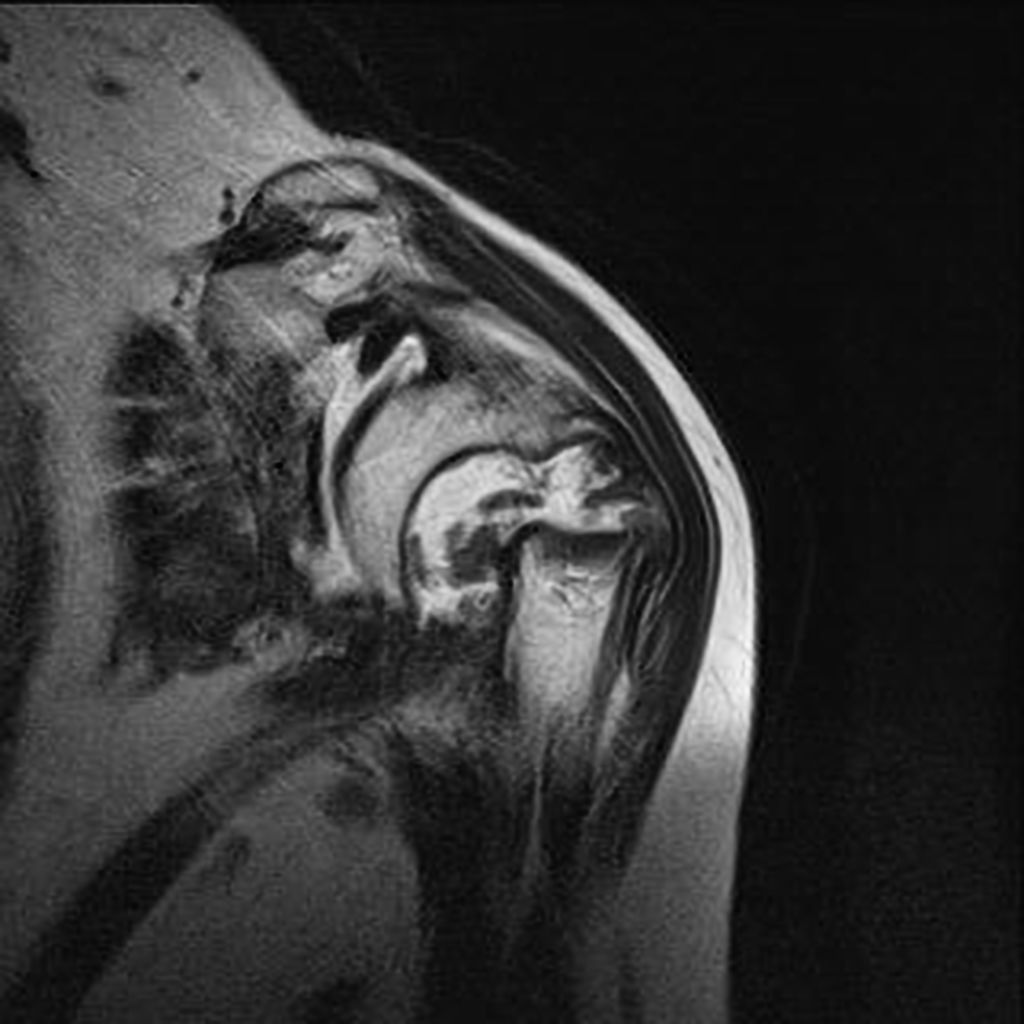
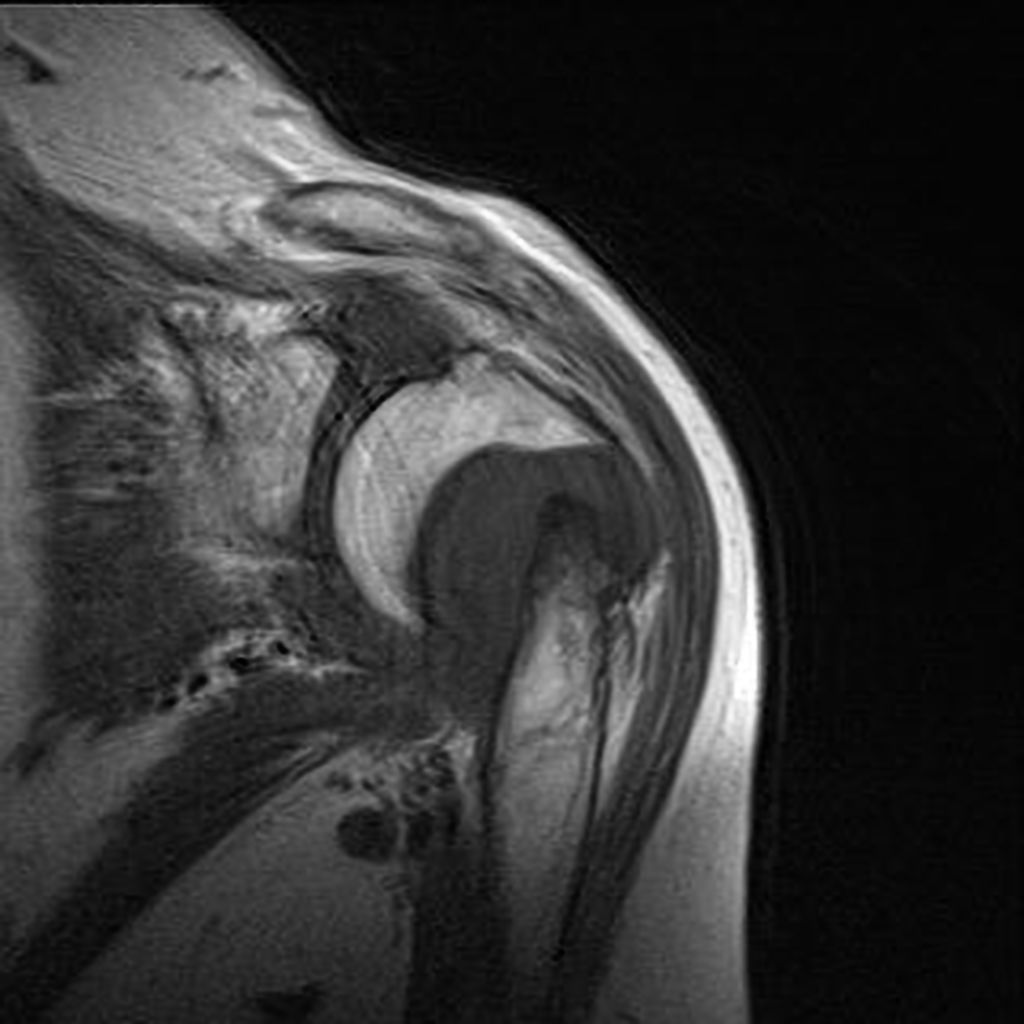
-
Coronal T2- Complete fracture of the anatomical neck of the humerus head with displaced bone fragments, and rotation and bone resorption. Presence of fluid between the bone fragments, with joint effusion and significant synovial thickening (synovitis).
-
Coronal T1- Complete fracture of the anatomical neck of the humerus head with displaced bone fragments, and rotation and bone resorption. Presence of fluid between the bone fragments, with joint effusion and significant synovial thickening (synovitis).
-
Coronal STIR- Complete fracture of the anatomical neck of the humerus head with displaced bone fragments, and rotation and bone resorption. Presence of fluid between the bone fragments, with joint effusion and significant synovial thickening (synovitis).
-
Axial STIR-Complete fracture of the anatomical neck of the humerus head with displaced bone fragments, and rotation and bone resorption. Presence of fluid between the bone fragments, with joint effusion and significant synovial thickening (synovitis).
Other Imaging Findings[49]
There are no other imaging findings associated with Proximal humerus fracture
Other Diagnostic Studies[49]
There are no other Diagnostic studies associated with Proximal humerus fracture
Treatment [50][48][26][51]
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open forearm fractures considered as a surgical emergency. Humerus fracture occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the Humerus fracture. There are controversies regarding the indications for intramedullary nailing of forearm fractures.
