Chronic stable angina exercise electrocardiography
|
Chronic stable angina Microchapters | ||
|
Classification | ||
|---|---|---|
| ||
| ||
|
Differentiating Chronic Stable Angina from Acute Coronary Syndromes | ||
|
Diagnosis | ||
|
Alternative Therapies for Refractory Angina | ||
|
Discharge Care | ||
|
Guidelines for Asymptomatic Patients | ||
|
Case Studies | ||
|
Chronic stable angina exercise electrocardiography On the Web | ||
|
Chronic stable angina exercise electrocardiography in the news | ||
|
to Hospitals Treating Chronic stable angina exercise electrocardiography | ||
|
Risk calculators and risk factors for Chronic stable angina exercise electrocardiography | ||
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Smita Kohli, M.D.; Lakshmi Gopalakrishnan, M.B.B.S.; Aysha Anwar, M.B.B.S[3]
Overview
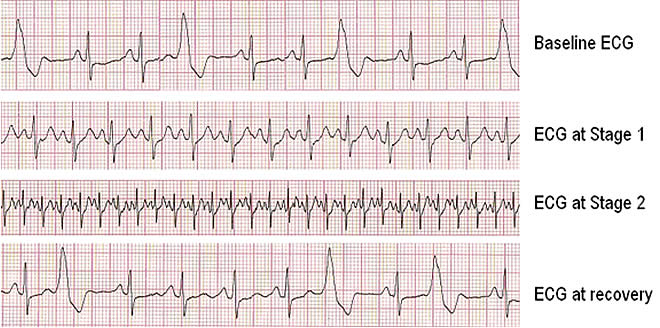
In patients with chronic stable angina, exercise ECG is more sensitive and specific to identify inducible ischemia and to diagnose coronary artery disease.[1] ECG abnormalities associated with MI include: down sloping of ST-segment depression or elevation, accompanying angina that occurs at a low workload during early stages of exercise and persistent for more than 3-minutes after exercise. The reliability of diagnosis is shown to improve with the evaluation of ST changes in relation to heart rate.[2] Bruce protocol or treadmill (expressed in terms of METs) or bicycle ergometer (expressed in terms of watts) are used to detect MI. Exercise ECG test must be terminated on the achievement of maximal predicted heart rate and/or if the patient becomes symptomatic or develops pain with significant ST-segment changes. Exercise ECG test also provides prognostic stratification to evaluate the response to medical therapy or revascularization.[3]
Exercise Electrocardiography
Indications
An exercise ECG is more useful than the resting ECG in detecting myocardial ischemia and evaluating the cause of chest pain.
Diagnostic Criteria
ST-segment changes suggestive of coronary artery disease include:
- Down sloping or horizontal ST segment depressions are highly suggestive of myocardial ischemia, particularly when:
- It occurs at a low workload,
- It occurs during early stages of exercise,
- It persists for more than 3 minutes after exercise, or
- It is accompanied by chest discomfort that is compatible with angina.
- In converse, up-sloping ST segments are much less specific indicators of coronary artery disease.
Sensitivity and Specificity
- Exercise electrocardiography has a sensitivity of approximately 70% for detecting coronary artery disease.
- Exercise electrocardiography has a specificity of approximately 75% for excluding coronary artery disease.
- To assess the probability of coronary artery disease in an individual patient, the exercise ECG result must be integrated with the clinical presentation.
- Conditions that increase the probability of exercise ECG yielding false positive results are:
- An abnormal resting ECG associated with left ventricular hypertrophy, intraventricular conduction abnormalities, pre-excitation syndromes (Long Ganong Lewine Syndrome = LGL, Wolf-Parkinson-White syndrome = WPW and Mahaim type), electrolyte imbalance or therapy with digitalis
- In women, the lower prior probability of CAD is associated with more false positive results on ECG.
- On the other hand, a fall in systolic pressure of 10 mm Hg or more during exercise or the appearance of a murmur of mitral regurgitation during exercise increases the probability that, an abnormal stress ECG is a true positive test result.
