Paget's disease of bone
For patient information click here
| Paget's disease of bone |
|
Paget's disease of bone Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Paget's disease of bone On the Web |
|
American Roentgen Ray Society Images of Paget's disease of bone |
|
Risk calculators and risk factors for Paget's disease of bone |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou [2];
Synonyms and Keywords: Commonly known as Paget's disease; Historically known as osteitis deformans
Overview
Paget's disease, otherwise known as osteitis deformans the disease is named after the English surgeon Sir James Paget[1][2]. It is the second most common bone disease after osteoporosis worldwide[3]. It is characterized by focal regions of highly exaggerated bone remodeling, with different abnormalities in all phases of the bone remodeling process[4]. Paget's diseases of bone is a chronic disorder that typically results in enlarged and deformed bones[5][6]. It is named after Sir James Paget, the British surgeon who first described this problem[7]. [8]The excessive breakdown and formation of bone tissue that occurs with Paget's disease can cause bone to weaken, resulting in bone pain, arthritis, deformities, and fractures. Paget's disease may be caused by a slow virus infection (i.e., paramyxoviruses such as measles and respiratory syncytial virus), present for many years before symptoms appearClosing </ref> missing for <ref> tag: indications for treatment and review of current therapies |journal=J. Bone Miner. Res. |volume=21 Suppl 2 |issue= |pages=P94–8 |date=December 2006 |pmid=17229018 |doi=10.1359/jbmr.06s218 |url=}}</ref>. There is also a hereditary factor since the disease may appear in more than one family member[9]. Paget's disease is rarely diagnosed in people less than 40 years of age[10]. Men are more commonly affected than women. Prevalence of Paget's disease ranges from 1.5 to 8 percent depending on age and country of residence[11]. Prevalence of familial Paget's disease (where more than one family member has the disease) ranges from 10 to 40 percent in different parts of the world. Because early diagnosis and treatment is important, after age 40, siblings and children of someone with Paget's disease may wish to have an alkaline phosphatase blood test every 2 or 3 years. If the alkaline phosphatase level is above normal, other tests such as a bone-specific alkaline phosphatase test, bone scan, or x-ray can be performed[5][12][2].
Paget's disease of bone affects the normal body's bone recycling process, in which new bone tissue gradually replaces old bone tissue. Accordingly, the disease made bone fragile and misshapen[6]. Paget's disease of bone can affect any bone in human body[11]. It appears most often in the spine, pelvis, long bones of the limbs, and skull[6]. It can be present in just one bone or in several bones. It can affect the entire bone or just part of it[5][2].
The risk of Paget's disease of bone increases with age. Paget's disease of bone most commonly affects the pelvis, skull, spine and legs[5]. Complications of Paget's disease of bone are broken bones, hearing loss and pinched nerves in spine[11]. Bisphosphonates — the medications also used to strengthen bones weakened by osteoporosis — are the mainstay of treatment. For patients who have complications, surgery may be necessary[12]. Paget disease may involve a single bone but is more frequently multifocal[6].
Historical Perspective
Paget's disease of bone initially described by Dr. James Paget[4]. In a paper published in 1877, Dr. James Paget reported five patients with "a rare disease of bones" which presented with slowly progressive bone deformities in the 4th and 5th decades of age[5][6][2]:
The first patient was described to have many of the classic complications of the disease, including arthritis related to abnormal bone mechanics, cranial nerve palsies associated with an enlarging skull, and malignant transformation of a tumor of the radius which ultimately proved fatal[3][11].
Paget's post-mortem autopsy revealed that the bones of the vault of this skull were in every part increased to about four times the normal thickness, and microscopic evaluation showed evidence of both bone erosion and abnormal remodeling[6]. Although he incorrectly attributed the findings to a process of chronic inflammation, having ruled out tumor and hypertrophy as alternative etiologies, these prescient observations of a mixed destructive/regenerative process correspond to the modern understanding of the disease[5].
Paget's disease of bone was originally termed osteitis deformans, because it was thought to involve an inflammatory process, which is implied by the suffix -itis. Now, that term is considered technically incorrect, and the preferred term is osteodystrophia deformans[2].
Classification
Pathophysiology
Sir James Paget first suggested the disease was due to an inflammatory process[5]. Some evidence suggests that a paramyxovirus infection is the underlying cause of Paget's disease, which may support the possible role of inflammation in the pathogenesis. However, no infectious virus has yet been isolated as a causative agent, and other evidence suggests an intrinsic hyperresponsive reaction to vitamin D and RANK ligand is the cause. Further research is therefore necessary[4].This osteoclastic overactivity followed by compensatory osteoblastic activity leads to a structurally disorganized mosaic of bone (woven bone), which is mechanically weaker, larger, less compact, more vascular, and more susceptible to fracture than normal adult lamellar bone[11]. Meanwhile, the pathogenesis of Paget's disease of bone is described in four stage[13]s:
- Osteoclastic activity
- Mixed osteoclastic – osteoblastic activity
- Osteoblastic activity
- Malignant degeneration
In normal bone, a normal process called remodeling. Bone is absorbed and then reformed in response to the normal stresses on the skeleton.
- Osteoclasts: cells that absorb bone.
- Osteoblasts: cells that make new bone.
In Paget's disease, osteoclasts are more active than osteoblasts. This means that there is more bone absorption than normal. The osteoblasts try to keep up by making new bone, but they overreact and make excess bone that is abnormally large and deformed.Since in normal bone there is a tight overlapping structure, like a well-constructed brick wall. Bone involved with the Paget's disease has an irregular mosaic pattern, as though the bricks were just dumped in place consequently the bones are large and dense, but weak and brittle. The bone is prone to fractures, bowing, and deformities.
