Eravacycline
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Eravacycline is a tetracycline class antibacterial that is FDA approved for the treatment of complicated intra‑abdominal infections in patients 18 years of age and older. Common adverse reactions include infusion site reactions, nausea, and vomiting.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Eravacycline is indicated for the treatment of complicated intra‑abdominal infections (cIAI) caused by susceptible microorganisms: Escherichia coli, Klebsiella pneumoniae, Citrobacter freundii, Enterobacter cloacae, Klebsiella oxytoca, Enterococcus faecalis, Enterococcus faecium, Staphylococcus aureus, Streptococcus anginosus group, Clostridium perfringens, Bacteroides species, and Parabacteroides distasonis in patients 18 years or older.
Limitations of Use
- Eravacycline is not indicated for the treatment of complicated urinary tract infections (cUTI).
Dosage
- The recommended dose regimen of eravacycline is 1 mg/kg every 12 hours. Administer intravenous infusions of eravacycline over approximately 60 minutes every 12 hours.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding eravacycline Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding eravacycline Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of eravacycline in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding eravacycline Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding eravacycline Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Eravacycline is contraindicated for use in patients with known hypersensitivity to eravacycline, tetracycline-class antibacterial drugs, or to any of the excipients.
Warnings
Hypersensitivity Reactions
- Life-threatening hypersensitivity (anaphylactic) reactions have been reported with eravacycline. Eravacycline is structurally similar to other tetracycline-class antibacterial drugs and should be avoided in patients with known hypersensitivity to tetracycline-class antibacterial drugs. Discontinue eravacycline if an allergic reaction occurs.
Tooth Discoloration and Enamel Hypoplasia
- The use of eravacycline during tooth development (last half of pregnancy, infancy and childhood to the age of 8 years) may cause permanent discoloration of the teeth (yellow-grey-brown). This adverse reaction is more common during long-term use of the tetracycline class drugs, but it has been observed following repeated short-term courses. Enamel hypoplasia has also been reported with tetracycline class drugs. Advise the patient of the potential risk to the fetus if eravacycline is used during the second or third trimester of pregnancy.
Inhibition of Bone Growth
- The use of eravacycline during the second and third trimester of pregnancy, infancy and childhood up to the age of 8 years may cause reversible inhibition of bone growth. All tetracyclines form a stable calcium complex in any bone-forming tissue. A decrease in fibula growth rate has been observed in premature infants given oral tetracycline in doses of 25 mg/kg every 6 hours. This reaction was shown to be reversible when the drug was discontinued. Advise the patient of the potential risk to the fetus if eravacycline is used during the second or third trimester of pregnancy.
Clostridium difficile-Associated Diarrhea
- Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
- C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
- If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial drug treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Tetracycline Class Adverse Reactions
- Eravacycline is structurally similar to tetracycline-class antibacterial drugs and may have similar adverse reactions. Adverse reactions including photosensitivity, pseudotumor cerebri, and anti‑anabolic action which has led to increased BUN, azotemia, acidosis, hyperphosphatemia, pancreatitis, and abnormal liver function tests, have been reported for other tetracycline-class antibacterial drugs, and may occur with eravacycline. Discontinue eravacycline if any of these adverse reactions are suspected.
Potential for Microbial Overgrowth
- Eravacycline use may result in overgrowth of non-susceptible organisms, including fungi. If such infections occur, discontinue eravacycline and institute appropriate therapy.
Development of Drug-Resistant Bacteria
- Prescribing eravacycline in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Eravacycline was evaluated in 3 active-controlled clinical trials (Trial 1, Trial 2 and Trial 3) in adults with cIAI. These trials included two Phase 3 trials (Trial 1and Trial 2) and one Phase 2 trial (Trial 3, NCT01265784). The Phase 3 trials included 520 patients treated with eravacycline and 517 patients treated with comparator antibacterial drugs (ertapenem or meropenem). The median age of patients treated with eravacycline was 56 years, ranging between 18 and 93 years old; 30% were age 65 years and older. Patients treated with eravacycline were predominantly male (57%) and Caucasian (98%). The eravacycline- treated population included 31% obese patients (BMI ≥ 30 kg/m2) and 8% with baseline moderate to severe renal impairment (calculated creatinine clearance 15 to less than 60 mL/min). Among the trials, 66 (13%) of patients had baseline moderate hepatic impairment (Child Pugh B); patients with severe hepatic impairment (Child Pugh C) were excluded from the trials.
Adverse Reactions Leading to Discontinuation
- Treatment discontinuation due to an adverse reaction occurred in 2% (11/520) of patients receiving eravacycline and 2% (11/517) of patients receiving the comparator. The most commonly reported adverse reactions leading to discontinuation of eravacycline were related to gastrointestinal disorders.
