Human iron metabolism
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Iron is an essential element for most life on Earth, including human beings. The control of this necessary but potentially toxic substance is an important part of many aspects of human health and disease. Hematologists have been especially interested in the system of iron metabolism because iron is essential to red blood cells. In fact, most of the human body's iron is contained in red blood cells' hemoglobin, and iron-deficiency is the most common cause of anemia.
Understanding this system is also important for understanding diseases of iron overload.
Recent discoveries in the field have shed new light on how humans control the level of iron in their bodies. That has created new understanding of the mechanisms of several diseases.
Importance of iron regulation
Iron is an absolute requirement for most forms of life, including humans and most bacterial species. And because plants and animals all use iron, iron can be found in a wide variety of food sources.
Iron is essential to life, because of its unique ability to serve as both an electron donor and acceptor.
But iron can also be potentially toxic. Iron's ability to donate and accept electrons means that if iron is free within the cell, it can catalyze the conversion of hydrogen peroxide into free radicals. And free radicals can cause damage to a wide variety of cellular structures, and ultimately kill the cell. To prevent that kind of damage, all life forms that use iron bind the iron atoms to proteins. That allows the cells to use the benefits of iron, but also limit its ability to do harm. [2]
The most important group of iron-binding proteins are the heme molecules, all of which contain iron at their centers. Humans and most bacteria use variants of heme to carry out redox reactions and electron transport processes. These reactions and processes are required for oxidative phosphorylation. That process is the principal source of energy for human cells; without it, our cells would die.
Humans also use iron in the hemoglobin of red blood cells, in order to transport oxygen from the lungs to the tissues and to export carbon dioxide back to the lungs. And iron is an essential component of myoglobin to store oxygen in muscle cells.
The human body needs iron for oxygen transport. That oxygen is required for the production and survival of all cells in our bodies. So human bodies tightly regulate iron absorption and recycling. Iron is such an essential element of human life, in fact, that humans have no physiologic regulatory mechanism for excreting iron. Most humans prevent iron overload solely by regulating iron absorption. Those who can't regulate absorption well enough get disorders of iron overload. In these diseases, the toxicity of iron starts overwhelming the body's ability to bind and store it. [3]
Body iron stores
Most well-nourished people in industrialized countries have 3-4 grams of iron in their bodies. Of this, about 2.5 g is contained in the hemoglobin needed to carry oxygen through the blood. Another 400 mg is devoted to cellular proteins that use iron for important cellular processes like storing oxygen (myoglobin), or performing energy-producing redox reactions (cytochromes). 3-4 mg circulates through the plasma, bound to transferrin. [4]
Since so much iron is required for hemoglobin, iron deficiency anemia is the first and primary clinical manifestation of iron deficiency. Oxygen transport is so important to human life that severe anemia harms or kills people by depriving their organs of enough oxygen. So iron-deficient people will suffer or die from organ damage well before cells run out of the iron needed for intracellular processes like electron transport.
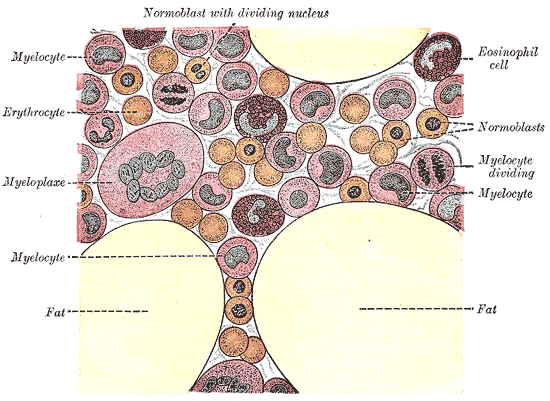
Some iron in the body is stored. Physiologically, most stored iron is bound by ferritin molecules; the largest amount of ferritin-bound iron is found in cells of the liver hepatocytes, the bone marrow and the spleen. The liver's stores of ferritin are the primary physiologic source of reserve iron in the body.
Macrophages of the reticuloendothelial system store iron as part of the process of breaking down and processing hemoglobin from engulfed red blood cells.