Non-Operative Treatmen [51]
- The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe.
- In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of both bones of the forearm. If the fracture shifts in position, it may require surgery to put the bones back together.
- Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the Humerus fracture
- For all patients with Humerus fracture, a post-reduction true lateral radiograph is suggested .
- Operative fixation is suggested in preference to cast fixation for fractures with post-reduction radial shortening greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm.
- Patients probably do not need to begin early wrist motion routinely after stable fracture fixation.
- Adjuvant treatment of Humerus fracture with vitamin C is suggested for the prevention of disproportionate pain
Complications of Non-surgical therapy
Failure of non-surgical therapy is common:
- Re-displacement to its original position even in a cast
- Stiffness
- Post traumatic osteoarthritis leading to wrist pain and loss of function
- Other risks specific to cast treatment include:
- Compression of the swollen arm causing compartment syndrome
- Reflex sympathetic dystrophy is a serious complication
- Stiffness is universal following a prolonged period of immobilization and swelling
Surgery [52][53][54][27][51][55][1][42]
Returning to the normal physical activity after Humerus fracturecan take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult Humerus fracture should be considered to be treated with open reduction and internal fixation (ORIF).
-
Plate and screw ORIF performed.
-
Plate and screw ORIF performed.
-
Treated with open reduction and pinning.
-
Treated with open reduction and pinning.
Operation
- There are a variety of methods and implants useful to stabilize the Humerus fracture, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex Humerus fracture include external fixation, and open reduction and internal fixation.
External Fixation With or Without Percutaneous Pin Fixation
- Wrist spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation of ulnar bone.
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the superficial branch of the nerve
- Complex regional pain syndrome
Open reduction and internal fixation with plates and screws
- This is the most common type of surgical repair for Humerus fracture
- During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment.
- The bones held together with special screws and metal plates attached to the outer surface of the bone.
Complications of open reduction and internal fixation with plates and screws =
- Infection
- Damage to nerves and blood vessels
- Synostosis
- Nonunion
Pain Management
Pain after an injury or surgery is a natural part of the healing process.
Medications are often prescribed for short-term pain relief after surgery or an injurysuch as:
- opioids
- non-steroidal anti-inflammatory drugs (NSAIDs)
- local anesthetics
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor.
Interventions [48]
The following options can be helpful for patients to rehabilitate after their fracture :
- Joints mobilization
- compression bandage
- Soft tissue massage
- Exercises and Activity modification
- Forearm taping
- Forearm bracing
Postoperative Rehabilitation [56]
- Complex Humerus fracture warrant individualized immobilization and rehabilitation strategies.
- Similarly, the addition of a thumb spica cast or orthosis with positioning of the wrist in slight ulnar deviation for management of a comminuted radial column fracture may prevent loss of reduction. *Because most multifragmentary Humerus fracture are the result of high-energy injuries, a prolonged period of wrist immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The wrist is typically immobilized for 2 weeks post-operatively in a sugar tong splint with neutral forearm rotation.
- At 6 weeks post-operatively, the wrist is placed into a removable orthosis, and active and passive range of motion (ROM) is initiated.
- Full weight bearing commences at approximately 3 months post-operatively after consolidation of the fracture is noted on radiographs.
- The presence of varying degrees of hand, wrist, and elbow stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral upper extremity fractures, or peripheral nerve injuries.
- Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness.
- Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the hand.
- A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the hand and limit the development of intrinsic muscle tightness
Primary Prevention[57]
There are various preventive options to reduce the incidence of the Humerus fracture
- Using forearm and wrist guards during practicing sports (skating, biking)
- Using forearm and wrist guards during driving motorbikes
- Avoid falls in elderly individuals
- Prevention and/or treatment of osteoporosis
- Healthy diet
Secondary Prevention[57]
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of osteoporosis consequently these type of patients at greater risk for the pathological fractures .