Most Common Adverse Reactions
- Adverse reactions occurring at 3% or greater in patients receiving eravacycline were infusion site reactions, nausea, and vomiting.
- Table 1 lists adverse reactions occurring in ≥ 1% of patients receiving eravacycline and with incidences greater than the comparator in the Phase 3 cIAI clinical trials. A similar adverse reaction profile was observed in the Phase 2 cIAI clinical trial (Trial 3).

Other Adverse Reactions of Eravacycline
- The following selected adverse reactions were reported in eravacycline-treated patients at a rate of less than 1% in the Phase 3 trials:
- Cardiac disorders: palpitations
- Gastrointestinal System: acute pancreatitis, pancreatic necrosis
- General Disorders and Administrative Site Conditions: chest pain
- Immune system disorders: hypersensitivity
- Laboratory Investigations: increased amylase, increased lipase, increased alanine aminotransferase, prolonged activated partial thromboplastin time, decreased renal clearance of creatinine, increased gamma-glutamyltransferase, decreased white blood cell count, neutropenia
- Metabolism and nutrition disorders: hypocalcemia
- Nervous System: dizziness, dysgeusia
- Psychiatric disorders: anxiety, insomnia, depression
- Respiratory, Thoracic, and Mediastinal System: pleural effusion, dyspnea
- Skin and subcutaneous tissue disorders: rash, hyperhidrosis
Postmarketing Experience
There is limited information regarding Eravacycline Postmarketing Experience in the drug label.
Drug Interactions
Effect of Strong CYP3A Inducers on Eravacycline
- Concomitant use of strong CYP3A inducers decreases the exposure of eravacycline, which may reduce the efficacy of eravacycline. Increase eravacycline dose in patients with concomitant use of a strong CYP3A inducer.
Anticoagulant Drugs
- Because tetracyclines have been shown to depress plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- Eravacycline, like other tetracycline-class antibacterial drugs, may cause discoloration of deciduous teeth and reversible inhibition of bone growth when administered during the second and third trimester of pregnancy. The limited available data with eravacycline use in pregnant women are insufficient to inform drug‑associated risk of major birth defects and miscarriages. Animal studies indicate that eravacycline crosses the placenta and is found in fetal plasma; doses greater than approximately 3- and 2.8- times the clinical exposure, based on AUC in rats and rabbits, respectively, administered during the period of organogenesis, were associated with decreased ossification, decreased fetal body weight, and/or increased post-implantation loss.
- The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Animal Data
- Embryo-fetal development studies in rats and rabbits reported no treatment-related effects at approximately 3 and 2.8 times the clinical exposure (based on AUC). Dosing was during the period of organogenesis, i.e. gestation days 7-17 in rats and gestation days 7-19 in rabbits. Higher doses, approximately 8.6 and 6.3 times the clinical exposure (based on AUC) in rats and rabbits, respectively, were associated with fetal effects including increased post-implantation loss, reduced fetal body weights, and delays in skeletal ossification in both species, and abortion in the rabbit.
- A peri-natal and post-natal rat toxicity study demonstrated that eravacycline crosses the placenta and is found in fetal plasma following intravenous administration to the dams. This study did not demonstrate anatomical malformations, but there were early decreases in pup weight that were later comparable to controls and a non-significant trend toward increased stillbirths or dead pups during lactation. F1 males from dams treated with 10 mg/kg/day eravacycline that continued to fertility testing had decreased testis and epididymis weights at approximately Post-Natal Day 111 that may have been at least partially related to lower body weights in this group.
- tetracyclines cross the placenta, are found in fetal tissues, and can have toxic effects on the developing fetus (often related to retardation of skeletal development). Evidence of embryotoxicity also has been noted in animals treated early in pregnancy.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Eravacycline in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Eravacycline during labor and delivery.
Nursing Mothers
Risk Summary
- It is not known whether eravacycline is excreted in human breast milk. Eravacycline (and its metabolites) is excreted in the milk of lactating rats. tetracyclines are excreted in human milk; however, the extent of absorption of tetracyclines, including eravacycline, by the breastfed infant is not known. There are no data on the effects of eravacycline on the breastfed infant, or the effects on milk production. Because there are other antibacterial drug options available to treat cIAI in lactating women and because of the potential for serious adverse reactions, including tooth discoloration and inhibition of bone growth, advise patients that breastfeeding is not recommended during treatment with eravacycline and for 4 days (based on half-life) after the last dose.
Animal Data
- Eravacycline (and its metabolites) was excreted in the milk of lactating rats on post-natal day 15 following intravenous administration of 3, 5, and 10 mg/kg/day eravacycline.