Causes
The main cause /causes of Paget's disease of bone is not well known yet[5]. But its thought that a combination of environmental and genetic factors contribute to this disease. Several genes appear to be linked to the occurrence of the disease[11]. Also it might be related to a viral infection in bone cells, but this theory is controversial[14][4].
- Age. Paget's disease occurs only rarely in people under 40 years of age. It is more common as people age[2].
- Ancestry. It is more common in people of Anglo-Saxon descent and those who live in certain geographic areas, such as the United States, England, Australia, New Zealand, and Western Europe. It is not common in Scandinavia, China, Japan, or India[15][13].
- Environmental factors. Some studies suggest that certain environmental exposures may play a role in the development of Paget's disease. This has not been proven definitively, however.
- Viral. Paget's disease may be caused by a slow virus infection (i.e., paramyxoviridae) present for many years before symptoms appear. Suspected viral infections include respiratory syncytial virus, canine distemper virus, and the measles virus. However, recent evidence has cast some doubt upon the measles association. Laboratory contamination may have played a role in past studies linking paramyxovirus (e.g. measles) to Paget's disease.
- Genetics. In around 15-40% of affected patients had a first-degree relative with Paget disease. Numerous other studies have described families exhibiting autosomal dominant inheritance involved in this disease[14].
- Mutations in the sequestosome SQSTM1/p62 gene (which is a selective activator of NFB (nuclear factor kappa-B) transcription factor, involved in osteoclast differentiation in addition to the activation in response to the cytokines interleukin-1 (IL-1) and RANKL (receptor activator of nuclear factor kappa-B ligand) were found in 30% of familial Paget cases[13].
- How germline DNA mutations can cause bone disease that is focal in nature remains unclear
- There is an association between human leukocyte antigen–A (HLA-A(DQW1 and DR2 antigens (class II HLA))), HLA-B, and HLA-C (class I) and clinical evidence of disease.
- There is a hereditary factor in the development of Paget's disease of bone[13]. Two genes, SQSTM1 and RANK, and specific regions of chromosome 5 and 6 are associated with Paget's disease of bone. Genetic causes may or may not involve a family history of Paget's disease[13].
- About 40–50% of people with the inherited version of Paget's disease have a mutation in the gene SQSTM1, which encodes a protein, called p62, that is involved in regulating the function of osteoclasts (bone cells). However, about 10-15 percent of people that develop the disease without any family history also have a mutation in the SQSTM1 gene[4].
- Paget's disease of bone is associated with mutations in RANK. Receptor Activator of Nuclear Factor κ B (RANK), which is a type I membrane protein that is expressed on the surface of osteoclasts and is involved in their activation upon ligand binding. Additional genetic associations include[2][13]:
| Name | OMIM | Locus | Gene |
|---|---|---|---|
| PDB1 | 167250 | 6p | ? |
| PDB2 | 18q22.1 | RANK | |
| PDB3 | 5q35 | SQSTM1 | |
| PDB4 | 606263 | 5q31 | ? |
- Other causes: Autoimmune, connective tissue, and vascular disorders are proposed as other possible etiologies.
Differentiating Paget's disease of bone from Other Diseases
| Condition | Calcium | Phosphate | Alkaline phosphatase | Parathyroid hormone | Comments |
|---|---|---|---|---|---|
| Osteopenia | unaffected | unaffected | normal | unaffected | decreased bone mass |
| Osteopetrosis | unaffected | unaffected | elevated | unaffected | thick dense bones also known as marble bone |
| Osteomalacia and rickets | decreased | decreased | elevated | elevated | soft bones |
| Osteitis fibrosa cystica | elevated | decreased | elevated | elevated | brown tumors |
| Paget's disease of bone | unaffected | unaffected | variable (depending on stage of disease) | unaffected | abnormal bone architecture |
Epidemiology and Demographics
Pagets disease of bone is the second most common metabolic bone disorder, after osteoporosis[5]. Most of patients with Paget disease are asymptomatic[11][2][14].
United States statistics
Paget disease affects 1 to 3 million people in the United States of America. Based on data from the National Health and Nutrition Examination Survey I (NHANES I, 1971-1975) the prevalence of pelvic Paget disease in the United States was 0.71% ± 0.18%, and the male-to-female ratio was 1.2:1, Also the prevalence of pelvic Paget disease was reported similar in white persons and black persons[5][2][4].
The prevalence of pelvic Paget disease increases with age, with the highest prevalence in persons older than 65 years. A survey study suggested that the prevalence in the United States is 2.3% of the population between ages 65 and 74 years[2][14].
Paget disease is estimated to occur in 1-3% of individuals older than 45-55 years and in up to 10% of persons older than 80 years. Geographically, pelvic Paget disease was least common in the southern United States and most common in the northeastern United States[2][14][4].
International statistics
he prevalence of Paget disease varies greatly in different areas of the world[5].
- Paget's disease is rare in people less than 55 years of age, and the prevalence increases with age and it involves about 3 percent of people older than 40 years of age (90% are over age 55, rare before age 40)[2][4].
- Paget's disease is almost around the 50 percent higher in men than in women.
- About 15 percent of people with Paget's disease also have a family member with the disease.
- The incidence of Paget's disease varies considerably with geographic location:
- Paget's predominantly affects people of European descent, whereas people of African, Asian, or Indian descent are less commonly affected.
- Paget's disease is less common in Switzerland and Scandinavia than in the rest of Western Europe.