So the Calcium and vitamin D supplementation play important role in increasing the bone mineral density (BMD) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive alcohol and quitting smoking play important role in this regard.
Detecting osteoporosis[24][58]
- DEXA(dual-energy x-ray absorptiometry) scan
- Serum calcium and vitamin D levels
- Ultrasonography of the calcaneus
Pharmacological therapy [58]
- The primary goal for the treatment of osteoporosis is to reduce longtime fracture risk in patients. Increasing bone mineral density (BMD) in response to the treatment is far less important than improvement of clinical aspects of osteoporosis, i.e., osteoporoticfracture. Therefore, most of the drugs efficacy is measured by the extent they improve the fracture risk instead of increasing BMD.
- During the treatment, if a single fracture happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a specialist.
- Calcium and vitamin D supplementation have been found to be effective in reducing the long term fracture risk, significantly. In order to suggest the people to use vitamin D and calcium supplements, the physician needs to make sure that patient is not able to obtain the nutrients through the daily intake. The available supplemental ions of calcium include calcium carbonate, calcium citrate, and vitamin D3 in various dosage forms.
Life style modifications[58][57]
- Exercise: Exercise promotes the mineralization of bone and bone accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of osteoporosis. However, it can have a negative effect on bone mineralization in cases of poor nutrition, such as anorexia nervosa and celiac disease.
- Nutrition: A diet high in calcium and vitamin D prevents bone loss. Patients at risk for osteoporosis, such as persons with chronic steroid use are generally treated with vitamin D and calcium supplementation. In renal disease, more active forms of vitamin D, such as 1,25-dihydroxycholecalciferol or calcitriol are used; as the kidney cannot adequately generate calcitriol from calcidiol (25-hydroxycholecalciferol), which is the storage form of vitamin D.
- By quitting smoking, osteoporosis as well as other diseases can be prevented.
- Avoiding excessive alcohol intake or drinking only in moderation.
Template:Fractures Template:WH Template:WS
See also
- AO classification of proximal humerus fracture
- Neer classification
- Distal humerus fracture
- Humeral_shaft_fracture
- Humerus fracture
References
- ↑ 1.0 1.1 Stone MA, Namdari S (April 2019). "Surgical Considerations in the Treatment of Osteoporotic Proximal Humerus Fractures". Orthop. Clin. North Am. 50 (2): 223–231. doi:10.1016/j.ocl.2018.10.005. PMID 30850080.
- ↑ Lin KM, James EW, Spitzer E, Fabricant PD (February 2018). "Pediatric and adolescent anterior shoulder instability: clinical management of first-time dislocators". Curr. Opin. Pediatr. 30 (1): 49–56. doi:10.1097/MOP.0000000000000566. PMID 29135565.
- ↑ 3.0 3.1 Monica J, Vredenburgh Z, Korsh J, Gatt C (July 2016). "Acute Shoulder Injuries in Adults". Am Fam Physician. 94 (2): 119–27. PMID 27419328.
- ↑ Rothberg D, Higgins T (January 2013). "Fractures of the proximal humerus". Orthop. Clin. North Am. 44 (1): 9–19. doi:10.1016/j.ocl.2012.08.004. PMID 23174322.
- ↑ Price MC, Horn PL, Latshaw JC (2013). "Proximal humerus fractures". Orthop Nurs. 32 (5): 251–8, quiz 259–60. doi:10.1097/NOR.0b013e3182a39b20. PMID 24022417.
- ↑ Bandovic I, Futterman B. PMID 30020631. Missing or empty
|title=(help) - ↑ Geßmann J, Königshausen M, Schildhauer TA, Seybold D (April 2019). "[Periprosthetic humeral fractures: from osteosynthesis to prosthetic replacement]". Oper Orthop Traumatol (in German). 31 (2): 84–97. doi:10.1007/s00064-019-0591-y. PMID 30820585.
