Don Juan fracture
| Don Juan fracture | |
| ICD-10 | S42.2-S42.4 |
|---|---|
| ICD-9 | 812 |
| eMedicine | emerg/199 orthoped/271 orthoped/199 |
|
WikiDoc Resources for Don Juan fracture |
|
Articles |
|---|
|
Most recent articles on Don Juan fracture Most cited articles on Don Juan fracture |
|
Media |
|
Powerpoint slides on Don Juan fracture |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Don Juan fracture |
|
Clinical Trials |
|
Ongoing Trials on Don Juan fracture at Clinical Trials.gov Trial results on Don Juan fracture Clinical Trials on Don Juan fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Don Juan fracture NICE Guidance on Don Juan fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Don Juan fracture Discussion groups on Don Juan fracture Patient Handouts on Don Juan fracture Directions to Hospitals Treating Don Juan fracture Risk calculators and risk factors for Don Juan fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Don Juan fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
Synonyms and Keywords: Lover's fracture, Heel Bone Fracture
Overview
The calcaneus bone known as the largest tarsal bone. Meanwhile, the Lover's fracture are the involvement of the calcaneal body and may be intra-articular or extra-articular[1][2].
Historical Perspective
The name "lover's fracture" is derived from this hypothetical fact that a lover may jump from great heights while trying to escape from the lover's spouse[3].
Causes
The main etiology of the calcaneal fracture is thought to be a loading may be placed on a leg during falling or from a direct blow to the side of the hip. The main cause of calcaneal fracture is trauma. Such as the most fractures the calcaneal fracture is caused by a falling or automobile accident. Meanwhile, the normal healthy bones are extremely tough and resilient and can withstand most powerful impacts. As a person age, two factors cause higher risk of fractures[1]:
- Weaker bones
- Greater risk of falling
Stress fractures as a common causes of fractures can be found due to the repeated stresses and strains. Importantly children having more physically active lifestyles than adults, are also prone to fractures. People with any underlying diseases such as osteoporosis, infection, or a tumor affecting their bones having a higher risk of fractures. As mentioned in previous chapters, this type of fracture is known as a pathological fracture. Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures[4].
Life-threatening Causes
- There are no life-threatening causes of calcaneal fracture , however complications resulting from calcaneal fracture is common[5][6].
Common Causes
Common causes of calcaneal fracture may include:
Less Common Causes
Less common causes of calcaneal fracture include conditions that predisposes to fracture:
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | Osteoporosis and osteopenia. |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | Osteoporosis and osteopenia. |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | Falling or car accident |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
List the causes of the disease in alphabetical order[7]:
Pathophysiology
The main etiology of the calcaneal fracture is thought to thee excessive high-energy axial load to patients heel moving the the talus downward onto the calcaneus bone and causing the injury.
inversion stress to the ankle joint.
The ankle is more stable and resistant to eversion injuries than inversion injuries Because:
The medial malleolus is shorter than the lateral malleolus causing higher range of the invertion than evertion of the talus bone.
The deltoid ligament stabilized the medial wall of the ankle joint
On the other hand, the transverse malleolar, Vertical malleolar, and posterior malleolar fractures are associated with an avulsion injury, talar impaction, and other bone and/or ligamentous injury, respectively.
Mechanism
In 80% of ankle fractures the foot is in supination position while, in 20% of fractures the foot is in pronation position. The calcaneus bone fracture is caused by a falling or direct trauma to the ankle joint. The form and severity of this fracture depends on the position of the ankle joint at the moment of the trauma. The ankle joint is flexible but the medial side of the ankle joint is rigid because the medial malleolus is attached to the tibia and also the medial collateral ligaments are very strong. Also, lateral wall of the ankle include: the fibula, syndesmosis and lateral collateral ligaments play important rolls in this flexibility. This lateral wall of the ankle allows the talus to move in lateral and dorsal sides easily. The fibula has no weight-bearing roll but it provide a flexible lateral support. The syndesmosis is formed by the anterior and posterior tibiofibular ligaments which is the fibrous connection between the fibula and tibia.
If we imagine the ankle as a ring in which bones and ligaments play an important role in the maintaining the stability of this joint. Meanwhile, if this ring is broken in one place it remains stable but when it is broken in two places, the ring is unstable and it is at the higher risk of fracture. Consequently the ankle is unstable when both the medial and the lateral malleoli are fractured.