- Paget's disease is uncommon in the native populations of North and South America, Africa, Asia, and the Middle East. When an individual from these regions does develop Paget's disease, there is typically some European ancestry present.
- Likelihood of occurrence increases with age
- Radiologic surveys show the frequency in adults is less than 1% in the Great Britain, and Australia
- The disease is rare in India, Japan, Scandanavia, and the Middle East
- More common in whites in U.S., England (3% at autopsy), France, Austria, Germany, Australia, New Zealand (5 - 11%); rare in blacks, Scandinavia, China
- The prevalence of Paget disease in sub-Saharan Africa is 0.01-0.02%.
- In Israel, Paget disease is predominantly found in Jews; however, cases have recently been reported in Israeli Arabs.
Risk Factors
Risk factors of Paget's disease of bone include[5][6][2][14][4]:
- Age. People older than 40 are most likely to develop Paget's disease of bone.
- Sex. Men are more commonly affected than are women.
- National origin. Paget's disease of bone is more common in England, Scotland, central Europe and Greece. It's uncommon in Scandinavia and Asia.
- Family history. Having a relative with Paget's disease of bone more likely develop the risk of Paget's disease of bone.
Screening
Natural History, Complications, and Prognosis
Natural History
Paget's disease is a frequent component of multisystem proteinopathy[14][6]. Advanced Paget's disease may lead to other medical conditions, including[2][3]:
- Osteoarthritis may result from changes in bone shape that alter normal skeletal mechanics. For example, bowing of a femur affected by Paget's may distort overall leg alignment, subjecting the knee to abnormal mechanical forces and accelerating degenerative wear[3].
- Heart failure is a rare, reported consequence of severe Paget's disease (i.e. more than 40% skeletal involvement). The abnormal bone formation is associated with recruitment of abnormal blood vessels, forcing the cardiovascular system to work harder (pump more blood) to ensure adequate circulation.
- Kidney stones are somewhat more common in patients with Paget's disease[3].
- Nervous system problems may occur in Paget's disease, resulting from increased pressure on the brain, spinal cord, or nerves, and reduced blood flow to the brain and spinal cord[4].
- When Paget's disease affects the facial bones, the teeth may become loose. Disturbance in chewing may occur. Chronic dental problems may lead to infection of the jaw bone.
- Angioid streaks may develop, possibly as a result of calcification of collagen or other pathological deposition.
- Vulvar Paget's disease ulceration can occur in female reproductive organs.
Paget's disease is not associated with osteoporosis. Although Paget's disease and osteoporosis can occur in the same patient, they are different disorders. Despite their marked differences, several treatments for Paget's disease are also used to treat osteoporosis[13]
Complications
In most patients the Paget's disease of bone progresses slowly[6]. The point is this disease can be managed effectively in nearly all people[3]. Possible complications of Paget's disease of bone include[2][14]:
- Fractures and deformities. Affected bones break more easily. Extra blood vessels in these deformed bones cause them to bleed more during surgeries. Leg bones can bow, which can affect ability to walk[15].
- Osteoarthritis. Misshapen bones can increase the amount of stress on nearby joints, which can cause osteoarthritis.
- Neurologic problems. When Paget's disease of bone occurs in an area where nerves pass through the bone, such as the spine and skull, the overgrowth of bone can compress and damage the nerve, causing pain, weakness or tingling in an arm or leg or hearing loss.
- Heart failure. Extensive Paget's disease of bone may force heart to work harder to pump blood to the affected areas of body. Sometimes, this increased workload can lead to heart failure.
- Bone cancer. Bone cancer occurs in about 1 percent of people with Paget's disease of bone..
Prognosis
The general outlook for patients with Paget disease is good, especially if treatment is administered before major changes have occurred in the bones[6]. The Paget's disease of boneis progressive and slowly worsens by time, and the affected people may remain minimally symptomatic. Since there is no cure the treatment is aimed at controlling symptoms. Any bone or bones can be affected, but Paget's disease occurs most frequently in the spine, skull, pelvis, femur, and lower legs[2][15][3][14][4].
Osteogenic sarcoma, a form of bone cancer, is a rare complication of Paget's disease occurring in less than 1 % of those affected with Paget's disease of bone[13]. The development of osteosarcoma may be suggested by the sudden onset or worsening painClosing </ref> missing for <ref> tag[4][8]. Biannual Foothills Meeting on Osteoporosis, Calgary, Alberta, Canada, September 9-10, 2000 |journal=Clin Ther |volume=23 |issue=4 |pages=620–6 |date=April 2001 |pmid=11354395 |doi= |url=}}</ref>[3][14].
Diagnosis
Lab tests
- People who have Paget's disease of bone usually have elevated levels of bone-specific alkaline phosphatase (marker of bone formation)in the blood in combination with normal calcium, phosphate, and aminotransferase levels in their blood, which can be revealed by a blood test[3][6][2][8][14][4].
- Also, Markers of bone turnover in urine eg. Pyridinoline
- Elevated levels of serum and urinary hydroxyproline are also found[15][3][8][4].
- Deoxypyridinoline (marker of bone resorption)
- N -Telopeptide of type I collagen (marker of bone resorption)
- Alpha-alpha type I C-telopeptide fragments
Diagnostic Criteria
History and Symptoms
Many patients do not know they have Paget's disease of bone because they have a mild case with no symptoms[6]. When symptoms occur, the most common complaint is bone pain.Sometimes, symptoms may be confused with those of arthritis or other disorders. Due to the nature of this disease which causes the generation of new bone faster than normal, the rapid remodeling produces leads to softer and weaker bone; accordingly this process cause the bone pain, deformities and fractures[2][8][14][4].