- ↑ Torchia MT, Austin DC, Cozzolino N, Jacobowitz L, Bell JE (April 2019). "Acute versus delayed reverse total shoulder arthroplasty for the treatment of proximal humeral fractures in the elderly population: a systematic review and meta-analysis". J Shoulder Elbow Surg. 28 (4): 765–773. doi:10.1016/j.jse.2018.10.004. PMID 30658889.
- ↑ Xie L, Ding F, Zhao Z, Chen Y, Xing D (2015). "Operative versus non-operative treatment in complex proximal humeral fractures: a meta-analysis of randomized controlled trials". Springerplus. 4: 728. doi:10.1186/s40064-015-1522-5. PMC 4659794. PMID 26636016.
- ↑ Teunis T, Nota SP, Hornicek FJ, Schwab JH, Lozano-Calderón SA (July 2014). "Outcome after reconstruction of the proximal humerus for tumor resection: a systematic review". Clin. Orthop. Relat. Res. 472 (7): 2245–53. doi:10.1007/s11999-014-3474-4. PMC 4048415. PMID 24469551.
- ↑ Ji JH, Moon CY, Kim YY, Shafi M (December 2009). "Arthroscopic fixation for a malunited greater tuberosity fracture using the suture-bridge technique: technical report and literature review". Knee Surg Sports Traumatol Arthrosc. 17 (12): 1473–6. doi:10.1007/s00167-009-0797-x. PMID 19399480.
- ↑ Duparc F, Merlet MC (February 2019). "Prevention and management of early treatment failures in elbow injuries". Orthop Traumatol Surg Res. 105 (1S): S75–S87. doi:10.1016/j.otsr.2018.05.016. PMID 30591417.
- ↑ Regel G, Seekamp A, Blauth M, Klemme R, Kuhn K, Tscherne H (February 1996). "[Complex injury of the elbow joint]". Unfallchirurg (in German). 99 (2): 92–99. PMID 8881223.
- ↑ Wülker N (October 2001). "[100 years shoulder and elbow surgery]". Orthopade (in German). 30 (10): 789–97. PMID 11681098.
- ↑ Park DY, Cho JH, Lee DH, Choi WS, Bang JY, Yin XY (October 2017). "A 3-Dimensional Analysis of the Fracture Planes in Pediatric Lateral Humeral Condyle Fractures for Image-Based Pin Positioning During Fixation". J Orthop Trauma. 31 (10): e340–e346. doi:10.1097/BOT.0000000000000914. PMID 28538289.
- ↑ Tsuda T (November 2017). "Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature". Curr Orthop Pract. 28 (6): 580–585. doi:10.1097/BCO.0000000000000563. PMID 29177024.
- ↑ Sabesan VJ, Lombardo D, Petersen-Fitts G, Weisman M, Ramthun K, Whaley J (December 2017). "National trends in proximal humerus fracture treatment patterns". Aging Clin Exp Res. 29 (6): 1277–1283. doi:10.1007/s40520-016-0695-2. PMID 28124187.
- ↑ Moayeri A, Mohamadpour M, Mousavi SF, Shirzadpour E, Mohamadpour S, Amraei M (2017). "Fracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysis". Ther Clin Risk Manag. 13: 455–468. doi:10.2147/TCRM.S131945. PMC 5395277. PMID 28442913.
- ↑ Gradl G, Pape HC, Tingart M, Arbab D (April 2014). "[Fractures of the proximal humerus in the elderly : Osteosynthesis versus joint replacement]". Orthopade (in German). 43 (4): 339–46. doi:10.1007/s00132-013-2161-6. PMID 24671346.
- ↑ Lefèvre Y, Journeau P, Angelliaume A, Bouty A, Dobremez E (February 2014). "Proximal humerus fractures in children and adolescents". Orthop Traumatol Surg Res. 100 (1 Suppl): S149–56. doi:10.1016/j.otsr.2013.06.010. PMID 24394917.
- ↑ Wennergren D, Stjernström S, Möller M, Sundfeldt M, Ekholm C (June 2017). "Validity of humerus fracture classification in the Swedish fracture register". BMC Musculoskelet Disord. 18 (1): 251. doi:10.1186/s12891-017-1612-3. PMC 5466790. PMID 28601085.