Pathophysiology
Its known that the calcaneus bone fracture in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture.
- The pattern of bone fracture and severity of injury depends on variety of factors such as:
- Patients age
- Patients Weight
- Patients past medical history specifically any bone diseases affecting the quality of bone (such as osteoporosis, malignancies)
- Energy of trauma
- Bone quality
- Position of the specific organ during the trauma
- The below-mentioned processes cause decreased bone mass density:
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Differentiating calcaneus bone fracture from other Diseases
In the orthopedic medicine its important to know that the ankle fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues.
- Acute compartment syndrome of ankle joint
- Ankle Dislocation
- Soft tissue Injury around the ankle ,
- Deep Venous thrombosis
- Thrombophlebitis
- Foot Fracture
- Gout
- Pseudogout
- Rheumatoid Arthritis
- Tibia Fracture
- Fibula Fracture
- bimalleolar fracture
- trimalleolar fracture
- triplane fracture
- Tillaux fracture
- Bosworth fracture
- pilon fracture
- Wagstaffe-Le Forte fracture
- Charcot-Marie-Tooth disease: in cases with repeated ankle fractures
Epidemiology and Demographics
- The calcaneus bone fracture accounts for 2% of all fractures and also is known as the most most frequent tarsal fracture (60% of all tarsal fractures) and including the 17% of open fractures
Risk Factors
There are different risk factors that presidpose patient for the calcaneus bone fracture that include:
- High-risk contact sports
- Higher age (elderly adults are higher prone to such fractures)
- Reduced bone density (osteoporosis)
- Direct blow
- Road / traffic accidents
- Falling
- Direct trauma to the ankle
- Taking part in any rough or high-impact sport
- Street fights, gunshot wounds, and domestic violence, may also cause the Ankle fracture
- Road traffic accidents.
Classification
Calcaneal fractures is divided into two sub-types depending involvement of the subtalar joint
Extra-articular: 25-30%
- Anterior calcaneal process fracture
- calcaneal tuberosity avulsion fracture
Extra-articular body fracture
- lover's fracture
- medial sustentaculum
Intra-articular: 70-75%
- intra-articular body fracture
As another classification method there are two common classifications as:
The Ankle fracture may be classified based on the exact location of fracturePMC4908218:
The Sanders classification is used for the intraarticular calcaneal fractures evaluations affecting the posterior facet of the calcaneus.
This Sanders classification is based on the number and location of the intraarticular fractures using the semicoronal CT images as follow:
The Regazzoni classification is used for the intraarticular calcaneal fractures evaluations affecting the posterior facet of the calcaneus[5].
This Regazzoni classification is based on the number and location of the intraarticular fractures using the semicoronal CT images as follow:
The Regazzoni classification differs from other CT based classifications because it evaluates intra-articular fractures, extra-articular fractures and the calcaneocuboid joint. Therefore, it is more accurate in detecting the lesions.
| Main Group | subgroups according to fracture severity |
|---|---|
| Type A: Peripheral fractures | A1: extra-articular |
| A2: avulsion fractures of the sustentaculum | |
| A3: fractures of the anterior process | |
| Type B, Fractures of the talocalcaneal joint | B1: posterior facet single |
| B2: posterior facet multiple | |
| B3: tarsal sinus or middle or anterior facet) | |
| Type C, Fractures of the talocalcaneal and the calcaneocuboid joints | C1: both joints single |
| C2: one joint multiple or tarsal sinus | |
| C3: both joints multiple |
Screening
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and postmenopausal and women.
Based on the US Preventive Services Task Force (USPSTF) there are three groups of patients need to be screened for the osteoporosis:
- · Men with no history of osteoporosis
- · Women with the age of 65≤ year old, with no previous history of pathological fracture due to the osteoporosis
- · Women with the age of <65 years, with 10-year fracture risk of not less than a 65-year-old white woman (who has not any other risk factor)
Accordingly women older than age of 50 are the main target for the osteoporosis screening. There is no specific recommendation to screen men for the osteoporosis.
The USPSTF recommendations from 2002 included:
Meanwhile, there are two major modalities for the osteoporosis screening:
- · Dual energy x-ray absorptiometry (DXA) of the hip and lumbar spine bones
- · Quantitative ultrasonography of the calcaneus
*It should be noted of the two above mentioned modalities for screening the ultrasonograhy is preferred to the DXA due to its lower cost, lower ionizing radiation, more availability.