Meanwhile the symptoms of the Paget's disease of bone are[4]:
- Bone pain is the most common symptom[6]. Bone pain can occur in any bone affected by Paget's disease[8]. It often localizes to areas adjacent to the joints[3][14].
- Excessive warmth (due to hypervascularity)
- Neurologic complications (caused by the compression of neural tissues)
- Headaches and hearing loss due to the overgrowth of bone when Paget's disease affects the skull.
- Pressure on nerves may occur when Paget's disease affects the skull or spine consequently there might be pain, tingling and numbness in an arm or leg.
- Somnolence (drowsiness) due to vascular steal syndrome of the skull.
- Paralysis due to vascular steal syndrome of the vertebrae.
- Increased head size, bowing of limb, or curvature of spine may occur in advanced cases.
- Hip pain may occur when Paget's disease affects the pelvis or thighbone.
- Damage to joint cartilage may lead to arthritis.
- Teeth may spread intraorally.
- Chalkstick fractures.
- Fatigue
- Weakness
- Loss of appetite
- Abdominal pain
- Constipation
Physical Examination
Paget's disease may be diagnosed using one or more of the following tests[6][4]:
- Pagetic bone has a characteristic appearance on x-rays. A skeletal survey is therefore indicated.
- An elevated level of alkaline phosphatase in the blood in combination with normal calcium, phosphate, and aminotransferase levels in an elderly patient are suggestive of Paget's disease[2].
- Urinary Hydroxyproline has been elevated in many patients and it is a marker used traditionally[8].
