Penile carcinoma in situ
Template:BalanitisV Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Vishal Devarkonda, M.B.B.S[2]
Overview
Balanitis is inflammation of glans penis. When inflammation involves foreskin and perpuce, it is termed as balanoposthitis. Bowenoid papulosis, Erythroplasia of Queyrat, and Bowen's disease are the three common penile carcinoma in situ causing balanitis. The exact pathogenesis for these conditions is not clearly known, but there is a strong association between Human papilloma virus and penile carcinoma in situ. Patients may be asymptomatic or symptomatic presentiing with pruritic, or painful lesions in the genital region. Diagnosis is based on the clinical features supported by biopsy. Transformation into invasive squamous cell carcinoma is the major complication associated with these conditions. Treatment for these conditions include both medical and surgical modalities.
Historical Perspective
Historical perspective of penile carcinoma in situ include:[1]
Bowenoid papulosis
- In 1977, term Bowenoid papulosis was coined by Kopf and Bart and named after dermatologist John templeton Bowen
Erythroplasia of Queyrat
- In 1891, Tarnovsky for the first time described Erythroplasia of Queyrat
- In 1893, Fournier and Darier appreciated it as a penile disease
- in 1933, Sulzberger recognized it as carcinoma in situ
Bowen's disease
- In 1912, Bowen's Disease was described by American dermatologist John T. Bowen
Classification
There is no established classification for Balanitis caused by Penile carcinoma in situ
Pathophysiology
Pathophysiology of penile carcinoma in situ include:[1][2][3] [4][5][6][2][7]
Bowenoid papulosis
The exact pathogenesis of Bowenoid papulosis is unknown.[1]
Some studies have shown, etiological role of HPV type 16, 31, and 39 in Bowenoid papulosis.
Associated conditions include:
- HIV
- Lymphopenia
- Depressed cell-mediated immunity
Histopathology
- The histopathology may reveal squamous cell carcinoma in situ, with widened spinous epidermal layer with proliferation of atypical basal cells, coilocytes, enlarged polimorfic and hyperchromatic nuclei as well as abnormal mitosis and hyperparakeratosis with collection of melanin of various amount seen.[1][2]

Erythroplasia of Queyrat
The exact pathogenesis of erythroplasia of Queyrat is unknown.
Some studies have shown that chronic irritation, inflammation, phimosis, smoking, smegma, poor hygiene, genital herpes simplex, HPV, heat, friction, maceration, trauma, perpuce dermatoses such as Lichen sclerosis or Lichen planus, may act as risk factors for developing Erythroplasia of Queyrat.[1]
Associated conditions
- Epidermodysplasia verruciformis associated HPV-8
- Genital high-risk HPV-16
Histopathology
- Slight to moderate plaque-like acanthotic epidermis with focal parakeratosis and hypogranulosis with loss of epidermal cell polarity as evidenced by vacuolated cells, atypical mitoses, atypical epithelial cells with hyperchromatic nuclei, multinucleated cells, dyskeratotic cells, and mitotic figures in the upper Malpighian layers.
- The upper dermis is often edematous and densely invaded by a band-like plasma cell rich chronic round cell infiltrate.[1]
Bowen's Disease
The exact pathogenesis of Bowen's disease is unknown.
Some studies have shown that lack of circumcision, HPV infection, phimosis, balanitis, or any chronic inflammation of the penile skin act as risk factors in developing Bowen's disease.[6]
Associated conditions
- HPV types 16[5]
- HPV type 33
Histopathology
Full-thickness epidermal atypia with disordered architecture, abnormal mitoses, dyskeratosis, and involvement of associated pilosebaceous apparatus with an intact epidermal junction.[6]
![Bowen's disease [6]histopathology](/images/c/cc/Bowen%27s_disease_histopathology.png)
Epidemiology and Demographics
There are no comprehensive studies reporting the incidence and prevalence of penile carcinoma in situ in general population. Some studies have reported the demographics of patients presenting with these conditions.
