Ringworm
| Ringworm | |
 | |
|---|---|
| Ringworm on the arm | |
| ICD-10 | B35.4 |
| ICD-9 | 110.9 |
| DiseasesDB | 17492 |
| eMedicine | emerg/592 |
| MeSH | D014005 |
|
Dermatophytosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ringworm On the Web |
|
American Roentgen Ray Society Images of Ringworm |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ringworm, also known as "Tinea", is an infection of the skin, characterized by a reddish to brownish raised or bumpy patch of skin that may be lighter in the center, giving the appearance of a 'ring'. Contrary to its name, ringworm is not caused by a worm but by parasitic fungi (Dermatophytosis). It can exist anywhere on the body.
Fungi are tiny organisms that survive by eating plant or animal material, those that cause parasitic infection (dermatophytes) feed on keratin, the material found in the outer layer of skin, hair, and nails. These fungi thrive best on skin that is moist, hot, and hidden from the light. Together with the other dermatophytosis, up to 20 percent of the population has one of these infections at any given moment.
Transmission
Ringworm is very common, especially among children, and may be spread by skin-to-skin contact, as well as via contact with contaminated items such as hairbrushes or through the use of the same toilet seat as an infected individual. Ringworm spreads readily, as those infected are contagious even before they show symptoms of the disease. Participants in contact sports such as wrestling have a risk of contracting the fungal infection through skin-to-skin contact.
Ringworm is mildly contagious. Ringworm is also a common infection in domestic animals, especially farm animals, dogs and cats. Humans can contract ringworm from these animals as humans are in close contact with them. Chickens may also be a source, due to the dirty conditions in which many poultry must live in which ringworm may thrive. Ringworm can also be caught from other humans, both by direct contact and by prolonged contact with flakes of shed skin (from sharing clothes or from house dust, for instance).
To catch ringworm, you have to be exposed to it and you have to be susceptible. Some people are much more susceptible than others. Those with eczema or other skin problems get ringworm more easily because the protective barrier of the skin's outer layer is less intact. Children are more susceptible before puberty. Some people are genetically predisposed, and can get it easily throughout life.
Symptoms and diagnosis
The best known sign of ringworm in people is the appearance of one or more red raised itchy patches with defined edges, not unlike the herald rash of Pityriasis rosea. These patches are often lighter in the center, taking on the appearance of a ring. If the infected area involves the scalp or beard area, then bald patches may become evident. The affected area may become itchy for periods of time.
Doctors can diagnose ringworm on sight, or they may take a skin scraping, or in the case of animal ringworm or tinea capitis, examine plucked hairs for fungal elements. This is examined under a microscope, or put on an agar plate in a microbiology laboratory and allowed to grow. Some of the fungi fluoresce under a black light examination.
In domestic animals, ringworm can cause a variety of symptoms, but most cases show scaling and patches of hair loss. Some cats can be carriers, but show no symptoms.
Sometimes a ringworm infection may cause skin lesions in a part of the body that is remote from the actual infection. Such lesions are called "dermatophytids". The lesions themselves are fungus-free, and normally disappear upon treatment of the actual infection. The most common example is an eruption in the hands resulting from a fungus infection of the feet. Dermatophytids are essentially a generalized allergic reaction to the fungus.
-
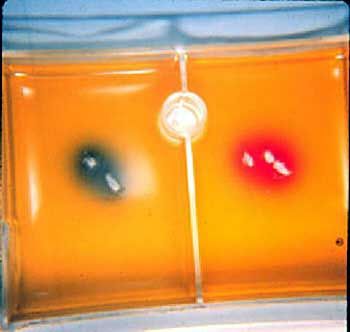
Plucked hair treated with KOH showing ectothrix spores and hyphae from a case of feline ringworm
-
Specialized agar plate, called Dermatophyte Test Medium is used to culture and identify ringworm organisms
-
Tinea corporis ringworm [1]
Differential diagnosis
Ringworm infection must be differentiated from other diseases presenting with an erythmatous, scaly, annular and pruritic rash. The differentials include the following:
| Name of superficial infection | Clinical presentation | Extension to hair follicle | Fungus(i) | Systemic disease | KOH preparations | Morphology in tissue sections |
|---|---|---|---|---|---|---|
| Tinea or ringworm | Round lesions with scaly border, accompanied by pruritis and burning | Yes; when suppurative known as kerion, when chronic known as Majocchi's granuloma | Dermatophytes (Epidermophyton spp., Trichophyton spp., Microsporum spp.) | Very rare but can invade the dermis and soft tissues, causing mycetomas | Hyphae with or without septations | Hyphae cannot be visualized in the keratin with H&E, special stains are needed |