After the primary evaluation of the osteoporosis, the further evaluation are required in some cases such as:
· Women with normal bone density or mild osteopenia: T-score of greater than −1.50 – should have screening for 15 years.
· Women with moderate osteopenia: T-score of −1.50 to −1.99 – should have screening for 5 years.
· Women with advanced osteopenia: T-score of −2.00 to −2.49 - should have screening for 1 year.
Natural History, Complications and Prognosis
Natural History
In cases with untreated calcaneus bone fracture the malunion and deformity of arm can be occurred.
Complications
The overall complication rate in the treatment of calcaneus bone fracture were found in around 40% of cases:
- Neurovascular compromise: such as Ulna nerve damage
- Compartment syndrome
- Chronic disability of the DRUJ
- Physeal Injury
- Malunion of the radius
- Nonunion
- Infection
- Refracture following plate removal
- Neural injury
- Instability of the DRUJ
- Loss of Motion (Stiffness)
- Posttraumatic Arthritis
- Heterotopic Ossification
Prognosis
Successful treatment of calcaneus bone fracture depends on the on-time interventions such as: accurate diagnosis and appropriate treatment and referral. Complex open fractures with soft-tissue injuries have a worse prognosis than isolated closed calcaneus bone fracture.
Diagnosis
The diagnosis of a calcaneus bone fracture should be confirmed using a radiographic examination.
History and Symptoms
The related signs and symptoms include:
- Deformity
- Skin lacerations
- Open fractures
- Erythema
- Edema
- Stiffness
- Decreased range of motion
- Tenderness
- Loss of function of the leg
- Difficulties in detection of pulses
- Nerve damage
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site. This injury should be confirmed using a radiographic evaluations.
Physical Examination
The related signs and symptoms include:
- Edema of the ankle
- Most of the time the edema will be a non-pitting edema
- Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of the ankle
- Bruising
- As a manifestation of internal injury to the local vessels by trauma or fractures bone
- Decrease in range of motion of the ankle
- Movement of the ankle will be painful if possible at all
- Tenderness
- Deformity
- Fractured bone deformity may be touchable in the internal side of the ankle if the fracture is displaced
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In polytrauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored.
Physical examination of patients with calcaneus bone fracture is usually remarkable for swelling, tenderness, bruises, ecchymosis, deformity and restricted range of motion of the ankle.
Appearance of the Patient
- Patients with calcaneus bone fracture usually appears normal unless the patients had a high energy trauma causing the open wound fracture.
Vital Signs
- Weak pulse may be seen when associated with polytrauma.
- Low blood pressure with normal pulse pressure may be present due to compound fracture with blood loss.
Skin
- Skin examination of patients with calcaneus bone fracture includes:
HEENT
- HEENT examination of patients with calcaneus bone fracture usually normal.
Neck
- Neck examination of patients with calcaneus bone fracture is usually normal
Lungs
- Pulmonary examination of patients with calcaneus bone fracture usually normal
Heart
- Cardiovascular examination of patients with calcaneus bone fracture usually normal
Abdomen
- Abdominal examination of patients with calcaneus bone fracture usually normal
Back
- Back examination of patients with calcaneus bone fracture usually normal
Genitourinary
- Genitourinary examination of patients with calcaneus bone fracture usually normal
Neuromuscular
- Neuromuscular examination of patients with calcaneus bone fracture is usually normal
- However, some patients may develop neuropraxia of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger.
Laboratory Findings
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the calcaneus bone fracture. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis.
