Cardiac amyloidosis MRI
|
Cardiac amyloidosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac amyloidosis MRI On the Web |
|
American Roentgen Ray Society Images of Cardiac amyloidosis MRI |
|
Risk calculators and risk factors for Cardiac amyloidosis MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mandana Chitsazan, M.D. [2] Raviteja Guddeti, M.B.B.S. [3]; Aarti Narayan, M.B.B.S [4]
Overview
Amyloidosis is an infiltrative disease resulting in deposition of amyloid in the extracellular spaces of the tissues. Amyloid infiltration of the heart leads to expansion of these extracellular spaces resulting in retainment of gadolinium dye during cardiac magnetic resonance imaging. This retainment of gadolinium leads to signal enhancement in the late washout phase during delayed enhanced cardiac imaging.
Cardiac MRI
- Cardiovascular magnetic resonance imaging (CMR) is emerging as a promising tool in the assessment of patients with cardiac amyloidosis (CA).
- Morphological abnormalities, including:
- Thickening of ventricular and atrial walls and valvular leaflets due to deposition of amyloid fibrils
- Normal or reduced ventricular sizes
- Enlarged atria caused by diastolic dysfunction and/or valvular dysfunction due to amyloid deposition
- Functional abnormalities, including:
- Parameters of diastolic dysfunction characterized by:
- Abnormal relaxation
- Restrictive inflow physiology
- Measures of systolic function (i.e., ejection fraction) are only impaired late in the disease course
- Parameters of diastolic dysfunction characterized by:
- Tissue characterization:
- Increased intrinsic signal of the myocardium:
- T1-T2-weighted imaging sequences
- Late gadolinium enhancement (LGE)
- The cornerstone technique for the diagnosis of CA.
- Traditional LGE imaging techniques require an operator-determined null point (i. e., the inversion recovery time at which the normal myocardium appears black or “nulled”).
- Difficulty nulling the myocardium or myocardial nulling before the blood pool (on TI scout sequence) is strongly suggestive of CA with 100% sensitivity.
- LGE imaging has become less operator-dependent after the development of a phase-sensitive inversion recovery sequence.
- LGE is more common in ATTR than AL CA.
- LGE cannot distinguish between subtypes of CA.
- A major limitation of LGE is that it is not easily quantifiable.
- Features of LGE in CA:
- Global subendocardial enhancement
- Transmural LGE
- A focal, patchy LGE (to a lesser degree)
- T1 mapping (pre- and/or post-contrast)
- T1 mapping measures the T1 signal of each pixel and/or voxel in an image.
- Areas of amyloid deposition demonstrate higher native T1 values compared to normal tissues.
- Native T1 values represent a combined signal from myocyte and extracellular space and can show changes in either or both of these two compartments.
- Native T1 can be helpful in patients with contraindications to gadolinium.
- T1 mapping can potentially detect amyloid deposition earlier in the disease course than LGE.
- Major limitation of native T1 is the lack of reproducibility for various scanners or magnetic field strengths (1.5-T vs. 3.0-T).
- Post-contrast T1 mapping is performed following gadolinium administration.
- ECV (expanded extracellular volume) imaging
- Characterizes the extracellular space
- Performed following gadolinium administration
- ECV is more reproducible than absolute T1 values.
- The ECV values are markedly increased in CA, though cannot distinguish between the subtypes of CA.