- Bone scans are useful in determining the extent and activity of the condition. If a bone scan suggests Paget's disease, the affected bone(s) should be x-rayed to confirm the diagnosis[2][14].
Laboratory Findings
Electrolyte and Biomarker Studies
There is an elevation of the alkaline phosphatase in patients blood, which can be revealed by a blood test[6][8][4].
Imaging Findings
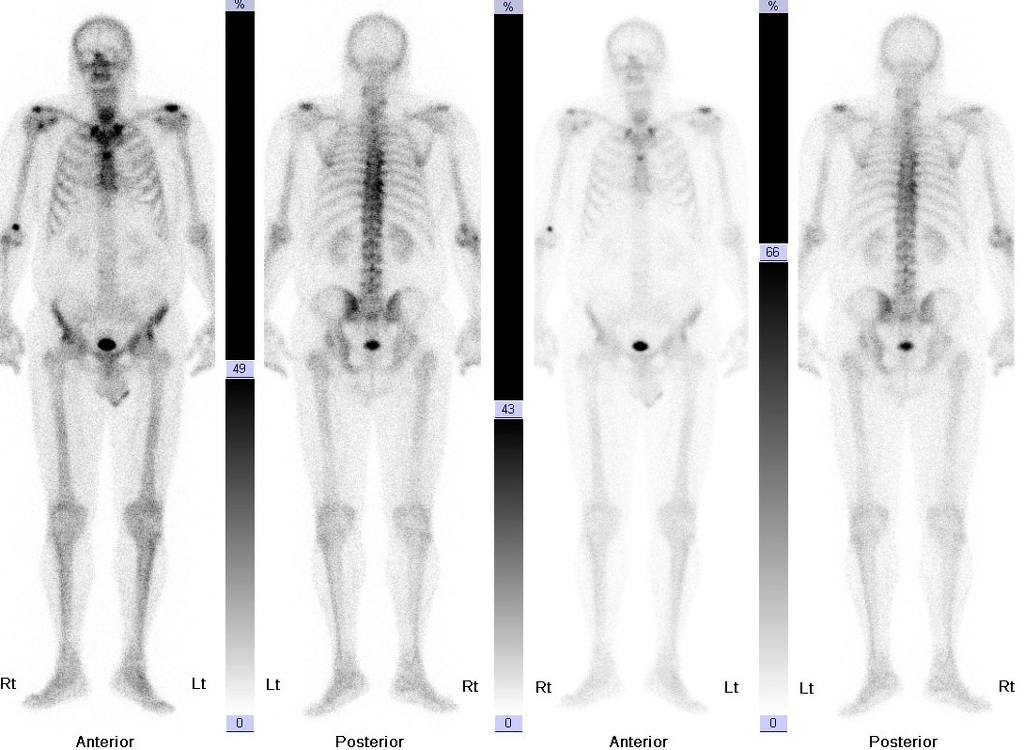
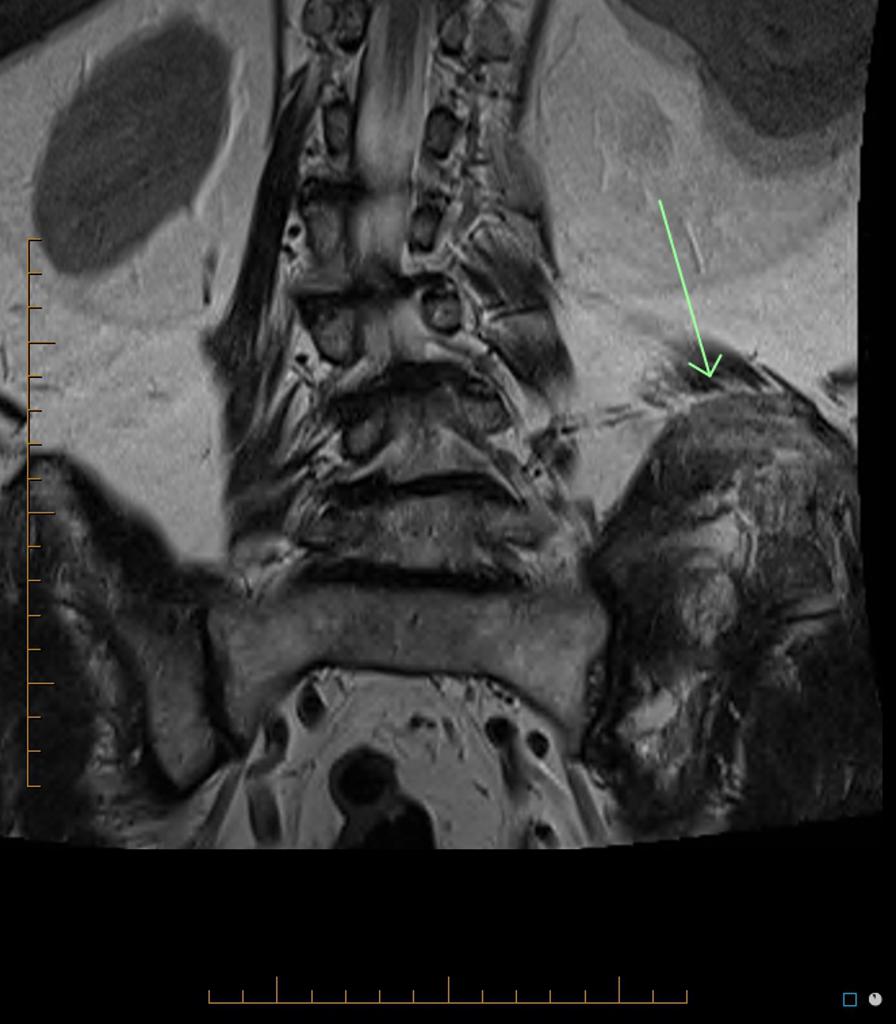
Bone changes due to the Paget's disease of bone can be investigated using[4]:
- X-rays.

Case courtesy of Dr Laughlin Dawes , <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/7477">rID: 7477</a> 
Case courtesy of Dr Björn Jobke, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/39303">rID: 39303</a> 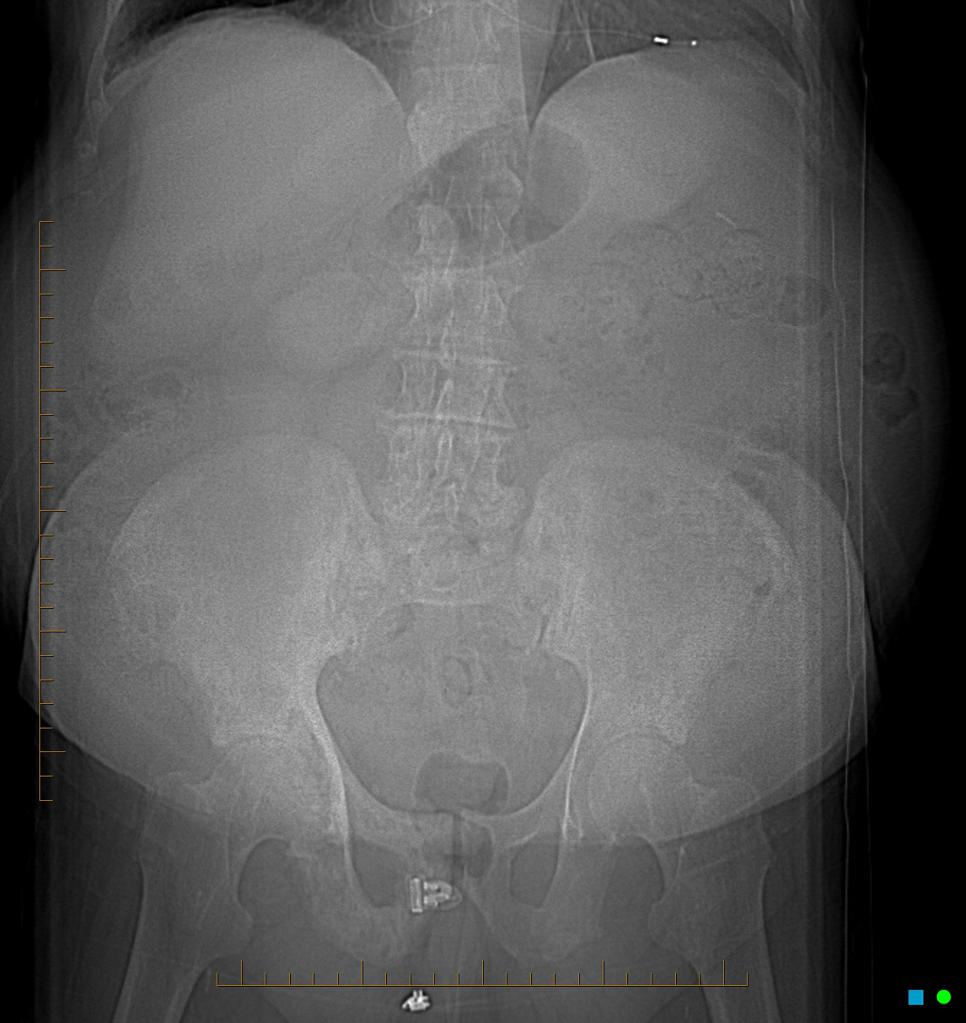
Case courtesy of A.Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/7476">rID: 7476</a> 
Case courtesy of A.Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/8031">rID: 8031</a> 
Case courtesy of A.Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/8032">rID: 8032</a> 
Case courtesy of <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/11727">rID: 11727</a> - The first indication of Paget's disease of bone is often abnormalities found on X-rays done for other purposes. Meanwhile, the X-ray imaging can show reabsorption of bone, enlargement of the bone and deformities that are characteristic of Paget's disease of bone, such as bowing of the long bones[14].