Laboratory tests for the diagnosis of osteoporosis are:
- Complete blood count (CBC)
- Serum total calcium level
- Serum Ionized calcium level
- Serum phosphate level
- Serum alkaline phosphatase level
- Serum 25-(OH)-vitamin D level
X Ray
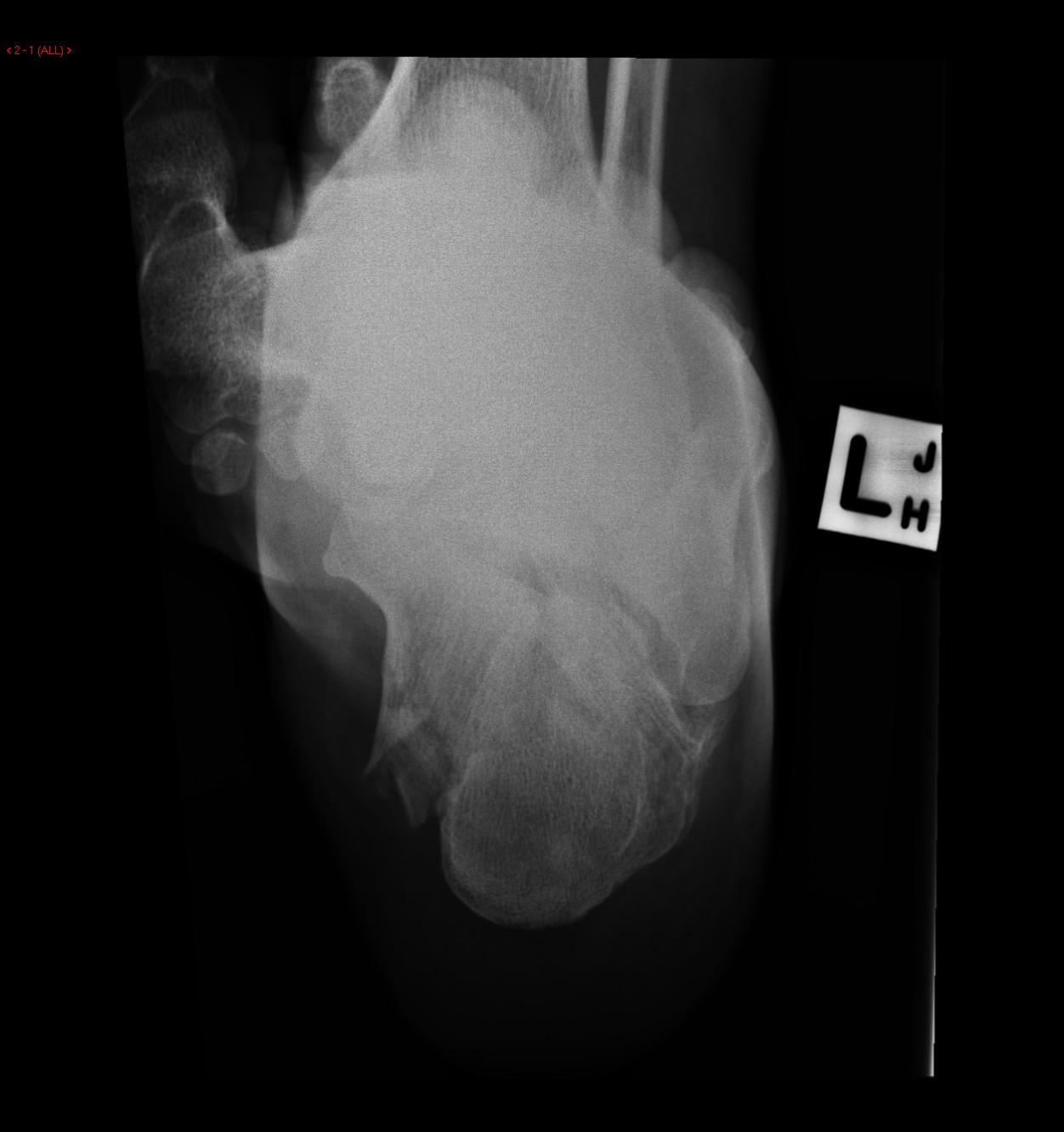
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the ankle. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the elbow and wrist joint in the radiographs of calcaneus bone fracture to ensure that the distal radioulnar joint injuries are not missed[8][9].
-
Frontal Plain films show a comminuted fracture of the left calcaneus with a flattening of Bohler's angle.
-
Lateral Plain films show a comminuted fracture of the left calcaneus with a flattening of Bohler's angle.
-
Lateral Plain films show a comminuted fracture of the left calcaneus with a flattening of Bohler's angle.
-
Frontal Plain films show a comminuted fracture of the left calcaneus with a flattening of Bohler's angle.
-
Plain films show a comminuted fracture of the left calcaneus with a flattening of Bohler's angle.
CT[10]
- CT-scan in the case of the calcaneus bone fracture is the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made.
-
Sagittal bone window Comminuted fracture of the calcaneus.
MRI
- Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely.
- MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the calcaneus bone fracture, but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated calcaneus bone fracture.