Treadmill Exercise Test
- Treadmill exercise test is more preferable to bicycle exercise test (or ergometer) for detecting myocardial ischemia.
- In patients who cannot perform treadmill exercise, pharmacologic stress scintigraphy or echocardiography is preferable to upper body arm exercise.
- Variables of the Treadmill Exercise Test which indicate the high risk are:
- Short exercise duration less than 5 METs,
- Significant ST segment depression (magnitude ≥2 mm, starts at exercise stage I or II, duration of exercise test is <5 minutes and ≥5 leads with ST changes,
- Significant changes in blood pressure: low peak systolic blood pressure (<130 mm Hg), significant decrease in systolic blood pressure during the test (below the resting standing blood pressure),
- Inability to attain to the target heart rate,
- Presence of exercise induced angina,
- Presence of frequent ventricular ectopy (e.g. couplets or tachycardia) at low workload.
For more information on exercise EKG during exercise stress testing, click here.
ACC/AHA/ACP–ASIM Guidelines for the Management of Patients With Chronic Stable Angina (DO NOT EDIT)[4]
Stress Testing and Advanced Imaging for Initial Diagnosis in Patients With Suspected SIHD Who Require Noninvasive Testing[4](DO NOT EDIT)
Patients able to exercise
| Class I |
| "1. Standard exercise ECG testing is recommended for patients with an intermediate pretest probability of IHD who have an interpretable ECG and at least moderate physical functioning or no disabling comorbidity(Level of Evidence: A)" |
| Class IIa |
| "1. For patients with a low pretest probability of obstructive IHD who do require testing, standard exercise ECG testing can be useful, provided the patient has an interpretable ECG and at least moderate physical functioning or no disabling comorbidity. (Level of Evidence: C)" |
Patients unable to exercise
| Class III |
| "1. Standard exercise ECG testing is not recommended for patients who have an uninterpretable ECG or are incapable of at least moderate physical functioning or have disabling comorbidity. (Level of Evidence: C)" |
ESC Guidelines- Exercise ECG for Initial Diagnostic Assessment of Angina (DO NOT EDIT)[5]
| Class I |
| "1. Patients with symptoms of angina and intermediate pre-test probability of coronary artery disease based on age, gender, and symptoms, unless unable to exercise or displays ECG changes which make ECG non-evaluable. (Level of Evidence: B)" |
| Class IIb |
| "1. Patients with more than 1 mm ST-depression on resting ECG or taking digoxin. (Level of Evidence: B)" |
| "1. In patients with low pre-test probability (less than 10% probability) of coronary disease based on age, gender, and symptoms. (Level of Evidence: B)" |
ESC Guidelines- Exercise ECG for Routine Re-assessment in Patients with Chronic Stable Angina (DO NOT EDIT)[5]
| Class IIb |
| "1. Routine periodic exercise ECG in the absence of clinical change. (Level of Evidence: C)" |
References
- ↑ Ashley EA, Myers J, Froelicher V (2000) Exercise testing in clinical medicine. Lancet 356 (9241):1592-7. DOI:10.1016/S0140-6736(00)03138-X PMID: 11075788
- ↑ Elamin MS, Boyle R, Kardash MM, Smith DR, Stoker JB, Whitaker W et al. (1982) Accurate detection of coronary heart disease by new exercise test. Br Heart J 48 (4):311-20. PMID: 6127094
- ↑ Mark DB, Shaw L, Harrell FE, Hlatky MA, Lee KL, Bengtson JR et al. (1991) Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med 325 (12):849-53. DOI:10.1056/NEJM199109193251204 PMID: 1875969
- ↑ 4.0 4.1 Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP; et al. (2012). "2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 126 (25): 3097–137. doi:10.1161/CIR.0b013e3182776f83. PMID 23166210.
- ↑ 5.0 5.1 Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F; et al. (2006). "Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology". Eur Heart J. 27 (11): 1341–81. doi:10.1093/eurheartj/ehl001. PMID 16735367.