Pediatric Use
- The safety and effectiveness of eravacycline in pediatric patients have not been established.
- Due to the adverse effects of the tetracycline-class of drugs, including eravacycline on tooth development and bone growth, use of eravacycline in pediatric patients less than 8 years of age is not recommended.
Geriatic Use
- Of the total number of patients with cIAI who received eravacycline in Phase 3 clinical trials (n = 520), 158 subjects were ≥ 65 years of age, while 59 subjects were ≥ 75 years of age. No overall differences in safety or efficacy were observed between these subjects and younger subjects.
- No clinically relevant differences in the pharmacokinetics of eravacycline were observed with respect to age in a population pharmacokinetic analysis of eravacycline.
Gender
There is no FDA guidance on the use of Eravacycline with respect to specific gender populations.
Race
There is no FDA guidance on the use of Eravacycline with respect to specific racial populations.
Renal Impairment
- No dosage adjustment is necessary for eravacycline in patients with renal impairment.
Hepatic Impairment
- No dosage adjustment is warranted for eravacycline in patients with mild to moderate hepatic impairment (Child Pugh A and Child Pugh B). Adjust eravacycline dosage in patients with severe hepatic impairment (Child Pugh C).
Females of Reproductive Potential and Males
Infertility
- Based on animal studies, eravacycline can lead to impaired spermiation and sperm maturation, resulting in abnormal sperm morphology and poor motility. The effect is reversible in rats. The long-term effects of eravacycline on male fertility have not been studied.
Immunocompromised Patients
There is no FDA guidance one the use of Eravacycline in patients who are immunocompromised.
Administration and Monitoring
Administration
Recommended Adult Dosage
- The recommended dose regimen of eravacycline is 1 mg/kg every 12 hours. Administer intravenous infusions of eravacycline over approximately 60 minutes every 12 hours.
- The recommended duration of treatment with eravacycline for cIAI is 4 to 14 days. The duration of therapy should be guided by the severity and location of infection and the patient’s clinical response.
Dosage Modifications in Patients with Hepatic Impairment
- In patients with severe hepatic impairment (Child Pugh C), administer eravacycline 1 mg/kg every 12 hours on Day 1 followed by eravacycline 1 mg/kg every 24 hours starting on Day 2 for a total duration of 4 to 14 days. No dosage adjustment is warranted in patients with mild to moderate hepatic impairment (Child Pugh A and Child Pugh B).
Dosage Modifications in Patients with Concomitant Use of a Strong Cytochrome P450 Isoenzymes (CYP) 3A Inducer
- With concomitant use of a strong CYP3A inducer, administer eravacycline 1.5 mg/kg every 12 hours for a total duration of 4 to 14 days. No dosage adjustment is warranted in patients with concomitant use of a weak or moderate CYP3A inducer.
Preparation and Administration
- Eravacycline is for intravenous infusion only. Each vial is for a single dose only.
Preparation
- Eravacycline is supplied as a sterile yellow to orange dry powder in a single-dose vial that must be reconstituted and further diluted prior to intravenous infusion as outlined below. Eravacycline does not contain preservatives. Aseptic technique must be used for reconstitution and dilution as follows:
- Calculate the dose of eravacycline based on the patient weight; 1 mg/kg actual body weight. Prepare the required dose for intravenous infusion, by reconstituting the appropriate number of vials needed. Reconstitute each vial of eravacycline with 5 mL of Sterile Water for Injection, USP. When the eravacycline vial content is reconstituted with 5 mL sterile Water for Injection, USP it will deliver 50 mg (10 mg/mL) of eravacycline (free base equivalents).
- Swirl the vial gently until the powder has dissolved entirely. Avoid shaking or rapid movement as it may cause foaming. The reconstituted eravacycline solution should be a clear, pale yellow to orange solution. Do not use the solution if you notice any particles or the solution is cloudy. Reconstituted solution is not for direct injection.
- The reconstituted eravacycline solution is further diluted for intravenous infusion to a target concentration of 0.3 mg/mL, in a 0.9% Sodium Chloride Injection, USP infusion bag before intravenous infusion. To dilute the reconstituted solution, withdraw the full or partial reconstituted vial content from each vial and add it into the infusion bag to generate an infusion solution with a target concentration of 0.3 mg/mL (within a range of 0.2 to 0.6 mg/mL). Do not shake the bag.
- The reconstituted and diluted solutions must be infused within 6 hours if stored at room temperature (not to exceed 25°C/77°F) or within 24 hours if stored refrigerated at 2 °C to 8 °C (36 °F to 46 °F). Reconstituted eravacycline solutions and diluted eravacycline infusion solutions should not be frozen.