- Meanwhile, the MRI can be useful in in following mentioned evaluations:
- Evaluation of occult fractures
- Evaluation of the post-traumatic or avascular necrosis of carpal bones
- Evaluation of tendons
- Evaluation of nerve
- Evaluation of carpal tunnel syndrome
-
Small subtle non displaced fissure fracture of persistent dark signal intensity is seen traversing the anterior beak of the calcaneus bone with surrounding extensive marrow edema signal eliciting high signal at STIR WI.
-
Small subtle non displaced fissure fracture of persistent dark signal intensity is seen traversing the anterior beak of the calcaneus bone with surrounding extensive marrow edema
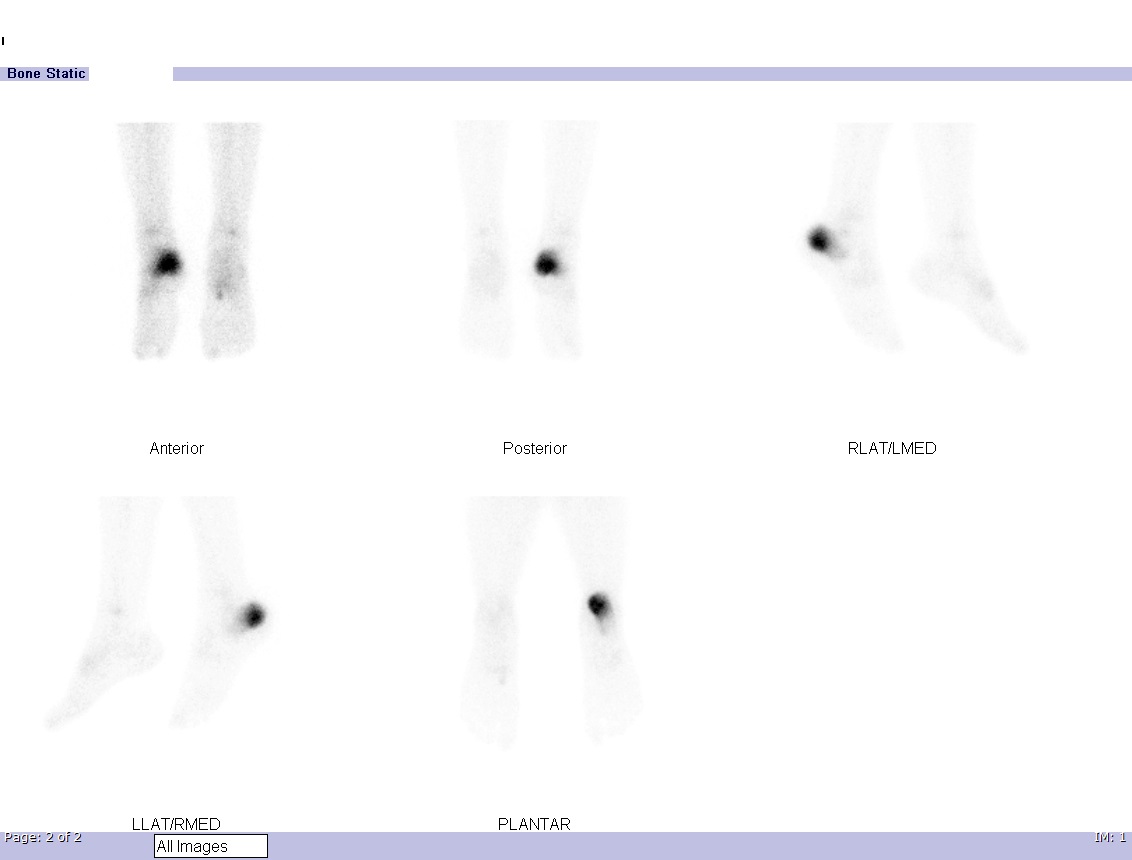
-
Dynamic flow and blood pool images show increased perfusion and vascularity at the right heel. Delayed static images show an intense increase in tracer uptake localized to the posterior aspect of the right calcaneum highly suspicious of a fracture.
-
Dynamic flow and blood pool images show increased perfusion and vascularity at the right heel. Delayed static images show an intense increase in tracer uptake localized to the posterior aspect of the right calcaneum highly suspicious of a fracture.
Other Diagnostic Studies
There are no other Diagnostic studies associated with calcaneus bone fracture[13][14]
Treatment [6]
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open ankle fractures considered as a surgical emergency. calcaneus bone fracture occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the calcaneus bone fracture. There are controversies regarding the indications for intramedullary nailing of ankle fractures[15].