- ↑ Ploeger MM, Pennekamp PH, Müller MC, Kabir K, Burger C, Wirtz DC, Schmolders J (December 2015). "[Bilateral Dislocation Fracture of the Humeral Head (Right AO 11C3.3; Left AO 11A1.3) without Direct Trauma Due to First Clinical Manifestation of Seizure - a Case Report and Review of the Literature]". Z Orthop Unfall (in German). 153 (6): 643–7. doi:10.1055/s-0035-1546265. PMID 26468921.
- ↑ Du S, Ye J, Chen H, Li X, Lin Q (December 2017). "Interventions for Treating 3- or 4-part proximal humeral fractures in elderly patient: A network meta-analysis of randomized controlled trials". Int J Surg. 48: 240–246. doi:10.1016/j.ijsu.2017.09.002. PMID 28890408.
- ↑ 24.0 24.1 Lill H, Ellwein A, Katthagen C, Voigt C (October 2012). "[Osteoporotic fractures of the proximal humerus]". Chirurg (in German). 83 (10): 858–65. doi:10.1007/s00104-012-2337-3. PMID 23051983.
- ↑ 25.0 25.1 Launonen AP, Lepola V, Flinkkilä T, Laitinen M, Paavola M, Malmivaara A (June 2015). "Treatment of proximal humerus fractures in the elderly: a systemic review of 409 patients". Acta Orthop. 86 (3): 280–5. doi:10.3109/17453674.2014.999299. PMC 4443467. PMID 25574643.
- ↑ 26.0 26.1 Laux CJ, Grubhofer F, Werner C, Simmen HP, Osterhoff G (September 2017). "Current concepts in locking plate fixation of proximal humerus fractures". J Orthop Surg Res. 12 (1): 137. doi:10.1186/s13018-017-0639-3. PMC 5613450. PMID 28946902. Vancouver style error: initials (help)
- ↑ 27.0 27.1 Petkovic D, Kovacevic D, Levine WN, Jobin CM (January 2019). "Management of the Failed Arthroplasty for Proximal Humerus Fracture". J Am Acad Orthop Surg. 27 (2): 39–49. doi:10.5435/JAAOS-D-17-00051. PMID 30260910.
- ↑ Yamada M, Briot J, Pedrono A, Sans N, Mansat P, Mansat M, Swider P (2007). "Age- and gender-related distribution of bone tissue of osteoporotic humeral head using computed tomography". J Shoulder Elbow Surg. 16 (5): 596–602. doi:10.1016/j.jse.2007.01.006. PMID 17644004.
- ↑ Lill H, Katthagen C, Hertel A, Gille J, Voigt C (May 2012). "All-arthroscopic intramedullary nailing of 2- and 3-part proximal humeral fractures: a new arthroscopic technique and preliminary results". Arch Orthop Trauma Surg. 132 (5): 641–7. doi:10.1007/s00402-011-1430-2. PMID 22101409.
- ↑ Kim TI, Choi JH, Kim SH, Oh JH (September 2016). "The Adequacy of Diagnosis and Treatment for Osteoporosis in Patients with Proximal Humeral Fractures". Clin Orthop Surg. 8 (3): 274–9. doi:10.4055/cios.2016.8.3.274. PMC 4987311. PMID 27583110.
- ↑ Cortes LE, Triana M, Vallejo F, Slongo TF, Streubel PN (July 2011). "Adult proximal humerus locking plate for the treatment of a pediatric subtrochanteric femoral nonunion: a case report". J Orthop Trauma. 25 (7): e63–7. doi:10.1097/BOT.0b013e3181f8d9c3. PMID 21577158.
- ↑ Lill H, Hepp P, Gowin W, Oestmann JW, Korner J, Haas NP, Josten C, Duda GN (December 2002). "[Age- and gender-related distribution of bone mineral density and mechanical properties of the proximal humerus]". Rofo (in German). 174 (12): 1544–50. doi:10.1055/s-2002-35944. PMID 12471527.