- Visually inspect the diluted eravacycline solution for particulate matter and discoloration prior to administration (the eravacycline infusion solution for administration is clear and ranges from light yellow to orange). Discard unused portions of the reconstituted and diluted solution.
Administration of the Intravenous Infusion
- The diluted eravacycline solution is administered as an intravenous infusion over approximately 60 minutes.
- Eravacycline may be administered intravenously through a dedicated line or through a Y-site. If the same intravenous line is used for sequential infusion of several drugs, the line should be flushed before and after infusion of eravacycline with 0.9% Sodium Chloride Injection, USP.
Drug Compatibilities
- Eravacycline is compatible with 0.9% Sodium Chloride Injection, USP. The compatibility of eravacycline with other drugs and infusion solutions has not been established. Eravacycline should not be mixed with other drugs or added to solutions containing other drugs.
Monitoring
There is limited information regarding Eravacycline Monitoring in the drug label.
IV Compatibility
- Eravacycline is indicated for intravenous use.
Overdosage
- No reports of overdose were reported in clinical trials. In the case of suspected overdose, eravacycline should be discontinued and the patient monitored for adverse reactions. Hemodialysis is not expected to remove significant quantities of eravacycline.
Pharmacology
Template:Chembox E numberTemplate:Chembox Pharmacology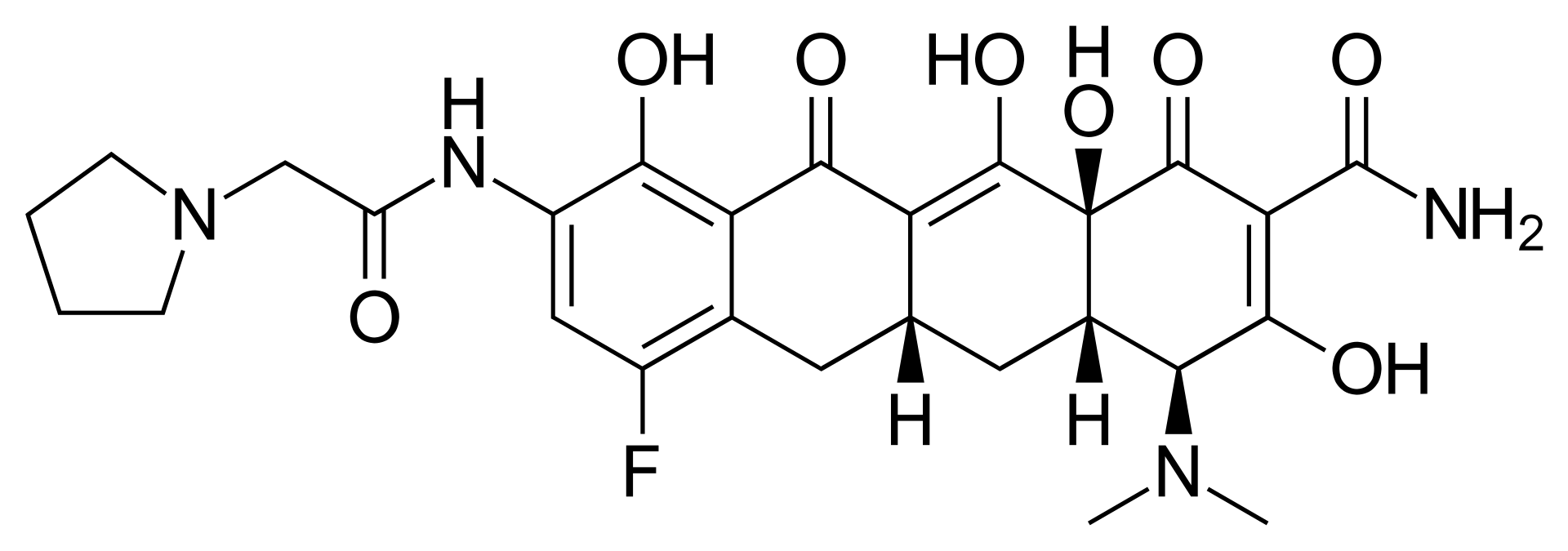
| |
| Names | |
|---|---|
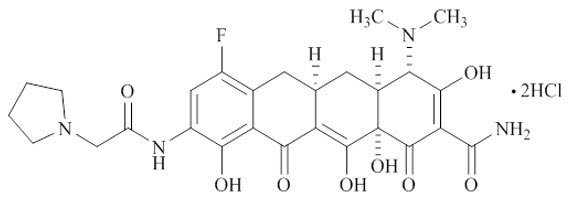
| IUPAC name
(4S,4aS,5aR,12aS)-4-(Dimethylamino)-7-fluoro-3,10,12,12a-tetrahydroxy-1,11-dioxo-9-[(1-pyrrolidinylacetyl)amino]-1,4,4a,5,5a,6,11,12a-octahydro-2-tetracenecarboxamide
| |
| Other names
Xerava
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChemSpider | |
| ECHA InfoCard | Lua error in Module:Wikidata at line 879: attempt to index field 'wikibase' (a nil value). Lua error in Module:Wikidata at line 879: attempt to index field 'wikibase' (a nil value). |
| KEGG | |
PubChem CID
|
|
| |
| |
| Properties | |
| C27H31FN4O8 | |
| Molar mass | 558.555 |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Mechanism of Action
- Eravacycline is an antibacterial drug.