- The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe.
- In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of the ankle joint. If the fracture shifts in position, it may require surgery to put the bones back together.
- Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the calcaneus bone fracture
- For all patients with calcaneus bone fracture, a post-reduction true lateral radiograph is suggested.
- Operative fixation is suggested in preference to cast fixation for fractures with post-reduction radial shortening greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm.
- Patients probably do not need to begin early wrist motion routinely after stable fracture fixation.
- Adjuvant treatment of calcaneus bone fracture with vitamin C is suggested for the prevention of disproportionate pain
- Lateral epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the supinated ankle , and the extended wrist for relaxing the extensor muscles.
Complications of Non-surgical therapy
Failure of non-surgical therapy is common:
- Re-displacement to its original position even in a cast
- Stiffness
- Post traumatic osteoarthritis leading to wrist pain and loss of function
- Other risks specific to cast treatment include:
- Compression of the swollen arm causing compartment syndrome
- Reflex sympathetic dystrophy is a serious complication
- Stiffness is universal following a prolonged period of immobilization and swelling
Returning to the normal physical activity after calcaneus bone fracture can take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult calcaneus bone fracture should be considered to be treated with open reduction and internal fixation (ORIF).
-
Post operation Calcaneal fracture
-
Post operation Calcaneal fracture
-
Post operation Calcaneal fracture
External fixation: For severe open fractures Open reduction and internal fixation: For calcaneus bone fracture which depending on each patients condition the following may be needed:
Nerve placement Bone grafting Osteotomy Arthrodesis
Operation [20]
- There are a variety of methods and implants useful to stabilize the calcaneus bone fracture, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex calcaneus bone fracture include external fixation, and open reduction and internal fixation.
External Fixation With or Without Percutaneous Pin Fixation
- Ankle spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation of bone.
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the Superficial branch of the nerve
- Complex regional pain syndrome
Open reduction and internal fixation with plates and screws [21]
- This is the most common type of surgical repair for calcaneus bone fracture
- During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment.
- The bones held together with special screws and metal plates attached to the outer surface of the bone.
Complications of open reduction and internal fixation with plates and screws =
- Infection
- Damage to nerves and blood vessels
- Synostosis
- Nonunion
Pain Management [22]
Pain after an injury or surgery is a natural part of the healing process.
Medications are often prescribed for short-term pain relief after surgery or an injury such as:
- opioids
- non-steroidal anti-inflammatory drugs (NSAIDs)
- local anesthetics
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor.
Interventions [2]
The following options can be helpful for patients to rehabilitate after their fracture :
- Joints mobilization
- compression bandage
- Soft tissue massage
- Exercises and Activity modification
Postoperative Rehabilitation [10]
- Complex calcaneus bone fracture warrant individualized immobilization and rehabilitation strategies.
- Because most multifragmentary calcaneus bone fracture are the result of high-energy injuries, a prolonged period of wrist immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The ankle is typically immobilized for 6 weeks post-operatively in a splint with Full weight bearing commences at approximately 3 months post-operatively after consolidation of the fracture is noted on radiographs.
- The presence of varying degrees of ankle stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral lower extremity fractures, or peripheral nerve injuries. Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness. Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the ankle. A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the ankle and limit the development of intrinsic muscle tightnes
Primary Prevention [22]
There are various preventive options to reduce the incidence of the calcaneus bone fracture
- Using ankle guards during practicing sports (skating, biking)
- Using ankle guards during driving motorbikes
- Avoid falls in elderly individuals
- Prevention and/or treatment of osteoporosis
- Healthy diet
Secondary Prevention
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of osteoporosis consequently these type of patients at greater risk for the pathological fractures [23][24].
So the Calcium and vitamin D supplementation play important role in increasing the bone mineral density (BMD) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive alcohol and quitting smoking play important role in this regard.
Detecting osteoporosis
- DEXA(dual-energy x-ray absorptiometry) scan
- Serum calcium and vitamin D levels
- Ultrasonography of the calcaneus
Pharmacological therapy
- The primary goal for the treatment of osteoporosis is to reduce longtime fracture risk in patients. Increasing bone mineral density (BMD) in response to the treatment is far less important than improvement of clinical aspects of osteoporosis, i.e., osteoporoticfracture. Therefore, most of the drugs efficacy is measured by the extent they improve the fracture risk instead of increasing BMD.