Bowenoid papulosis
Bowenoid papulosis usually occurs in sexually active men aged between 20 to 40 years, with a mean age of 31 years, it occurs slightly more common in women then men.[1]
Erythroplasia of Queyrat
Erythroplasia of Queyrat is a rare condition usually affecting uncircumcised men in their third to sixth decades of life.[1]
Bowen's Disease
Bowen's disease usually occurs equally in both men and women, with the highest incidence in patients older than age 60 years.[1]
Screening
There are no established screening guidelines to screen patients for penile carcinoma in situ.
Natural History, Complications, and Prognosis
Natural history
Bowenoid papulosis
If left untreated, papules may increase, or decrease, or disappear with time, or progress into squamous cell carcinoma(Studies have reported risk of progression of bowenoid papulosis to squamous cell carcinoma at 2.6%).[1]
Erythroplasia of Queyrat
If left untreated, Erythroplasia of Queyrat may progress into invasive Squamous cell carcinoma, with an incidence ranging from 10% to 33%.[1]
Bowen's Disease
If left untreated, Bowen's disease may progress into invasive Squamous cell carcinoma(Incidence of Bowen's disease to develop into invasive squamous cell carcinoma is 3% to 5% for cutaneous and 10% for genital lesions). The malignant potential of Bowen's disease is increased when its existence is compounded by concomitant disease such as HPV infection, Lichen sclerosis or Lichen planus, or in patients with poor genital hygiene and smokers.[1]
Complications
Complication of penile carcinoma in situ include:[1]
- Pain
- Transformation into invasive squamous cell carcinoma
Prognosis
The prognosis is usually good with treatment.
Diagnosis
History and symptoms
History and symptoms of penile carcinoma in situ include:[1][5][8]
Bowenoid papulosis
- Patients may be asymptomatic or present with pruritic, or painful lesions in the genital region.
Erythroplasia of Queyrat
- Patients may present with non-healing lesions in the genital region, which could also be associated with scaling, crusting, and bleeding.
Bowen's Disease
- Patient may be asymptomatic or present with pruritic, or painful lesions in the genital region.
Physical examination
Physical examination findings of penile carcinoma in situ include:[1]
| Physical examination findings of penile carcinoma in situ | ||
|---|---|---|
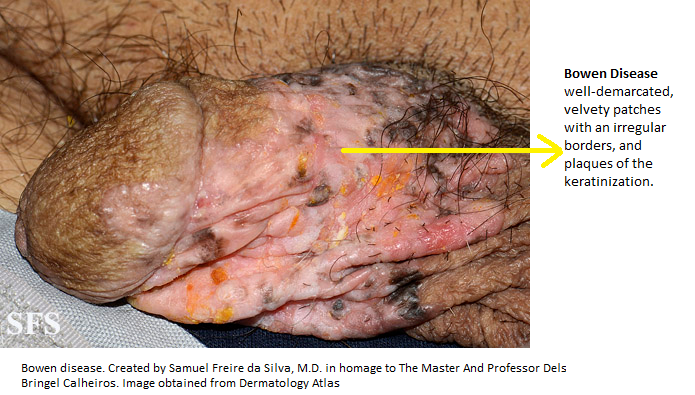
| Bowenoid papulosis | Erythroplasia of Queyrat | Bowen's Disease |
| Multiple, small, well-demarcated, grey-brown, red, pink, or skin-colored papillomatous papules or small patches on the penile shaft, glans, or foreskin, vulva, and perianal area.The papules are nonpruritic, range in size from 2 to 10 mm, and usually lack scales. |
|
Red, sometimes slightly pigmented, scaly, moist, velvety patches and plaques of keratinization on penis. |

Laboratory findings
Definite diagnosis is made by biopsy showing typical histologic picture of intraepidermal carcinoma in situ.
Treatment
Choice of treatment in penile carcinoma in situ depends after careful analysis of lesion size, number, site, degree of functional impairment, modality availability and cost.