| Tinea versicolor | Hypo and hyperpigmentation in patients with oily and sweaty skin, fine scales when scratching | Yes, known as Pityrosporum folliculits | Malassezia spp. | Systemic infections may occur in premature neonates receiving parenteral nutrition and in other immunosuppressed hosts | Yeasts and hyphae (“spaghetti and meat balls”) | Faintly basophilic hyphae in the stratum corneum |
| Tinea nigra | Brown to black macule, usually on palms, with some scaling | No | Phaeoannellomyces werneckii | Not described | Darkly pigmented, septated, and branching hyphae | Pigmented hyphae in the stratum corneum |
| White piedra | Creamy-white, small, soft nodules in hair shafts | No | Trichosporon spp. | Immunosuppressed patients may have lung infiltrates, renal involvement, and fungemia | Septate hyphae perpendicular to hair shaft | Not used for diagnosis |
| Black piedra | Hard dark nodules in hair shafts | No | Piedraia hortae | Not described | Collections of crescent ascospores surrounded by pigmented hyphae | Not used for diagnosis |
| Superficial candidiasis | Intertrigo, chronic paronychia, onychodystrophy, cheilitis | Yes | Candida spp. | Yes, particularly in patients with AIDS and depending on the level of immunosuppression | Yeasts, pseudohyphae may be observed | Fungal elements may be seen through the biopsy, vascular invasion must be determined |
Treatment
Topical antifungal drugs containing miconazole (Daktarin, Micatin & Monistat), clotrimazole, terbinafine (Lamisil), butenafine and tolnaftate (Tinactin), many available without a prescription, are used to clear up the infection. Pyrithione zinc, found in Head and Shoulders shampoo, is a very effective treatment for ringworm on the scalp and can be used as a body wash to assist in overall treatment.
On September 28, 2007, the U.S. Food and Drug Administration stated that Terbinafine (Lamisil by Novartis AG) is a new treatment approved for use by children aged 4 up. Antifungal granules can be sprinkled on a child's food to treat ringworm of the scalp, Tinea capitis.[2]
Treatment may be obstructed by itching, burning, cracking, and scaling that accompany this condition and prevent effective treatment. Ointments may be mixed with hydrocortisone creams such as Cortaid appear to reduce inflammation and speed recovery, but not always. Fungal infections may take a while to clear up, but most ringworm infections should see improvement in a week or two. Types affecting the nails or scalp are very difficult to treat due to fungal infection in follicle roots or under the nail itself.
Griseofulvin is a traditional drug used to treat ringworm in both animals and people. It can be very effective, but likely requires a prescription and may produce side effects. In cats and cattle, sulfurated lime rinses are often used to treat ringworm; and dilute povidone-iodine may be used as a wash in cattle. Enilconazole, as a rinse, is an effective ringworm treatment available in many countries for treating animals.
Lufenuron, the active ingredient in Program oral flea treatment, is also commonly prescribed by vets to treat ringworm infections in cats and dogs.
Folk remedies
Numerous folk remedies have been promoted for the treatment of Ringworm, many of them involving potentially dangerous caustic or acidic ingredients. These remedies generally take the approach of trying to burn away the fungal infection with mild acid preparations, soothing the symptoms with herbal poultices, or applying oils or drawing salves believed to have antibiotic or healing properties, such as tea tree oil. The efficacy of any of these traditional remedies cannot be assessed since they have not undergone rigorous clinical testing. Indeed, some may cause greater harm than the fungal infection they are intended to treat.
Prevention
Fungi thrive in warm, moist areas, such as locker rooms and swimming pools, and in skin folds. The fungi may be present without any symptoms. To prevent ringworm:
- Do not share clothing, sports equipment, towels, or sheets. If you think you have been exposed to ringworm, wash your clothes in hot water with fungus-killing (fungicidal) soap.
- Shower and shampoo thoroughly after any sport that requires skin-to-skin contact.
- Wrestlers should regularly inspect the skin before practice, use protective bandages over infections while practicing or avoid competition until 1 week after symptoms resolve, and thoroughly disinfect gym pads and equipment.
- Wear loose-fitting cotton clothing and change underwear at least once a day.
- Keep your skin clean and dry. Always dry yourself completely after showers or baths.
- Take your pet to the vet if it has patches of missing hair, which could be a sign of a fungal infection.
- Continue topical remedies for 2 to 4 weeks after symptoms have resolved.
See also
References
Additional Resource
- The Merck Manual, Twelfth Edition, 1972, p. 1451
External links
de:Hautpilz id:Kurap is:Hringskyrfi nl:Ringworm (schimmel) sv:Ringorm ur:داد

![Tinea corporis ringworm [1]](/images/5/5c/Tinea_corporis.jpg)