Iron is also stored in hemosiderin in an apparently pathologic process. This molecule appears to be mainly the result of cell damage. It is often found engulfed by macrophages that are scavenging regions of damage. It can also be found among people with iron overload due to frequent blood cell destruction and transfusions.
Men tend to have more stored iron than women, particularly women who must use their stores to compensate for iron lost through menstruation, pregnancy or lactation.
How the body gets its iron
Most of the iron in the body is hoarded and recycled by the reticuloendothelial system which breaks down aged red blood cells. However, people lose a small but steady amount by sweating and by shedding cells of the skin and the mucosal lining of the gastrointestinal tract. The total amount of loss for healthy people in the developed world amounts to an estimated average of 1 mg a day for men, and 1.5–2 mg a day for women with regular menstrual periods. People in developing countries with gastrointestinal parasitic infections often lose more. [5]
This steady loss means that people must continue to absorb iron. They do so via a tightly regulated process that under normal circumstances protects against iron overload.
Absorbing iron from the diet
Like most mineral nutrients, iron from digested food or supplements is almost entirely absorbed in the duodenum by enterocytes of the duodenal lining. These cells have special molecules that allow them to move iron into the body.
To be absorbed, dietary iron must be in its ferrous Fe2+ form. A ferric reductase enzyme on the enterocytes' brush border, Dcytb, reduces ferric Fe3+ to Fe2+. A protein called divalent metal transporter 1 DMT1, which transports all kinds of divalent metals into the body, then transports the iron across the enterocyte's cell membrane and into the cell.
These intestinal lining cells can then either store the iron as ferritin (in which case the iron will leave the body when the cell dies and is sloughed off into feces) or the cell can move it into the rest of the body, using a protein called ferroportin. The body regulates iron levels by regulating each of these steps. For instance, cells produce more Dcytb, DMT1 and ferroportin in response to iron deficiency anemia. [6]
Our bodies' rates of iron absorption appear to respond to a variety of interdependent factors, including total iron stores, the extent to which the bone marrow is producing new red blood cells, the concentration of hemoglobin in the blood, and the oxygen content of the blood. We also absorb less iron during times of inflammation. In fact, recent discoveries demonstrate that hepcidin regulation of ferroportin (see below) is responsible for the syndrome of anemia of chronic disease.
While Dcytb and DMT1 are unique to iron transport across the duodenum, ferroportin is distributed throughout the body on all cells which store iron. Thus, regulation of ferroportin is the body's main way of regulating the amount of iron in circulation.
Reasons for iron deficiency
Functional or actual iron deficiency can result from a variety of causes, explained in more detail in the article dedicated to this topic. These causes can be grouped into several categories:
- Increased demand for iron, which the diet can't accommodate.
- Increased loss of iron (usually through loss of blood).
- Nutritional deficiency. This can either be the result of failure to eat iron-containing foods, or eating a diet heavy in food that reduces the absorption of iron, or both.
- Inability to absorb iron because of damage to the intestinal lining. Examples of causes of this kind of damage include surgery involving the duodenum, or diseases like Crohn's or celiac sprue which severely reduce the surface area available for absorption.
- Inflammation leading to hepcidin-induced restriction on iron release from enterocytes (see below).
The possibility of too much iron
The body is able to substantially reduce the amount of iron it absorbs across the mucosa. But it does not seem to be able to entirely shut down the iron transport process. Also, in situations where excess iron damages the intestinal lining itself (for instance, when children eat a large quantity of iron tablets produced for adult consumption), even more iron can enter the bloodstream and cause a potentially deadly syndrome of iron intoxication. Large amounts of free iron in the circulation will cause damage to critical cells in the liver, the heart and other metabolically active organs.
Iron toxicity results when the amount of circulating iron exceeds the amount of transferrin available to bind it. But the body is able to vigorously regulate its iron uptake. So frank iron toxicity from ingestion is usually the result of extraordinary circumstances like iron tablet overdose[7] rather than variations in diet. Iron toxicity is usually the result of more chronic iron overload syndromes associated with genetic diseases, repeated transfusions or other causes.