- Bone scan.
- In a bone scan, radioactive material is injected into body and this material travels to the spots on your bones most affected by Paget's disease of bone, so they light up on the scan images.
Other Diagnostic Studies
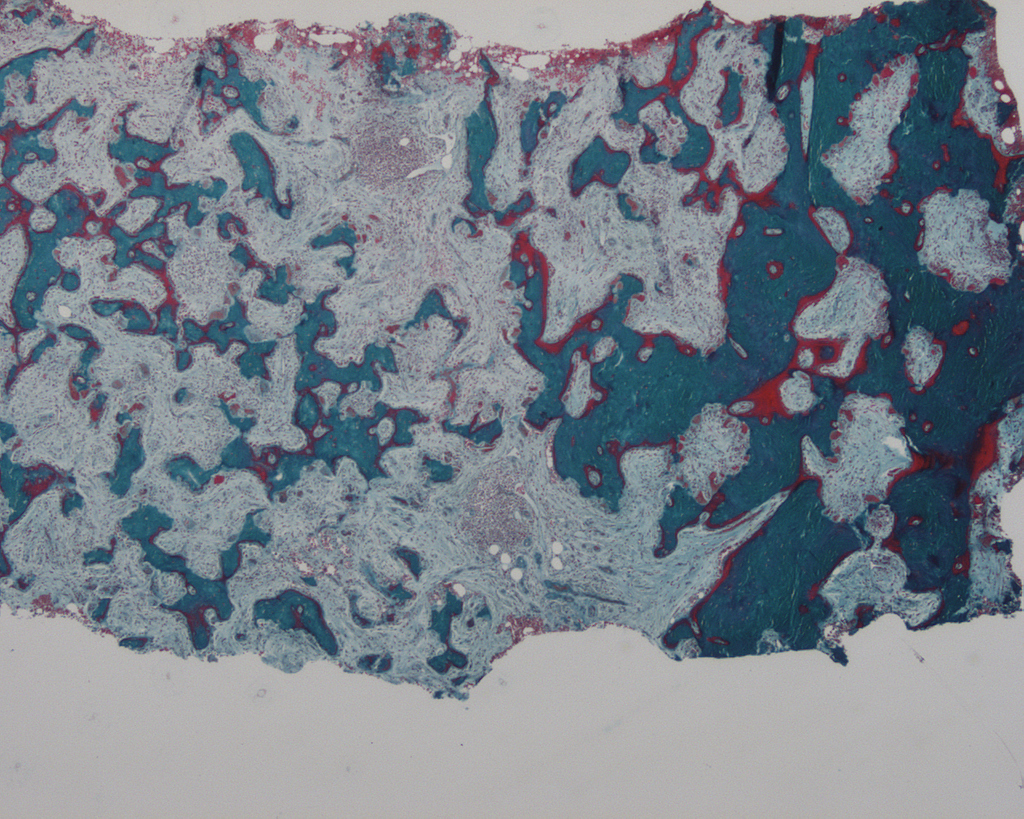
Bone biopsy
A biopsy is sometimes necessary to confirm the diagnosis of Paget's disease or to rule out other conditions[4][8]. In a biopsy, a small sample of the affected bone is removed and examined under a microscope[16]. The procedure can be performed under local anesthesia with a needle or as a small open operation[14]. x Computed tomography (CT) scanning and magnetic resonance imaging (MRI) are recommended for the diagnosis of Paget disease of bone. But, both are useful in the evaluation of related complications such as neoplastic degeneration, articular abnormalities, and spinal involvement with neurologic compromise[8].

Treatment
There is no cure for Paget’s disease and no way to reverse its effects on bone. Treatment focuses on relieving symptoms and preventing future complications[17]. If the disease is active (According to the elevated alkaline phosphatase level and other indicative founding) and affecting important and high-risk sites in body, such as skull or spine then the treatment are necessary to prevent complications, even if you don't have symptoms[14]. The goal of treatment is to relieve bone pain and prevent the progression of the disease[16]. The U.S. Food and Drug Administration has approved the following treatments for Paget's disease[2][4]:
Medications
Osteoporosis drugs (bisphosphonates) are the most common treatment for Paget's disease of bone. Oral bisphosphonates are generally well-tolerated, but they may irritate your gastrointestinal tract. [12][15]:
Medical Therapy
The goal of treatment is to relieve bone pain and prevent the progression of the disease[15]. The U.S. Food and Drug Administration has approved the following treatments for Paget's disease[12][18][14]:
Chronic Pharmacotherapies
Cytotoxic drugs like plicamycin and dactinomycin are no longer used for therapy[12]:[18][15][14]:
- Bisphosphonates are used to inhibit bone resorption
- Etidronate has been used at 20 mg/kg body weight per day and is effective in producing clinical improvement
- osteomalacia is a potential complication of therapy
- Alendronate (Fosamax), pamidronate, risendronate, and tiludronate are the bisphosphonates most commonly used now as they are more potent than etidronate and do not result in the same mineralization defects
- Alendronate is approx. 700-fold more potent than etidronate
- Alendronate (oral administration) and pamidronate (intravenous administration) are approved for use in the US
Common bisphosphonates and their use[18]:
- Alendronate is administered orally with water 30-60 minutes before breakfast after an overnight fast
- Dose is 40 mg/d for 6 months
- Pamidronate is given intravenously
- Dose is 30 mg/d in 5% glucose in water or normal saline over 4h ion 3 successive days
- Calcitonin will be replaced by bisphosphonates for primary treatment of severe disease, but calcitonin can still be used for patients who cannot tolerate alendronate due to gastrointestinal side effects[18]
- The administration of calcitonins suppresses the pagetic lesion which leads to a decrease in bone pain.