Structure
- The molecular formula for eravacycline dihydrochloride is C27H31FN4O8•2HCl, and its molecular weight is 631.5.
- The following represents the chemical structure of eravacycline dihydrochloride:
Pharmacodynamics
- The AUC divided by the MIC of eravacycline has been shown to be the best predictor of activity. Based on the flat exposure-response relationship observed in clinical studies, eravacycline exposure achieved with the recommended dosage regimen appears to be on the plateau of the exposure-response curve.
Cardiac Electrophysiology
- The effect of eravacycline on the QTc interval was evaluated in a Phase 1 randomized, placebo and positive controlled, double-blind, single-dose, crossover thorough QTc study in 60 healthy adult subjects. At the 1.5 mg/kg single dose (1.5 times the maximum approved recommended dose), eravacycline did not prolong the QTc interval to any clinically relevant extent.
Pharmacokinetics
- Following single-dose intravenous administration, eravacycline AUC and Cmax increase approximately dose-proportionally over doses from 1 mg/kg to 3 mg/kg (3 times the approved dose).
- The mean exposure of eravacycline after single and multiple intravenous infusions (approximately 60 minutes) of 1 mg/kg administered to healthy adults every 12 hours is presented in Table 2.
- There is approximately 45% accumulation following intravenous dosing of 1 mg/kg every 12 hours.

Distribution
- Protein binding of eravacycline to human plasma proteins increases with increasing plasma concentrations, with 79% to 90% (bound) at plasma concentrations ranging from 100 to 10,000 ng/mL. The volume of distribution at steady-state is approximately 321 L.
Elimination
- The mean elimination half-life is 20 hours.
Metabolism
- Eravacycline is metabolized primarily by CYP3A4- and FMO-mediated oxidation.
Excretion
- Following a single intravenous dose of radiolabeled eravacycline 60 mg, approximately 34% of the dose is excreted in urine and 47% in feces as unchanged eravacycline (20% in urine and 17% in feces) and metabolites.
Specific Populations
- No clinically significant differences in the pharmacokinetics of eravacycline were observed based on age (18-86 years), sex, and race.
Patients with Renal Impairment
- The geometric least square mean Cmax for eravacycline was increased by 8.8% for subjects with end stage renal disease (ESRD) versus healthy subjects with 90% CI -19.4, 45.2. The geometric least square mean AUC0-inf for eravacycline was decreased by 4.0% for subjects with ESRD versus healthy subjects with 90% CI -14.0, 12.3.
Patients with Hepatic Impairment
- Eravacycline Cmax was 13.9%, 16.3%, and 19.7% higher in subjects with mild (Child-Pugh Class A), moderate (Child-Pugh Class B), and severe (Child‑Pugh Class C) hepatic impairment versus healthy subjects, respectively. Eravacycline AUC0-inf was 22.9%, 37.9%, and 110.3% higher in subjects with mild, moderate, and severe hepatic impairment versus healthy subjects, respectively.
Drug Interaction Studies
Clinical Studies
- Concomitant use of rifampin (strong CYP3A4/3A5 inducer) decreased eravacycline AUC by 35% and increased eravacycline clearance by 54%.
- Concomitant use of itraconazole (strong CYP3A inhibitor) increased eravacycline Cmax by 5% and AUC by 32%, and decreased eravacycline clearance by 32%.
In Vitro Studies
- Eravacycline is not an inhibitor of CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5. Eravacycline is not an inducer of CYP1A2, 2B6, or 3A4.
- Eravacycline is not a substrate for P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), bile salt export pump (BSEP), organic anion transporter peptide (OATP)1B1, OATP1B3, organic ion transporter (OAT)1, OAT3, OCT1, OCT2, multidrug and toxin extrusion (protein) (MATE)1, or MATE2-K transporters.
- Eravacycline is not an inhibitor of BCRP, BSEP, OATP1B1, OATP1B3, OAT1, OAT3, OCT1, OCT2, MATE1, or MATE2-K transporters.