How cells get their iron from the body
As discussed above, most of the iron in the body is located on hemoglobin molecules of red blood cells. When red blood cells reach a certain age, they are degraded and engulfed by specialized scavenging macrophages. These cells internalize the iron-containing hemoglobin, degrade it, put the iron onto transferrin molecules, and then export the transferrin-iron complexes back out into the blood. Most of the iron used for blood cell production comes from this cycle of hemoglobin recycling.
But all cells use some iron. That means they must somehow get it from the circulating blood. Since iron is tightly bound to transferrin, cells throughout the body have receptors for transferrin-iron complexes on their surfaces. These receptors engulf and internalize both the protein and the iron attached to it. Once inside, the cell transfers the iron to ferritin, the internal iron storage molecule.
Cells have advanced mechanisms for sensing their own need for iron. In human cells, the best characterized iron-sensing mechanism is the result of post-transcriptional regulation of mRNA (the chemical instructions derived from DNA genes to make proteins). Sequences of mRNA called iron responsive elements (IREs) are contained within the mRNA sequences that code for transferrin receptors and for ferritin. Iron responsive element binding protein (IRE-BP) binds to these mRNA sequences. On its own, the IRE-BP binds to the IREs of ferritin and transferrin receptor mRNA. But when iron binds to the IRE-BP, the IRE-BP changes shape with the result that the IRE-BPs can no longer bind the ferritin mRNA. This liberates the mRNA to direct the cell to make more ferritin. In other words, when there is high iron in the cell, the iron itself causes the cell to produce more iron storage molecules. (The IRE-BP is an aconitase; for a schematic drawing of the shape change, see here).
Transferrin receptor production depends on a similar mechanism. But this one has the opposite trigger, and the opposite ultimate effect. IRE-BPs without iron bind to the IREs on transferrin receptor mRNA. But those IREs have a different effect: when the IRE-BP binds to these sites, the binding not only allows for transcription but also stabilizes the mRNA molecule so it can stay intact for longer.
So in low-iron conditions, IRE-BPs allow the cell to keep producing transferrin receptors. And more transferrin receptors make it easier for the cell to bring in more iron from transferrin-iron complexes circulating outside the cell. But as iron binds to more and more IRE-BPs, they change shape and unbind the transferrin receptor mRNA. The transferrin receptor mRNA is rapidly degraded without the IRE-BP attached to it. The cell stops producing transferrin receptors.
When the cell has obtained more iron than it can bind up with ferritin or heme molecules, more and more iron will bind to the IRE-BPs. That will stop transferrin receptor production. And iron-IRE-BP binding will also start ferritin production.
When the cell is low on iron, less and less iron will bind to IRE-BPs. The IRE-BPs without iron will bind to transferrin receptor mRNA. Transferrin receptor production will increase, and ferritin production will decrease. [8]
Regulation of circulating iron levels
Iron is too toxic to simply leave iron uptake up to the cells that might or might not need it. The body needs to control the amount of iron that circulates as well. As discussed above, ferroportin transport regulates the amount of iron that leaves the duodenal enterocytes and goes into the circulation. Ferroportin is also found in the iron-storing cells of the liver and in iron-storing macrophages. Ferroportin, in turn, is regulated by hepcidin. Hepcidin stops ferroportin from releasing iron into the rest of the body. So a high level of hepcidin will cause a low amount of circulating iron (by preventing ferroportin from releasing the iron), while a low level will cause a high amount of circulating iron.
The discovery of hepcidin, a peptide hormone secreted by the liver, appears to be a profound breakthrough in the understanding of iron metabolism, since it appears to be the long-pursued master regulator of iron homeostasis. (The story of the discovery of hepcidin and its role in iron metabolism is told at the hepcidin article.)

Current understanding of this system offers two explanations for why tight control of iron levels is important to human health. First, discussed above, is the need to protect against the possible toxicity of iron. The second is as a strategy to defend against bacterial infection. As explained above, most forms of life on Earth depend on iron to catalyze biochemical reactions that are necessary for life. This is as true for bacteria that cause human disease as it is for human cells.