- Calcitonin also improves neurologic symptoms and decreases elevated cardiac output
- Some individuals do not respond to porcine or salmon calcitonins
- Calcitonin can be administered by nasal spray at doses of 200 IU/d.
Bisphosphonate
Five bisphosphonates are currently available. In general, the most commonly prescribed are the three most potent bisphosphonates: Actonel®, Fosamax® and Aredia®. Didronel® and Skelid® may be appropriate therapies for selected patients but are less commonly used. As a rule, bisphosphonate tablets should be taken with 6-8 oz of tap water on an empty stomach. None of these drugs should be used by people with severe kidney disease.
- Didronel® (etidronate disodium) -- Tablet; approved regimen is 200-400 mg once daily for 6 months; the higher dose (400 mg) is more commonly used; no food, beverages, or medications for 2 hours before and after taking; course should not exceed 6 months, but repeat courses can be given after rest periods, preferably of 3-6 months duration.
- Aredia® (pamidronate disodium) -- Intravenous; approved regimen 30 mg infusion over 4 hours on 3 consecutive days; more commonly used regimen 60 mg over 2-4 hours for 2 or more consecutive or non-consecutive days.
- Fosamax® (alendronate sodium) -- Tablet; 40 mg once daily for 6 months; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
- Skelid® (tiludronate disodium) -- Tablet; 400 mg (two 200 mg tablets) once daily for 3 months; may be taken any time of day, as long as there is a period of 2 hours before and after resuming food, beverages, and medications.
- Actonel® (risedronate sodium) -- Tablet; 30 mg once daily for 2 months; patients should wait at least 30 minutes after taking before eating any food, drinking anything other than tap water, taking any medication, or lying down (patient may sit).
Calcitonin
- Miacalcin® is administered by injection; 50 to 100 units daily or 3 times per week for 6-18 months. Repeat courses can be given after brief rest periods. Miacalcin may be appropriate for certain patients but is seldom used. The nasal spray form of this drug is not approved for the treatment of Paget's disease.
Rarely, bisphosphonate therapy has been linked to severe muscle, joint or bone pain, which might not resolve when the medication is discontinued. Bisphosphonates can also increase the risk of a rare condition in which a section of jawbone dies and deteriorates (osteonecrosis of the jawbone), usually associated with active dental disease or oral surgery.
If patinets can't tolerate bisphosphonates, the n the calcitonin (Miacalcin), a naturally occurring hormone involved in calcium regulation and bone metabolism should be considered in this regard. Side effects may include nausea, facial flushing and irritation at the injection site[18][19][19][15][14].
Surgery
In some cases, surgery may be needed to treat the complications of Paget's disease, including[18][20][2]:
- Bone fractures
- Malalignment or deformity of bone
- Severe arthritis
- Reduce pressure on nerves
The surgical procedures used to treat fractures, malalignment, or arthritis in patients with Paget's disease are similar to normal population[20][8].
These procedures may include[20][8][14]:
- Internal fixation. This procedure can be used to treat fractures in bone affected by the disease. In internal fixation, bone fragments are first repositioned into their normal alignment, then held in place with screws, wires, pins, or metal plates attached to the outside of the bone.
- Osteotomy. An osteotomy can help relieve pain and restore alignment to weight-bearing joints that are affected by Paget’s disease, especially the knee and hip. During the procedure, your doctor will remove a wedge of bone near the damaged joint in order to shift weight onto a healthier part of the joint.
- Total joint replacement. In this procedure, parts of an arthritic or damaged joint are removed and replaced with a metal, plastic or ceramic device called a prosthesis. The prosthesis is designed to replicate the movement of a normal, healthy joint[2].
Paget's disease of bone causes the body to produce too many blood vessels in the affected bones, increasing the risk of serious blood loss during an operation. Medical therapy prior to surgery helps to decrease bleeding and other complications. There are generally three major complications of Paget's disease for which surgery may be recommended.
- Fractures -- Surgery may allow fractures to heal in better position[2].
- Severe degenerative arthritis -- If disability is severe and medication and physical therapy are no longer helpful, joint replacement of the hips and knees may be considered.
- Bone deformity -- Cutting and realignment of Pagetic bone (osteotomy) may help painful weight-bearing joints, especially the knees[21].
Complications resulting from enlargement of the skull or spine may injure the nervous system. However, most neurologic symptoms, even those that are moderately severe, can be treated with medication and do not require neurosurgery[20][21][2][14].
Prevention
While there are no known ways to prevent Paget's disease from occurring, eating a healthy diet with sufficient calcium and vitamin D, and getting regular exercise, are important components in maintaining skeletal health and joint mobility. To reduce your risk of complications associated with Paget's disease of bone, the following mentioned factor can be helpful[20][21][4]:
- Prevent falls
- Diet
In general, patients with Paget's disease should receive 1000-1500 mg of calcium, adequate sunlight, and at least 400 units of vitamin D daily. This is especially important in patients being treated with bisphosphonates[14]. Patients with a history of kidney stones should discuss calcium and vitamin D intake with their physician[21][2].