- ↑ Resmini G, Iolascon G (August 2007). "79-year-old post-menopausal woman with humerus fracture during teriparatide treatment". Aging Clin Exp Res. 19 (4 Suppl): 30–1. PMID 18182890.
- ↑ Atilla B, Caglar O, Akgun RC (March 2008). "Acute fracture of the acetabulum secondary to a convulsive seizure 3 years after total hip arthroplasty". Orthopedics. 31 (3): 283. PMID 19292226.
- ↑ Zych GA, Montane I (October 1987). "Acute fracture of the proximal humerus superimposed on a chronic posterior dislocation of the humeral head". South. Med. J. 80 (10): 1307–8. PMID 3660047.
- ↑ Wu JW, Shen HL, Liu LM, Gao ZH (August 2016). "[Analysis of early failure of the PHILOS in proximal humerus fractures]". Beijing Da Xue Xue Bao (in Chinese). 48 (4): 683–685. PMID 29263513.
- ↑ Siegel JA, Dines DM (January 2000). "Proximal humerus malunions". Orthop. Clin. North Am. 31 (1): 35–50. PMID 10629331.
- ↑ Iwamoto T, Suzuki T, Matsumura N, Nakamura M, Matsumoto M, Sato K (May 2017). "Lateral Para-Olecranon Approach for the Treatment of Distal Humeral Fracture". J Hand Surg Am. 42 (5): 344–350. doi:10.1016/j.jhsa.2017.02.004. PMID 28359639.
- ↑ Bhat TA, Gulzar A, Bhat AA, Bhat TA, Ali Z (February 2018). "A review of upper limb injuries in bear maul victims: Consistent pattern and inverse relation in severity with facial and scalp injuries". Chin. J. Traumatol. 21 (1): 38–41. doi:10.1016/j.cjtee.2017.11.001. PMID 29402720.
- ↑ Jabran A, Peach C, Ren L (April 2018). "Biomechanical analysis of plate systems for proximal humerus fractures: a systematic literature review". Biomed Eng Online. 17 (1): 47. doi:10.1186/s12938-018-0479-3. PMC 5923007. PMID 29703261.
- ↑ Biber R, Grüninger S, Bail HJ (January 2017). "[Upper extremity fractures in the elderly]". Z Gerontol Geriatr (in German). 50 (1): 73–85. doi:10.1007/s00391-016-1166-2. PMID 28070676.
- ↑ 42.0 42.1 42.2 42.3 Gaetke-Udager K, Yablon CM (April 2019). "Fractures Around the Shoulder: Radiologic Update on Surgical Fixation Techniques". Semin Musculoskelet Radiol. 23 (2): 99–108. doi:10.1055/s-0038-1677465. PMID 30925624.
- ↑ Khanna K, Brabston EW, Qayyum U, Gardner TR, Levine WN, Jobin CM, Ahmad CS (April 2018). "Proximal Humerus Fracture 3-D Modeling". Am J. Orthop. 47 (4). doi:10.12788/ajo.2018.0023. PMID 29719012.
- ↑ Ramappa AJ, Patel V, Goswami K, Zurakowski D, Yablon C, Rodriguez EK, Appleton P, DeAngelis JP (March 2014). "Using computed tomography to assess proximal humerus fractures". Am J. Orthop. 43 (3): E43–7. PMID 24660183.
- ↑ Hasan AP, Phadnis J, Jaarsma RL, Bain GI (October 2017). "Fracture line morphology of complex proximal humeral fractures". J Shoulder Elbow Surg. 26 (10): e300–e308. doi:10.1016/j.jse.2017.05.014. PMID 28689822.
- ↑ Carbone S, Mezzoprete R, Papalia M, Arceri V, Carbone A, Gumina S (March 2018). "Radiographic patterns of osteoporotic proximal humerus fractures". Eur J Radiol. 100: 43–48. doi:10.1016/j.ejrad.2017.12.025. PMID 29496078.