Microbiology
Mechanism of Action
- Eravacycline is a fluorocycline antibacterial within the tetracycline class of antibacterial drugs. Eravacycline disrupts bacterial protein synthesis by binding to the 30S ribosomal subunit thus preventing the incorporation of amino acid residues into elongating peptide chains.
- In general, eravacycline is bacteriostatic against gram-positive bacteria (e.g., Staphylococcus aureus and Enterococcus faecalis); however, in vitro bactericidal activity has been demonstrated against certain strains of Escherichia coli, Klebsiella pneumoniae.
Resistance
- Eravacycline resistance in some bacteria is associated with upregulated, non-specific intrinsic multidrug-resistant (MDR) efflux, and target-site modifications such as to the 16s rRNA or certain 30S ribosomal proteins (e.g., S10).
- The C7 and C9 substitutions in eravacycline are not present in any naturally occurring or semisynthetic tetracyclines and the substitution pattern imparts microbiological activities including in vitro activity against gram-positive and gram-negative strains expressing certain tetracycline-specific resistance mechanism(s) [i.e., efflux mediated by tet(A), tet(B), and tet(K); ribosomal protection as encoded by tet(M) and tet(Q)].
- Activity of eravacycline was demonstrated in vitro against Enterobacteriaceae in the presence of certain beta-lactamases, including extended spectrum β-lactamases, and AmpC. However, some beta-lactamase-producing isolates may confer resistance to eravacycline via other resistance mechanisms.
- The overall frequency of spontaneous mutants in the gram-positive organisms tested was in the range of 10-9 to 10-10 at 4 times the eravacycline Minimum Inhibitory Concentration (MIC). Multistep selection of gram-negative strains resulted in a 16- to 32-times increase in eravacycline MIC for one isolate of Escherichia coli and Klebsiella pneumoniae, respectively. The frequency of spontaneous mutations in K. pneumoniae was 10-7 to 10‑8 at 4 times the eravacycline MIC.
Interaction with Other Antimicrobials
- In vitro studies have not demonstrated antagonism between eravacycline and other commonly used antibacterial drugs for the indicated pathogens.
Antimicrobial Activity
- Eravacycline has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections:
- Aerobic bacteria
- Anaerobic bacteria
- Gram-positive bacteria
- Gram-negative bacteria
- Bacteroides caccae
- Bacteroides fragilis
- Bacteroides ovatus
- Bacteroides thetaiotaomicron
- Bacteroides uniformis
- Bacteroides vulgatus
- Parabacteroides distasonis
- The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for eravacycline against isolates of similar genus or organism group. However, the efficacy of eravacycline in treating clinical infections caused by these bacteria has not been established in adequate and well-controlled clinical trials.
Susceptibility Test Methods
- For specific information regarding susceptibility test interpretive criteria, and associated test methods and quality control standards recognized by FDA for this drug, please see https://www.fda.gov/STIC.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies with eravacycline have not been conducted. However, there has been evidence of oncogenic activity in rats in studies with the related antibacterial drugs, oxytetracycline (adrenal and pituitary tumors) and minocycline (thyroid tumors).
- Eravacycline was not genotoxic in a standard battery of assays, including an in vitro mammalian cell mutation assay, an in vitro clastogenicity assay, and an in vivo rat bone marrow micronucleus assay.
- There are no human data on the effect of eravacycline on fertility. Eravacycline did not affect mating or fertility in male rats following intravenous administration at a dose approximating a clinical dose of 0.65 mg/kg/day (approximately 1.5 times the clinical exposure, based on AUC determined in a separate study), however, eravacycline administration at higher doses was associated with adverse reactions on male fertility and spermatogenesis that were at least partially reversible after a 70-day recovery period (1 spermatogenic cycle). Decreased sperm counts, abnormal sperm morphology, and reduced sperm motility were observed with testicular effects (impaired spermiation and sperm maturation). There were no adverse reactions on mating or fertility in female rats administered intravenous eravacycline at a dose approximating a clinical dose of 3.2 mg/kg/day (approximately 18 times the clinical exposure based on AUC determined in a separate study in unmated females).
- Decreased sperm counts and eravacycline‑related lesions noted in the testes and epididymides were seen in general toxicology studies in rats and were reversible. These findings were anticipated effects for a tetracycline-class compound.
Animal Toxicology and/or Pharmacology
- In repeated dose toxicity studies in rats, dogs and monkeys, lymphoid depletion/atrophy of lymph nodes, spleen and thymus, decreased erythrocytes, reticulocytes, leukocytes, and platelets (dog and monkey), in association with bone marrow hypocellularity, and adverse gastrointestinal effects (dog and monkey) were observed with eravacycline. These findings were reversible or partially reversible during recovery periods of 3 to 7 weeks.