- Exercise regularly. Exercise is very important in maintaining skeletal health, avoiding weight gain, and maintaining joint mobility. Since undue stress on affected bones should be avoided, patients should discuss any exercise program with their physician before beginning.Regular exercise is essential for maintaining joint mobility and bone strength[14]. Some activities may place too much stress on the affected bones[20][21][4].
References
- ↑ Asel M, LeBoeuf NR (February 2019). "Extramammary Paget's Disease". Hematol. Oncol. Clin. North Am. 33 (1): 73–85. doi:10.1016/j.hoc.2018.09.003. PMID 30497678.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 Drake WM, Kendler DL, Brown JP (April 2001). "Consensus statement on the modern therapy of Paget's disease of bone from a Western Osteoporosis Alliance symposium. Biannual Foothills Meeting on Osteoporosis, Calgary, Alberta, Canada, September 9-10, 2000". Clin Ther. 23 (4): 620–6. PMID 11354395.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Ralston SH, Langston AL, Reid IR (July 2008). "Pathogenesis and management of Paget's disease of bone". Lancet. 372 (9633): 155–63. doi:10.1016/S0140-6736(08)61035-1. PMID 18620951.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 Muschitz C, Feichtinger X, Haschka J, Kocijan R (February 2017). "Diagnosis and treatment of Paget's disease of bone : A clinical practice guideline". Wien Med Wochenschr. 167 (1–2): 18–24. doi:10.1007/s10354-016-0502-x. PMID 27600563.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 Sieghart S (2004). "[Osteitis deformans--Paget's disease]". Wien Med Wochenschr (in German). 154 (5–6): 97–101. PMID 15106891.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 Michou L, Brown JP (2011). "Emerging strategies and therapies for treatment of Paget's disease of bone". Drug Des Devel Ther. 5: 225–39. doi:10.2147/DDDT.S11306. PMC 3096538. PMID 21607019.
- ↑ Kravets I (November 2018). "Paget's Disease of Bone: Diagnosis and Treatment". Am. J. Med. 131 (11): 1298–1303. doi:10.1016/j.amjmed.2018.04.028. PMID 29752905.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 Schneider D, Hofmann MT, Peterson JA (May 2002). "Diagnosis and treatment of Paget's disease of bone". Am Fam Physician. 65 (10): 2069–72. PMID 12046775.
- ↑ Abelson A (March 2008). "A review of Paget's disease of bone with a focus on the efficacy and safety of zoledronic acid 5 mg". Curr Med Res Opin. 24 (3): 695–705. doi:10.1185/030079908X260899. PMID 18226324.
- ↑ De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A, Singer F. PMID 25905262. Missing or empty
|title=(help) - ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Langston AL, Ralston SH (August 2004). "Management of Paget's disease of bone". Rheumatology (Oxford). 43 (8): 955–9. doi:10.1093/rheumatology/keh243. PMID 15187244.
- ↑ 12.0 12.1 12.2 12.3 12.4 Umland EM, Boyce EG (September 2001). "Risedronate: a new oral bisphosphonate". Clin Ther. 23 (9): 1409–21. PMID 11589256.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Roodman GD (August 2001). "Studies in Paget's disease and their relevance to oncology". Semin. Oncol. 28 (4 Suppl 11): 15–21. PMID 11544571.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 14.14 14.15 14.16 14.17 14.18 14.19 14.20 14.21 14.22 14.23 Reid IR, Nicholson GC, Weinstein RS, Hosking DJ, Cundy T, Kotowicz MA, Murphy WA, Yeap S, Dufresne S, Lombardi A, Musliner TA, Thompson DE, Yates AJ (October 1996). "Biochemical and radiologic improvement in Paget's disease of bone treated with alendronate: a randomized, placebo-controlled trial". Am. J. Med. 101 (4): 341–8. PMID 8873503.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 Walsh JP, Ward LC, Stewart GO, Will RK, Criddle RA, Prince RL, Stuckey BG, Dhaliwal SS, Bhagat CI, Retallack RW, Kent GN, Drury PJ, Vasikaran S, Gutteridge DH (April 2004). "A randomized clinical trial comparing oral alendronate and intravenous pamidronate for the treatment of Paget's disease of bone". Bone. 34 (4): 747–54. doi:10.1016/j.bone.2003.12.011. PMID 15050907.
- ↑ 16.0 16.1 Tiegs RD (1997). "Paget's disease of bone: indications for treatment and goals of therapy". Clin Ther. 19 (6): 1309–29, discussion 1523–4. PMID 9444442.
- ↑ Reginster JY, Lecart MP (November 1995). "Efficacy and safety of drugs for Paget's disease of bone". Bone. 17 (5 Suppl): 485S–488S. PMID 8573423.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 Reid IR, Sharma S, Kalluru R, Eagleton C (September 2016). "Treatment of Paget's Disease of Bone with Denosumab: Case Report and Literature Review". Calcif. Tissue Int. 99 (3): 322–5. doi:10.1007/s00223-016-0150-6. PMID 27193832.
- ↑ 19.0 19.1 Tucci JR, Bontha S (2001). "Intravenously administered pamidronate in the treatment of Paget's disease of bone". Endocr Pract. 7 (6): 423–9. doi:10.4158/EP.7.6.423. PMID 11747277.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 Siris ES (July 1998). "Paget's disease of bone". J. Bone Miner. Res. 13 (7): 1061–5. doi:10.1359/jbmr.1998.13.7.1061. PMID 9661069.
- ↑ 21.0 21.1 21.2 21.3 21.4 Walsh JP (September 2004). "Paget's disease of bone". Med. J. Aust. 181 (5): 262–5. PMID 15347275.