- During the treatment, if a single fracture happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a specialist.
- Calcium and vitamin D supplementation have been found to be effective in reducing the long term fracture risk, significantly. In order to suggest the people to use vitamin D and calcium supplements, the physician needs to make sure that patient is not able to obtain the nutrients through the daily intake. The available supplemental ions of calcium include calcium carbonate, calcium citrate, and vitamin D3 in various dosage forms.
Life style modifications
- Exercise: Exercise promotes the mineralization of bone and bone accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of osteoporosis. However, it can have a negative effect on bone mineralization in cases of poor nutrition, such as anorexia nervosa and celiac disease.
- Nutrition: A diet high in calcium and vitamin D prevents bone loss. Patients at risk for osteoporosis, such as persons with chronic steroid use are generally treated with vitamin D and calcium supplementation. In renal disease, more active forms of vitamin D, such as 1,25-dihydroxycholecalciferol or calcitriol are used; as the kidney cannot adequately generate calcitriol from calcidiol (25-hydroxycholecalciferol), which is the storage form of vitamin D.
- By quitting smoking, osteoporosis as well as other diseases can be prevented[25].
- Avoiding excessive alcohol intake or drinking only in moderation.
See also
- triplane fracture
- Tillaux fracture
- Bosworth fracture
- pilon fracture
- Wagstaffe-Le Forte fracture
- Maisonneuve Fracture
References
- ↑ 1.0 1.1 Reichel R, Monstein HJ, Jansen HW, Philipson L, Benecke BJ (May 1982). "Small nuclear RNAs are encoded in the nontranscribed region of ribosomal spacer DNA". Proc. Natl. Acad. Sci. U.S.A. 79 (10): 3106–10. doi:10.1073/pnas.79.10.3106. PMID 6179077.
- ↑ 2.0 2.1 Tomasini M, Meciani L, Sartorelli E (December 1965). "[Observations on the subject of digitalis therapy of chronic pulmonary heart disease]". Minerva Med. (in Italian). 56 (101): 4470–82. PMID 5862705.
- ↑ Lee P, Hunter TB, Taljanovic M (2004). "Musculoskeletal colloquialisms: how did we come up with these names?". Radiographics. 24 (4): 1009–27. doi:10.1148/rg.244045015. PMID 15256625.
- ↑ Fikhman BA, Sirotiuk LV, Petukhov VG (April 1966). "[Photometric analysis of bacterial suspensions. IV. On the possibility of using the osmotic effect to determine the relationship between live and dead cells in suspensions of tularemia bacteria]". Zh. Mikrobiol. Epidemiol. Immunobiol. (in Russian). 43 (4): 130–4. PMID 6004727.
- ↑ 5.0 5.1 Ventrucci M, Gullo L, Daniele C, Bartolucci C, Priori P, Platé L, Bonora G, Labò G (1983). "Comparative study of serum pancreatic isoamylase, lipase, and trypsin-like immunoreactivity in pancreatic disease". Digestion. 28 (2): 114–21. doi:10.1159/000198973. PMID 6197334.
- ↑ 6.0 6.1 6.2 Belmonte M, Scardovi C, Tabacchi G (April 1966). "[Rheographic control cerebral hemodynamic effects induced by roentgen irradiation on the cervical sympathetic system in subjects with tapeto-retinal degenerations]". Ann Ottalmol Clin Ocul (in Italian). 92 (4): 235–46. PMID 5961258.
- ↑ 7.0 7.1 Masztalerz A, Bujwidowa B, Jagielska I, Masztalerzowa Z, Potoczek J, Szczepańska H, Warych B (September 1983). "[Social class and dental and occlusal conditions]". Czas Stomatol (in Polish). 36 (9): 691–5. PMID 6584293.
- ↑ Saito Y (December 1973). "[Comparison of ACTH and insulin actions on sugar transport in their target organs]". Nihon Naibunpi Gakkai Zasshi (in Japanese). 49 (12): 1436–46. doi:10.1507/endocrine1927.49.12_1436. PMID 4359527.
- ↑ Wilesmith JW, Bode R, Pritchard DG, Stuart FA, Sayers PE (August 1986). "Tuberculosis in East Sussex. I. Outbreaks of tuberculosis in cattle herds (1964-1984)". J Hyg (Lond). 97 (1): 1–10. doi:10.1017/s0022172400064305. PMID 3734437.