- ↑ Sakoma Y, Hirooka T (December 2017). "Relationship between the Axillary Nerve and Accompanying Vessels and Proximal Humeral Locking Plates in Japanese: An MRI Study". Acta Med. Okayama. 71 (6): 525–529. doi:10.18926/AMO/55590. PMID 29276226.
- ↑ 48.0 48.1 48.2 Kancherla VK, Singh A, Anakwenze OA (January 2017). "Management of Acute Proximal Humeral Fractures". J Am Acad Orthop Surg. 25 (1): 42–52. doi:10.5435/JAAOS-D-15-00240. PMID 28002214.
- ↑ 49.0 49.1 Robinson BC, Athwal GS, Sanchez-Sotelo J, Rispoli DM (October 2008). "Classification and imaging of proximal humerus fractures". Orthop. Clin. North Am. 39 (4): 393–403, v. doi:10.1016/j.ocl.2008.05.002. PMID 18803970.
- ↑ Launonen AP, Sumrein BO, Lepola V (2017). "Treatment of proximal humerus fractures in the elderly". Duodecim. 133 (4): 353–8. PMID 29205983.
- ↑ 51.0 51.1 51.2 Beks RB, Ochen Y, Frima H, Smeeing D, van der Meijden O, Timmers TK, van der Velde D, van Heijl M, Leenen L, Groenwold R, Houwert RM (August 2018). "Operative versus nonoperative treatment of proximal humeral fractures: a systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials". J Shoulder Elbow Surg. 27 (8): 1526–1534. doi:10.1016/j.jse.2018.03.009. PMID 29735376. Vancouver style error: initials (help)
- ↑ Zhao W, Zhang Y, Johansson D, Chen X, Zheng F, Li L (2017). "Comparison of Minimally Invasive Percutaneous Plate Osteosynthesis and Open Reduction Internal Fixation on Proximal Humeral Fracture in Elder Patients: A Systematic Review and Meta-Analysis". Biomed Res Int. 2017: 3431609. doi:10.1155/2017/3431609. PMC 5494086. PMID 28698871.
- ↑ Gracitelli M, Malavolta EA, Assunção JH, Ferreira Neto AA, Silva JS, Hernandez AJ (September 2017). "Locking intramedullary nails versus locking plates for the treatment of proximal humerus fractures". Expert Rev Med Devices. 14 (9): 733–739. doi:10.1080/17434440.2017.1364624. PMID 28792243. Vancouver style error: initials (help)
- ↑ Sobel AD, Shah KN, Paxton ES (August 2017). "Fixation of a Proximal Humerus Fracture With an Intramedullary Nail". J Orthop Trauma. 31 Suppl 3: S47–S49. doi:10.1097/BOT.0000000000000909. PMID 28697089.
- ↑ Vlachopoulos L, Székely G, Gerber C, Fürnstahl P (January 2018). "A scale-space curvature matching algorithm for the reconstruction of complex proximal humeral fractures". Med Image Anal. 43: 142–156. doi:10.1016/j.media.2017.10.006. PMID 29102769.
- ↑ Grobet C, Marks M, Tecklenburg L, Audigé L (July 2018). "Application and measurement properties of EQ-5D to measure quality of life in patients with upper extremity orthopaedic disorders: a systematic literature review". Arch Orthop Trauma Surg. 138 (7): 953–961. doi:10.1007/s00402-018-2933-x. PMID 29654354.
- ↑ 57.0 57.1 57.2 Walsh JS, Vilaca T (May 2017). "Obesity, Type 2 Diabetes and Bone in Adults". Calcif. Tissue Int. 100 (5): 528–535. doi:10.1007/s00223-016-0229-0. PMC 5394147. PMID 28280846.
- ↑ 58.0 58.1 58.2 Kammerlander C, Neuerburg C, Verlaan JJ, Schmoelz W, Miclau T, Larsson S (June 2016). "The use of augmentation techniques in osteoporotic fracture fixation". Injury. 47 Suppl 2: S36–43. doi:10.1016/S0020-1383(16)47007-5. PMID 27338226.