Modalities for treating penile carcinoma in situ include:[1][5]
Bowenoid papulosis
Conservative treatment
- Topical 5-FU,or podophyllin, or retinoic acid, or cidofovir; only moderate effects have been reported.
- Imiquimod cream 5% reported successful clearance of bowenoid papulosis
Surgical treatment
Surgical modalities in treating bowenoid papulosis include:
Cryosurgery, electrodessication, laser vaporization (Nd:YAG, argon, and carbon dioxide lasers), and surgical excision. All these modalities are found to associated with scarring
Erythroplasia of Queyrat
Conservative treatment Imiquimod and Topical 5-FU application, help in minimizing the risk for scarring, poor wound healing, and functional impairment
Surgical treatment
Surgical modalities in treating Erythroplasia of Queyrat include: mohs micrographic surgery, cryotherapy, electrodesiccation and curettage, and laser ablation
Bowen's Disease
Conservative treatment
- Photodynamic therapy and Topical 5-FU application, help in minimizing the risk for scarring, poor wound healing, and functional impairment
- Recent studies have found that topical application of Imiquimod cream 5% once daily for 16 weeks was effective in treating Bowen's disease
Surgical treatment
Surgical modalities in treating bowen's disease include: Local excision, mohs micrographic surgery, cryotherapy, curettage with cautery/electrocautery, laser therapy with carbon dioxide, argon, and Nd:YAG lasers
Prevention
Primary Prevention
There are no established primary preventive measures for preventing penile carcinoma in situ.
Secondary prevention
There are no established secondary preventive measures for penile carcinoma in situ.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Kutlubay Z, Engin B, Zara T, Tüzün Y (2013). "Anogenital malignancies and premalignancies: facts and controversies". Clin Dermatol. 31 (4): 362–73. doi:10.1016/j.clindermatol.2013.01.003. PMID 23806153.
- ↑ 2.0 2.1 2.2 Kreuter A, Brockmeyer NH, Pfister H, Altmeyer P, Wieland U, German Competence Network HIV/AIDS (2007). "Increased human papillomavirus type 31 DNA load in a verrucous high-grade intraepithelial neoplasia of a human immunodeficiency virus-infected patient with extensive bowenoid papulosis". Br J Dermatol. 156 (3): 596–8. doi:10.1111/j.1365-2133.2007.07690.x. PMID 17300265.
- ↑ Matuszewski M, Michajłowski I, Michajłowski J, Sokołowska-Wojdyło M, Włodarczyk A, Krajka K (2009). "Topical treatment of bowenoid papulosis of the penis with imiquimod". J Eur Acad Dermatol Venereol. 23 (8): 978–9. doi:10.1111/j.1468-3083.2008.03083.x. PMID 19207667.
- ↑ Conejo-Mir JS, Muñoz MA, Linares M, Rodríguez L, Serrano A (2005). "Carbon dioxide laser treatment of erythroplasia of Queyrat: a revisited treatment to this condition". J Eur Acad Dermatol Venereol. 19 (5): 643–4. doi:10.1111/j.1468-3083.2005.01217.x. PMID 16164731.
- ↑ 5.0 5.1 5.2 5.3 Henquet CJ (2011). "Anogenital malignancies and pre-malignancies". J Eur Acad Dermatol Venereol. 25 (8): 885–95. doi:10.1111/j.1468-3083.2010.03969.x. PMID 21272092.
- ↑ 6.0 6.1 6.2 6.3 Arlette JP (2003). "Treatment of Bowen's disease and erythroplasia of Queyrat". Br J Dermatol. 149 Suppl 66: 43–9. PMID 14616349.
- ↑ Stables GI, Stringer MR, Robinson DJ, Ash DV (1999). "Erythroplasia of Queyrat treated by topical aminolaevulinic acid photodynamic therapy". Br J Dermatol. 140 (3): 514–7. PMID 10233277.
- ↑ Buechner SA (2002). "Common skin disorders of the penis". BJU Int. 90 (5): 498–506. PMID 12175386.