- Bone discoloration, which was not fully reversible over recovery periods of up to 7 weeks, was observed in rats and monkeys after 13 weeks of dosing and in the juvenile rat study after dosing over Post-Natal Days 21-70.
- Intravenous administration of eravacycline has been associated with a histamine response in rat and dog studies.
Clinical Studies
Complicated Intra-abdominal infections in Adults
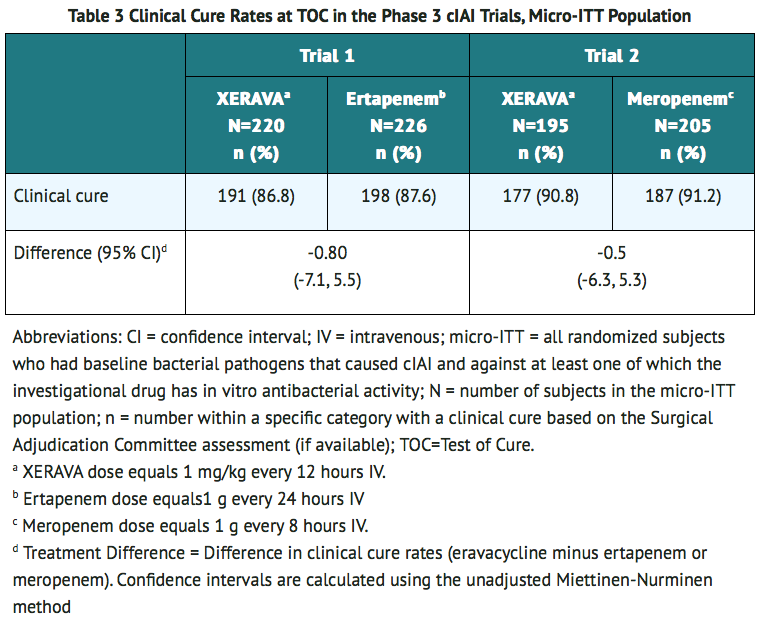
- A total of 1,041 adults hospitalized with cIAI were enrolled in two Phase 3, randomized, double-blind, active-controlled, multinational, multicenter trials (Trials 1, NCT01844856, and Trial 2, NCT02784704). These studies compared eravacycline (1 mg/kg intravenous every 12 hours) with either ertapenem (1 g every 24 hours) or meropenem (1 g every 8 hours) as the active comparator for 4 to 14 days of therapy. Complicated intra-abdominal infections included appendicitis, cholecystitis, diverticulitis, gastric/duodenal perforation, intra-abdominal abscess, perforation of intestine, and peritonitis.
- The microbiologic intent-to-treat (micro-ITT) population, which included all patients who had at least one baseline intra-abdominal pathogen, consisted of 846 patients in the two trials. Populations in Trial 1 and Trial 2 were similar. The median age was 56 years and 56% were male. The majority of patients (95%) were from Europe; 5% were from the United States. The most common primary cIAI diagnosis was intra-abdominal abscess(es), occurring in 60% of patients. Bacteremia at baseline was present in 8% of patients.
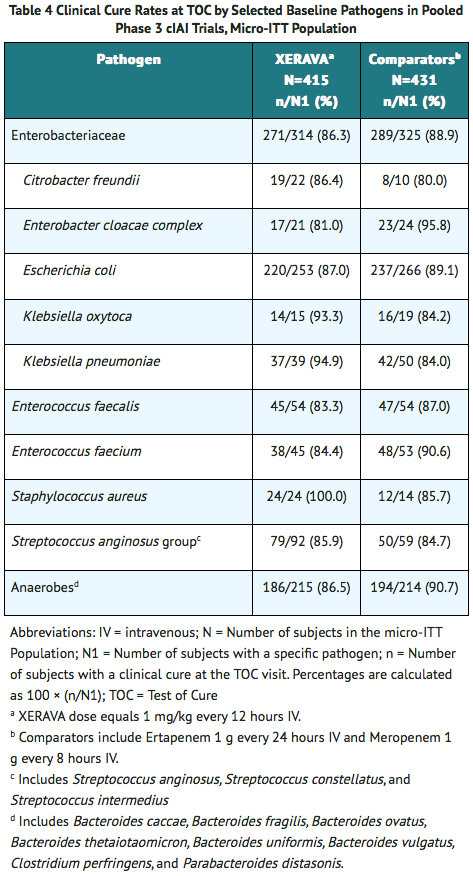
- Clinical cure was defined as complete resolution or significant improvement of signs or symptoms of the index infection at the Test of Cure (TOC) visit which occurred 25 to 31 days after randomization. Selected clinical responses were reviewed by a Surgical Adjudication Committee. Table 3 presents the clinical cure rates in the micro-ITT population. Clinical cure rates at the TOC visit for selected pathogens are presented in Table 4.