- Increased intrinsic signal of the myocardium:
- However, CMR might be limited in patients with
- Atrial fibrillation
- Severe renal disease (due to contraindications to gadolinium use)
- Non-compatible intracardiac devices
- Limited patients’ cooperation to repeatedly hold their breaths
ACC/AHA Guidelines- ACCF/ACR/AHA/NASCI/SCMR 2010 Expert Consensus Document on Cardiovascular Magnetic Resonance[1] (DO NOT EDIT)
| “ |
CMR may be used for assessment of patients with LV dysfunction or hypertrophy or suspected forms of cardiac injury not related to ischemic heart disease. When the diagnosis is unclear, CMR may be considered to identify the etiology of cardiac dysfunction in patients presenting with heart failure, including
|
” |
Images
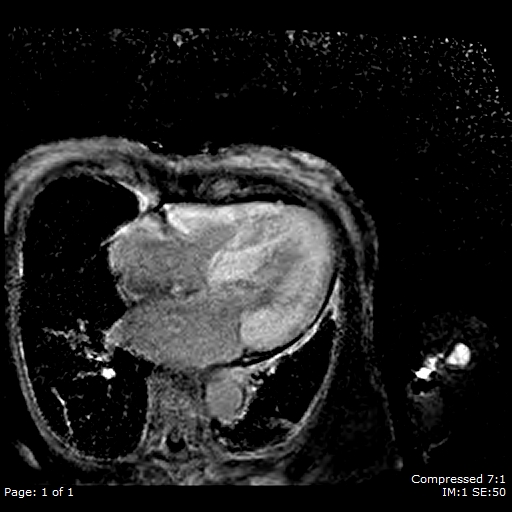
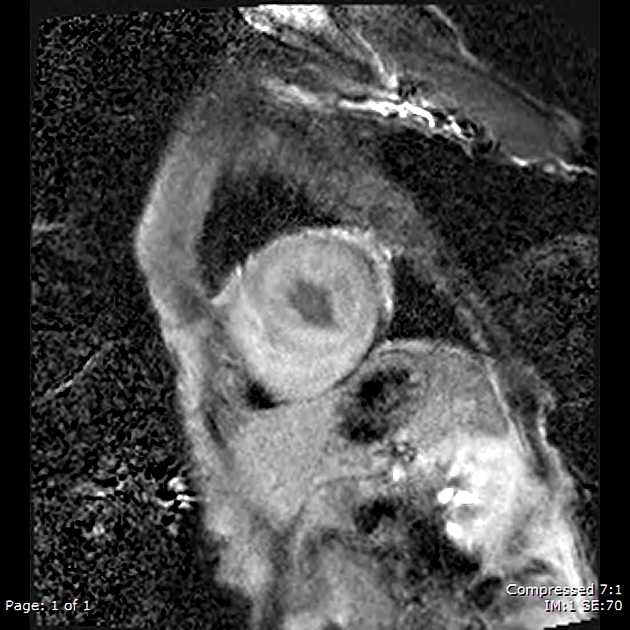
CMR images characterizing: markedly increased wall thickness; asymmetrically increased LV wall thickness with septal, basal, and mid-cavity thickening; mildly impaired LV systolic function; and moderately dilated left atrium.
File:Apical 4chamber CMR-CA.mp4
File:Short axis apical CMR-CA.mp4
File:Short axis Basal CMR-CA.mp4
File:Short-axis mid-Cavitary.mp4
Late gadolinium enhancement (LGE) images characterizing: abnormal coincident nulling of the blood pool and myocardium; diffuse transmural late gadolinium enhancement of the LV, RV, and right atrium; and rapid clearance of gadolinium from the blood pool.

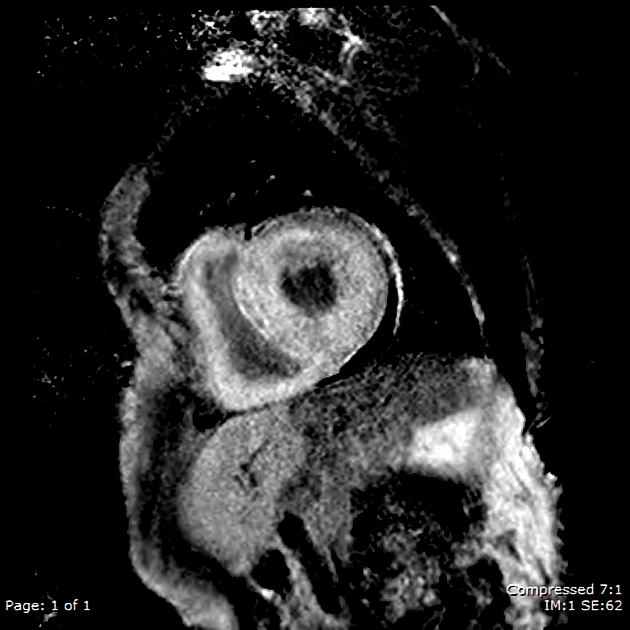
File:Short axis Mid T1 scout.mp4
References
- ↑ American College of Cardiology Foundation Task Force on Expert Consensus Documents. Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA; et al. (2010). "ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents". Circulation. 121 (22): 2462–508. doi:10.1161/CIR.0b013e3181d44a8f. PMC 3034132. PMID 20479157.
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>
- ↑ Case courtesy of Dr Ben Hudson, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/62017">rID: 62017</a>