- ↑ 10.0 10.1 Hopkins NF, Spinks TJ, Rhodes CG, Ranicar AS, Jamieson CW (January 1983). "Positron emission tomography in venous ulceration and liposclerosis: study of regional tissue function". Br Med J (Clin Res Ed). 286 (6362): 333–6. doi:10.1136/bmj.286.6362.333. PMID 6402087.
- ↑ Awachie JB (November 1965). "The ecology of Echinorhynchus truttae Schrank, 1788 (Acanthocephala) in a trout stream in North Wales". Parasitology. 55 (4): 747–62. PMID 5895366.
- ↑ Sieber-Blum M, Reed W, Lidov HG (October 1983). "Serotoninergic differentiation of quail neural crest cells in vitro". Dev. Biol. 99 (2): 352–9. doi:10.1016/0012-1606(83)90285-3. PMID 6352372.
- ↑ Earl RT, Hunneyball IM, Billett EE, Mayer RJ (March 1988). "Evaluation of reconstituted Sendai virus envelopes as intra-articular drug vectors: effects on normal and experimentally arthritic rabbit knee joints". J. Pharm. Pharmacol. 40 (3): 166–70. doi:10.1111/j.2042-7158.1988.tb05211.x. PMID 2899144.
- ↑ Hemindra D (1981). "[Internal resorption of the primary teeth (case report)]". J Dent Assoc Thai (in Thai). 31 (4): 176–83. PMID 6951845.
- ↑ Sharygin AA (January 1970). "[A complex study of stomach and intestinal functioning in experimental pleuropneumonia]". Biull Eksp Biol Med (in Russian). 69 (1): 40–3. PMID 5450139.
- ↑ McClure GM (September 1987). "Child and family psychiatry in China". J Am Acad Child Adolesc Psychiatry. 26 (5): 806–10. doi:10.1097/00004583-198709000-00033. PMID 3667516.
- ↑ Darmon A, Zangvill M, Cabantchik ZI (January 1983). "New approaches for the reconstitution and functional assay of membrane transport proteins. Application to the anion transporter of human erythrocytes". Biochim. Biophys. Acta. 727 (1): 77–88. doi:10.1016/0005-2736(83)90371-1. PMID 6824657.
- ↑ Dygalo NN, Markel' AL, Naumenko EV (March 1987). "[Prenatal hydrocortisone modification of the adrenocortical function of adult rats with hereditary arterial hypertension]". Biull Eksp Biol Med (in Russian). 103 (3): 287–9. PMID 3828503.
- ↑ Yamagishi M, Kanazi K, Usui T, Ishikura H, Izumi Y, Kamamoto T, Okubo T, Konishi H, Miki M, Sawada H (July 1984). "A case of myeloid metaplasia with fatty and partially fibrotic bone marrow". Nippon Ketsueki Gakkai Zasshi. 47 (4): 982–9. PMID 6507023.
- ↑ Beckmann G, Wingberg J, Hasund A (October 1983). "[Computer-assisted cephalometry using the Bergen technic]". Fortschr Kieferorthop (in German). 44 (5): 359–69. doi:10.1007/bf01994542. PMID 6583145.
- ↑ Pols J (January 1985). "[Involuntary commitment: therapy or confinement?]". Tijdschr Ziekenverpl (in Dutch; Flemish). 38 (2): 47–52. PMID 3849198.
- ↑ 22.0 22.1 Fainstein V, Bodey GP, Fekety R (June 1981). "Relapsing pseudomembranous colitis associated with cancer chemotherapy". J. Infect. Dis. 143 (6): 865. doi:10.1093/infdis/143.6.865. PMID 6166695.
- ↑ Lotte A, Hatton F, Beust M, Rozenberg M (1966). "[Statistical report on the activities of departmental centers of BCG vaccination in 1964]". Bull Inst Natl Sante Rech Med (in French). 21 (2): 389–98. PMID 5930824.
- ↑ Lopetegui R, Sosa Miatello C (1965). "[Protein components in extracts of cultured Trypanosoma cruzi (crithidias)]". Rev Soc Argent Biol (in Spanish; Castilian). 41 (5): 190–6. PMID 5888141.
- ↑ Sy M, Pilet C, Niel M, Maillet M, Goret P (1965). "[Antibacterial actions of some halogenated derivatives of m-xylenol]". Therapie (in French). 20 (4): 1071–7. PMID 5845202.