Complicated urinary tract infections (cUTI) in Adults
- Two randomized, double-blind, active-controlled, clinical trials (Trial 4, NCT01978938, and Trial 5, NCT03032510) evaluated the efficacy and safety of once-daily intravenous eravacycline for the treatment of patients with complicated urinary tract infections (cUTI). Trial 4 included an optional switch from IV to oral therapy with eravacycline. The trials did not demonstrate the efficacy of eravacycline for the combined endpoints of clinical cure and microbiological success in the microbiological intent-to-treat (micro-ITT) population at the test-of-cure visit.
How Supplied
- Eravacycline for injection, 50 mg/vial, is a yellow to orange, sterile, preservative-free powder for reconstitution in single-dose 10-mL clear glass vials with a rubber stopper and an aluminum overseal. Each vial contains 50 mg of eravacycline (equivalent to 63.5 mg of eravacycline dihydrochloride). Eravacycline is supplied in two packaging configurations:
- Single-vial carton containing one 50 mg single-dose vial
- Twelve-vial carton containing twelve 50 mg single-dose vial cartons
Storage
- Prior to reconstitution, eravacycline should be stored at 2°C to 8°C (36°F to 46°F). Keep vial in carton until use.
Images
Drug Images
{{#ask: Page Name::Eravacycline |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
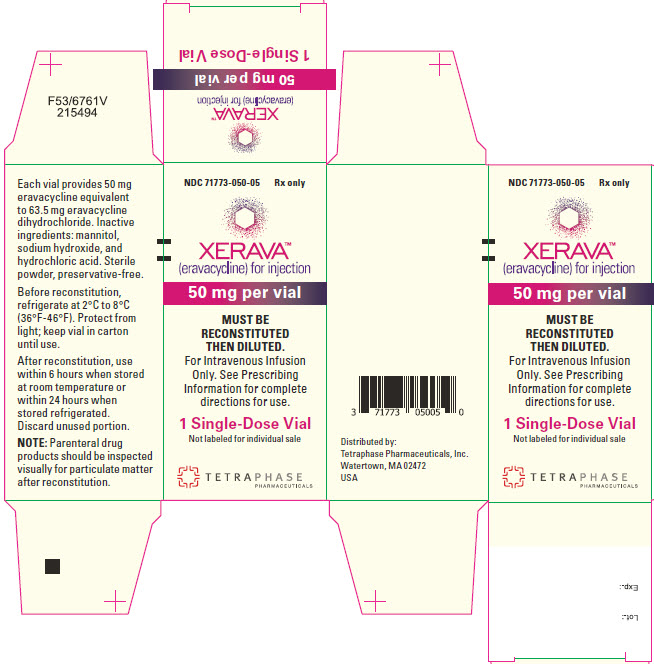
{{#ask: Label Page::Eravacycline |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Serious Allergic Reactions
- Advise patients that allergic reactions, including serious allergic reactions, could occur and that serious reactions require immediate treatment. Ask patient about any previous hypersensitivity reactions to antibacterial drugs including tetracycline or other allergens.
Tooth Discoloration and Inhibition of Bone Growth
- Advise patients that eravacycline, like other tetracycline-class drugs, may cause permanent tooth discoloration of deciduous teeth and reversible inhibition of bone growth when administered during the second and third trimesters of pregnancy. Tell your healthcare provider right away if you become pregnant during treatment.
Lactation
- Advise women not to breastfeed during treatment with eravacycline and for 4 days after the last dose.
Diarrhea
- Diarrhea is a common problem caused by antibacterial drugs, including eravacycline, which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drug, patients can develop watery and bloody stools (with or without stomach cramps and fever) which may be a sign of a more serious intestinal infection, even as late as 2 or more months after having taken the last dose of the antibacterial drug. If this occurs, instruct patients to contact their healthcare provider as soon as possible.
Tetracycline Class Adverse Reactions
- Inform patients that eravacycline is similar to tetracycline-class antibacterial drugs and may have similar adverse reactions.
Overgrowth of Non-susceptible Microorganisms
- Inform patients that antibacterial drugs including eravacycline may promote the overgrowth of non-susceptible microorganisms, including fungi.
Antibacterial Resistance
- Inform patients that antibacterial drugs including eravacycline should only be used to treat bacterial infections. They do not treat viral infections (for example, the common cold). When eravacycline is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by eravacycline or other antibacterial drugs in the future.
Precautions with Alcohol
Alcohol-Eravacycline interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Eravacycline Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.