If bacteria are to survive, then, they must get iron from the environment. Disease-causing bacteria do this in many ways, including releasing iron-binding molecules called siderophores and then reabsorbing them to recover iron, or scavenging iron from hemoglobin and transferrin. But the harder they have to work to get iron, the greater a metabolic price they must pay. That means that iron-deprived bacteria reproduce more slowly. So our control of iron levels appears to be an important defense against bacterial infection. And people with increased amounts of iron, like people with hemochromatosis, are more susceptible to bacterial infection. [9]
However, although this mechanism is an elegant response to short-term bacterial infection, it can cause problems when inflammation goes on for longer. Since the liver produces hepcidin in response to inflammatory cytokines, hepcidin levels can increase as the result of non-bacterial sources of inflammation, like viral infection, cancer, auto-immune diseases or other chronic diseases. When this occurs, the sequestration of iron appears to be the major cause of the syndrome of anemia of chronic disease, in which not enough iron is available to produce an adequate number of hemoglobin-containing red blood cells. [10]
Diseases of iron regulation
The discovery of hepcidin has shed a great deal of light on the basic workings of iron regulation. A recent review by Clara Camaschella [11] suggests that by understanding this master regulator of the iron regulation system, many other molecular elements of the system will soon become easier to understand. For instance, a severe form of iron overload, juvenile hemochromatosis, is now understood to be the result of severe hepcidin deficiency.
Indeed, as Camaschella's review suggests, if hepcidin is the master regulator, most genetic forms of iron overload can be thought of as relative hepcidin deficiency in one way or another. The exceptions, people who have mutations in the gene for ferroportin, prove the rule: these people have plenty of hepcidin, but their cells lack the proper response to it. So, in people with ferroportin proteins that transport iron out of cells without responding to hepcidin's signals to stop, they have a deficiency in the action of hepcidin, if not in hepcidin itself.
But the exact mechanisms of most of the various forms of adult hemochromatosis, which make up most of the genetic iron overload disorders, remain unsolved. So while researchers have been able to identify genetic mutations causing several adult variants of hemochromatosis, they now must turn their attention to the normal function of these mutated genes.
These genes represent multiple steps along the pathway of iron regulation, from the body's ability to sense iron, to the body's ability to regulate uptake and storage. Working out the functions of each gene in this pathway will be an important tool for finding new methods of treating genetic disorders, as well as for understanding the basic workings of the pathway.
So though many mysteries of iron metabolism remain, the discovery of hepcidin already allows a much better understanding of the nature of iron regulation, and makes researchers optimistic that many more breakthroughs in this field are soon to come.
References
- ^ Andrews NC. Disorders of iron metabolism. New England Journal of Medicine. 341(26):1986-1995. December 23, 1999. Also, see related correspondence, published in NEJM 342(17):1293-1294, Apr 27, 2000.
- ^ Schrier SL and Bacon BR. Iron overload syndromes other than hereditary hematochromatosis. Up-to-Date (Subscription required). Accessed December 2005.
- ^ Schrier SL. Regulation of iron balance. Up-to-Date (Subscription required). Accessed December 2005.
- ^ Andrews NC. Disorders of iron metabolism. New England Journal of Medicine. Related correspondence, published in NEJM 342(17):1293-1294, Apr 27, 2000.
- ^ Fleming RE and Bacon BR. Orchestration of iron homeostasis. New England Journal of Medicine. 352(17):1741-1744. April 28, 2005.
- ^ Baker MD. Major trauma in children. Rudolph's Pediatrics, 21st Ed. McGraw-Hill. 2003.
- ^ Berg J. Tymoczko, JL; Stryer, L. Biochemistry. 5th Ed. WF Freeman & Co. 2001. (Hosted on the web by the National Library of Medicine.)
- ^ Ganz T. Hepcidin, a key regulator of iron metabolism and mediator of anemia of inflammation. Blood 102(3): 783-788. 1 Aug 2003.
- ^ Andrews NC. Anemia of inflammation: the cytokine-hepcidin link. J Clin Invest 113(9):1251-3. May 2004.
- ^ Camaschella C. Understanding iron homeostasis through genetic analysis of hemochromatosis and related disorders. Blood 106(12):3710-3717, 1 December 2005.